Abstract
Purpose:
To investigate therapeutic outcome of dose escalation ≥ 80 Gy in nonresected non-small cell lung cancer (NSCLC).
Patients and Methods:
124 consecutive patients with histologically/cytologically proven NSCLC were enrolled. Tumor stage I, II, IIIA, and IIIB was diagnosed in 30, eight, 39, and 47 patients, respectively. 38 patients (31%) had weight loss > 5% during the 3 months before diagnosis. A median dose of 88.2 Gy (range 80.0–96.0 Gy), 69.3 Gy (63.0–88.0 Gy) and 56.7 Gy was applied to primary lesions, involved lymph nodes, and elective nodes (within a region of about 6 cm cranial to macroscopically involved nodes), respectively. Daily fractional ICRU doses of 2.0–2.2 Gy were delivered by the conformal target-splitting technique. 58 patients (47%) received induction chemotherapy, in median two cycles prior to radiotherapy.
Results:
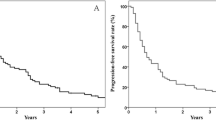
Median follow-up time of all patients was 19 months, of patients alive 72.4 months (69–121 months). The cumulative actual overall survival rate at 2 and 5 years amounts to 39% and 11.3%, respectively, resulting in a median overall survival time of 19.6 months. According to stages I, II, IIIA, and IIIB, the median overall survival times are 31.8, 31.4, 19.0, and 14.5 months, respectively. The locoregional tumor control rate at 2 years is 49%. Apart from one treatment-related death (pneumonitis), acute toxicity according to EORTC/RTOG scores was moderate: lung grade 2 (n = 7), grade 3 (n = 3); esophagus grade 1 (n = 11); heart grade 3 (n = 1, pericarditis). No late toxicity grade > 1 has been observed.
Conclusion:
Sequential, conventionally fractionated high-dose radiotherapy by conformal target splitting is well tolerated. The results for survival and locoregional tumor control seem to at least equalize the outcome of simultaneous chemoradiation approaches, which, at present, are considered “state of the art” for patients with nonresected NSCLC. A higher potential of radiation therapy might be reached by accelerated fractionation regimens.
Zusammenfassung
Ziel:
Evaluierung der Behandlung mit Dosen ≥ 80 Gy bei nichtoperierter Patienten mit nichtkleinzelligem Bronchialkarzinom (NSCLC).
Patienten und Methodik:
124 konsekutiv zugewiesene Patienten mit histologisch/zytologisch verifiziertem NSCLC wurden untersucht (Tabelle 1). Ein Tumorstadium I, II, IIIA und IIIB lag bei 30, acht, 39 bzw. 47 Patienten vor. Bei 38 Patienten (31%) zeigte sich ein Gewichtsverlust > 5% in den 3 Monaten vor Diagnosestellung. Primartumoren wurden im Mittel mit 88,2 Gy (Bandbreite 80,0–96,0 Gy), makroskopisch befallene Lymphknoten mit 69,3 Gy (63,0–88,0 Gy) und elektive Lymphknotenstationen (Region von etwa 6 cm kranial der makroskopisch befallenen Lymphknoten) mit 56,7 Gy behandelt (Tabelle 2). ICRU-Einzeldosen von 2,0–2,2 Gy wurden mit der konformalen „target-splitting“-Technik appliziert. 58 Patienten (47%) erhielten zwei Zyklen einer Induktionschemotherapie.
Ergebnisse:
Die noch lebenden Patienten wurden im Mittel 72,4 Monate nachbeobachtet (69–121 Monate). Die kumulativen 2- und 5-Jahres-Überlebensraten betragen 39% bzw. 11,3% bei einer medianen Überlebenszeit (ULZ) von 19,6 Monaten. Bezogen auf die Tumorstadien I, II, IIIA bzw. IIIB beträgt die mediane Überlebenszeit 31,8, 31,4, 19,0 bzw. 14,5 Monate. Die lokoregionare 2-Jahres-Tumorkontrollrate liegt bei 49%. Ein Patient verstarb infolge einer Pneumonitis, ansonsten war die Toxizitat gemessen an den EORTC/RTOG-Scoring-Kriterien moderat: Pneumonitis Grad 2 (n = 7), Grad 3 (n = 3); Osophagus Grad 1 (n = 11); Herz Grad 3 (n = 1, Perikarditis; Tabelle 3). Bei keinem Patienten trat eine Spattoxizitat > Grad 1 auf.
Schlussfolgerung:
Eine sequentielle, konventionell fraktionierte, hochdosierte Bestrahlung mittels „target-splitting“-Technik zeigt eine geringe Morbiditat. Die Ergebnisse bezüglich Überlebenszeit und lokaler Tumorkontrolle erscheinen gegenüber den Resultaten der simultanen Chemo-/Radiotherapie, die derzeit als „state of the art“ angesehen wird, zumindest als ebenbürtig (Tabelle 4). Eine weitere Steigerung des strahlentherapeutischen Potentials durfte mit akzelerierten Fraktionierungsschemata moglich sein.
Similar content being viewed by others
References
Alvarez Moret J, Kolbl O, Bogner L. Quasi-IMAT study with conventional equipment to show high plan quality with a single gantry arc. Strahlenther Onkol 2009;185:41–8
Auperin A, Le Pechoux C, Rolland E, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small cell lung cancer. J Clin Oncol 2010;28:2181–90
Belderbos J, Heemsbergen W, De Jaeger K, et al. Final results of a phase I/II dose escalation trial in non-small lung cancer using three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:126–34
Bradley J, Bae K, Graham M, et al. Primary analysis of the phase II component of a phase I/II dose intensification study using three-dimensional conformal radiation therapy and concurrent chemotherapy for patients with inoperable non-small cell lung cancer: RTOG 0117. J Clin Oncol 2010;28:2475–80
Bradley J, Graham M, Winter K, et al. Toxicity and outcome results of RTOG 9311: a phase I–II dose escalation study using three-dimensional conformal radiotherapy in patients with inoperable non-small cell lung carcinoma. Int J Radiat Oncol Biol Phys 2005;61:318–28
Cox JD, Pajak T, Asbell S, et al. Interruptions of high-dose radiation therapy decrease long-term survival of favorable patients with unresectable non-small cell lung cancer of the lung: analysis of 1244 cases from 3 Radiation Therapy Oncology Group (RTOG) trials. Int J Radiat Oncol Biol Phys 1993;27:493–8
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341–6
Curran WJ, Scott C, Langer C, et al. Phase III comparison of sequential versus concurrent chemoradiation for patients with unresected stage III non-small cell lung cancer. Initial report of RTOG 9410. Proc Am Soc Clin Oncol 2003;22:621.abstract 2499
Deutschmann H, Steininger P, Nairz O, et al. „Augmented reality“ in conventional simulation by projection of 3-D structures into 2-D images. Strahlenther Onkol 2008;184:93–9
Dillman RO, Seagren SL, Propert KJ, et al. A randomized trial of induction chemotherapy plus high-dose radiation versus radiation alone in stage III non-small lung cancer. N Engl J Med 1990;323:940–5
Dziadziuszko R. Stage III: combined treatment – sequential. J Thorac Oncol 2010;5.Suppl:S17
Fournel P, Robinet G, Thomas P, et al. Randomized phase III trial of sequential chemoradiotherapy compared with concurrent chemoradiotherapy in locally advanced non-small cell lung cancer: Groupe Lyon-Saint Etienne d’Oncologie Thoracique – Groupe Francais de Pneumo-Cancerologie NPC 95-01 study. J Clin Oncol 2005;23:5910–7
Fowler J. Biological factors influencing optimum fractionation in radiation therapy. Acta Oncol 2001;40:712–7
Furuse K, Fukuoka M, Kawahara M, et al. Phase III study of concurrent versus sequential thoracic radiation therapy in combination with mitomycin, vindesine, and cisplatin in unresectable stage III non-small cell lung cancer. J Clin Oncol 1999;17:2692–9
Hanna N, Neubauer M, Yiannoutsos C, et al. Phase III trial of cisplatin, etoposide, and concurrent chest radiation with or without consolidation docetaxel in patients with inoperable stage III non-small cell lung cancer: The Hoosier Oncology Group and US Oncology. J Clin Oncol 2008;26:5755–60
Hayman J, Martel M, Ten Haken R, et al. Dose escalation in non-small cell lung cancer using three-dimensional conformal radiation therapy: update of a phase I trial. J Clin Oncol 2001;19:127–36
Jeremic B, Koning C. Induction chemotherapy before chemoradiation in locally advanced non-small cell lung cancer: failure after failure, again and again. J Clin Oncol 2008;26:e1–2
Kong FM, Ten Haken RK, Schipper MJ, et al. High-dose radiation improved local tumor control and overall survival in patients with inoperable/unresectable non-small cell lung cancer: long-term results of a radiation dose escalation study. Int J Radiat Oncol Biol Phys 2005;63:324–33
Machtay M, Hsu C, Komaki R, et al. Effect of overall treatment time on outcomes after concurrent chemoradiation for locally advanced non-small cell lung carcinoma: analysis of the Radiation Therapy Oncology Group (RTOG) experience. Int J Radiat Oncol Biol Phys 2005;63:667–71
Nairz O, Merz F, Deutschmann H, et al. A strategy for the use of image-guided radiotherapy (IGRT) on linear accelerators and its impact on treatment margins for prostate cancer patients. Strahlenther Onkol 2008;184:663–7
Rengan R, Rosenzweig K, Venkatraman E, et al. Improved local control with higher doses of radiation in large-volume stage III non-small cell lung cancer. Int J Radiat Oncol Biol Phys 2004;60:741–7
Rosenzweig KE, Fox JL, Yorke E, et al. Results of a phase I dose-escalation study using three-dimensional conformal radiotherapy in the treatment of inoperable non-small cell lung carcinoma. Cancer 2005;103:2118–27
Socinsky M, Morris D, Halle J, et al. Induction and concurrent chemotherapy with high-dose thoracic conformal radiation therapy in unresectable stage IIIA and IIIB non-small cell lung cancer: a dose-escalation phase I trial. J Clin Oncol 2004;22:4341–50
Sterzing F, Schubert K, Sroka-Perez G, et al. Helical tomotherapy. Experiences of the first 150 patients in Heidelberg. Strahlenther Onkol 2008;184:8–14
Stinchcombe T, Morris D, Lee C, et al. Induction chemotherapy with carboplatin, irinotecan, and paclitaxel followed by high-dose three-dimension conformal thoracic radiotherapy (74 Gy) with concurrent carboplatin, paclitaxel, and gefitinib in unresectable stgae IIIA and stage IIIB non-small cell lung cancer. J Thorac Oncol 2008;3:250–7
Wang C, Nakayama H, Sugahara S, et al. Comparisons of dose-volume histograms for proton-beam versus conformal X-ray therapy in patients with stage I non-small lung cancer. Strahlenther Onkol 2009;185:231–4
Wurstbauer K, Deutschmann H, Kopp P, et al. NSCLC: primary tumor size – radiation dose-related accelerated, twice daily radiotherapy by target splitting, preceded by two cycles of chemotherapy – first results of a prospective study. Strahlenther Onkol 2007;183:Suppl 2:36–8
Wurstbauer K, Deutschmann H, Kopp P, et al. NSCLC: nonresected NSCLC: primary tumor size – radiation dose-related accelerated, twice daily radiotherapy, preceded by two cycles of chemotherapy: up-date of a prospective study. J Thorac Oncol 2009;4:Suppl 1:S958
Wurstbauer K, Deutschmann H, Kopp P, et al. Target splitting in radiation therapy for lung cancer: further developments and exemplary treatment plans. Radiat Oncol 2009;4:30
Wurstbauer K, Deutschmann H, Kopp P, et al. Nonresected non-small cell lung cancer in stages I through IIIB: accelerated, twice daily, high-dose radiotherapy – a prospective phase I/II trial with long-term follow-up. Int J Radiat Oncol Biol Phys 2010;77:1345–51
Wurstbauer K, Deutschmann H, Kopp P, Sedlmayer F. Radiotherapy planning for lung cancer: slow CTs allow the drawing of tighter margins. Radiother Oncol 2005;75:165–70
Wurstbauer K, Deutschmann H, Kranzinger M, et al. Radiotherapy for lung cancer: target splitting by asymmetric collimation enables reduction of radiation doses to normal tissues and dose escalation. Int J Radiat Oncol Biol Phys 1999;44:333–41
Wurstbauer K, Merz F, Sedlmayer F. Amphotericin B lozengers: prophylaxis for esophagitis in thoracic radiotherapy. Strahlenther Onkol 2009;185:512–6
Youlden D, Cramb S, Baade P. The international epidemiology of lung cancer. Geographical distribution and secular trends. J Thorac Oncol 2008;3:819–31
Zatloukal P, Petruzelka L, Zemanova M, et al. Concurrent versus sequential chemoradiotherapy with cisplatin and vinorelbine in locally avanced non-small cell lung cancer: a randomized study. Lung Cancer 2004;46:87–98
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wurstbauer, K., Weise, H., Deutschmann, H. et al. Non-Small Cell Lung Cancer in Stages I–IIIB. Strahlenther Onkol 186, 551–557 (2010). https://doi.org/10.1007/s00066-010-2108-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2108-3