Abstract
Purpose:
To retrospectively analyze patient characteristics, treatment, and treatment outcome of pediatric patients with hematologic diseases treated with total body irradiation (TBI) between 1978 and 2006.
Patients and Methods:
32 pediatric patients were referred to the Department of Radiation-Oncology at the University of Zurich for TBI. Records of regular follow-up of 28 patients were available for review. Patient characteristics as well as treatment outcome regarding local control and overall survival were assessed. A total of 18 patients suffered from acute lymphoblastic leukemia (ALL), 5 from acute and 2 from chronic myelogenous leukemia, 1 from non-Hodgkin lymphoma, and 2 from anaplastic anemia. The cohort consisted of 15 patients referred after first remission and 13 patients with relapsed leukemia. Mean follow-up was 34 months (2–196 months) with 15 patients alive at the time of last follow-up. Eight patients died of recurrent disease, 1 of graft vs. host reaction, 2 of sepsis, and 2 patients died of a secondary malignancy.
Results:
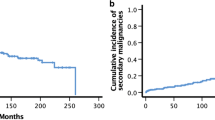
The 5-year overall survival rate (OS) was 60%. Overall survival was significantly inferior in patients treated after relapse compared to those treated for newly diagnosed leukemia (24% versus 74%; p=0.004). At the time of last follow-up, 11 patients survived for more than 36 months following TBI. Late effects (RTOG ≥3) were pneumonitis in 1 patient, chronic bronchitis in 1 patient, cardiomyopathy in 2 patients, severe cataractogenesis in 1 patient (48 months after TBI with 10 Gy in a single dose) and secondary malignancies in 2 patients (36 and 190 months after TBI). Growth disturbances were observed in all patients treated prepubertally. In 2 patients with identical twins treated at ages 2 and 7, a loss of 8% in final height of the treated twin was observed.
Conclusion:
As severe late sequelae after TBI, we observed 2 secondary malignancies in 11 patients who survived in excess of 36 months. However, long-term morbidity is moderate following treatment with the fractionated TBI at the low-dose rate that was generally used here. Conditioning for bone marrow transplantation without radiation is an attractive option, but is not sufficiently effective to completely replace TBI for the most common pediatric indications.
Zusammenfassung
Ziel:
Retrospektive Analyse von Patientencharakteristika, Behandlung und Ergebnis bei Kindern mit hämatologischen Erkrankungen, die zwischen 1978 und 2006 mit Ganzkörperbestrahlung behandelt wurden.
Patienten und Methodik:
32 Kinder wurden unserer Klinik zur TBI zugewiesen, 28 Krankengeschichten waren zugänglich (n=28). 18 Patienten litten unter akuter lymphoblastischer Leukämie (ALL), 5 unter akuter (AML) und 2 unter chronisch myeloischer Leukämie (CML), einer unter Non-Hodgkin-Lymphom und zwei unter aplastischer Anämie. 15 Patienten wurden nach erster Remission zugewiesen, 13 mit Rezidiv. Bei der letzten Kontrolle lebten noch 15 Patienten (mean 34 Monate (2–196 Monate). Acht Patienten sind an einem Rezidiv verstorben, einer an einer Graft-versus-host Erkrankung, zwei an Sepsis und zwei an Sekundärtumoren.
Resultate:
Das 5-Jahres Gesamtüberleben lag bei 60%. Das Gesamtüberleben war signifikant (p=0.004) niedriger bei Patienten, die nach einem Rezidiv behandelt wurden (24%), als bei solchen die bei Erstdiagnose behandelt wurden (74%). Spättoxizität RTOG ≥3 waren eine Pneumonitis bei 1 Patienten, eine chronische Bronchitis bei einem Patienten, Kardiomyopathie bei 2 Patienten, eine Katarakt bei einem Patienten (48 Monate nach TBI mit 10Gy Einzeldosis) und Sekundärtumore bei 2 Patienten. Wachstumsstörungen mit einer Körpergrösse kleiner als die 25. Perzentile zeigten sich bei allen vor der Pubertät behandelten Kindern. Bei zwei eineiigen Zwillingen zeigt sich ein Verlust von 8% an Körpergrösse im Vergleich zum Zwilling.
Schlussfolgerung:
Wie erwartet zeigen sich schwere Spättoxizitäten nach Ganzkörperbestrahlung mit zwei Sekundärtumoren bei 11 Patienten, die länger als 36 Monate überlebt haben. Aber die Morbidität ist mässig nach fraktionierter Ganzkörperbestrahlung und der hier in fast allen Fällen verwendeten niedrigen Dosisrate. Konditionierung ohne TBI ist eine attraktive Möglichkeit, aber noch nicht effektiv genug um die TBI im Kindesalter ganz zu ersetzen.
Similar content being viewed by others
References
Barrett A, Depledge MH, Powles RL. Interstitial pneumonitis following bone marrow transplantation after low dose rate total body irradiation. Int J Radiat Oncol Biol Phys 1983;9:1029–33
Berger C, et al. Late thyroid toxicity in 153 long-term survivors of allogeneic bone marrow transplantation for acute lymphoblastic leukaemia. Bone Marrow Transplant 2005;35:991–5
Bhatia S, et al. Late mortality in survivors of autologous hematopoietic-cell transplantation: report from the Bone Marrow Transplant Survivor Study. Blood 2005;105:4215–22
Bhatia S, et al. Solid cancers after bone marrow transplantation. J Clin Oncol 2001;19:464–71
Blaise D, et al. Allogeneic bone marrow transplantation for acute myeloid leukemia in first remission: a randomized trial of a busulfan-Cytoxan versus Cytoxan-total body irradiation as preparative regimen: a report from the Group d’Etudes de la Greffe de Moelle Osseuse. Blood 1992;79:2578–82
Blume KG, et al. A prospective randomized comparison of total body irradiation- etoposide versus busulfan-cyclophosphamide as preparatory regimens for bone marrow transplantation in patients with leukemia who were not in first remission: a Southwest Oncology Group study. Blood 1993;81: 2187–93
Bortin MM, et al. Factors associated with interstitial pneumonitis after bone-marrow transplantation for acute leukaemia. Lancet 1982;319: 437–9
Briot E, Dutreix A, Bridier A. Dosimetry for total body irradiation. Radiother Oncol 1990;18(Suppl 1):16–29
Bruno B, et al. Effects of allogeneic bone marrow transplantation on pulmonary function in 80 children in a single paediatric centre. Bone Marrow Transplant 2004;34:143–7
Clift RA, et al. Marrow transplantation for chronic myeloid leukemia: a randomized study comparing cyclophosphamide and total body irradiation with busulfan and cyclophosphamide. Blood 1994;84:2036–43
Cosset JM, et al. Clinical basis for TBI fractionation. Radiother Oncol 1990;18(Suppl 1):60–7
Deeg HJ, et al. Marrow transplantation for acute nonlymphoblastic leukemia in first remission: toxicity and long-term follow-up of patients conditioned with single dose or fractionated total body irradiation. Bone Marrow Transplant 1986;1:151–7
Devergie A, et al. Allogeneic bone marrow transplantation for chronic myeloid leukemia in first chronic phase: a randomized trial of busulfan-cytoxan versus cytoxan-total body irradiation as preparative regimen: a report from the French Society of Bone Marrow Graft (SFGM). Blood 1995;85:2263–8
Eich HT, Müller RP, Engenhart-Cabillic R, et al. Involved-node radiotherapy in early-stage Hodgkin’s lymphoma. Definition and guidelines of the German Hodgkin Study Group (GHSG). Strahlenther Onkol 2008;184:406–10
Faraci M, et al. Very late nonfatal consequences of fractionated TBI in children undergoing bone marrow transplant. Int J Radiat Oncol Biol Phys 2005;63:1568–75
Gerstein J, et al. Long-term renal toxicity in children following fractionated total-body irradiation (TBI) before allogeneic stem cell transplantation (SCT). Strahlenther Onkol 2009;185:751–5
Granados E, et al. Hematopoietic cell transplantation in acute lymphoblastic leukemia: better long term event-free survival with conditioning regimens containing total body irradiation. Haematologica 2000;85:1060–7
Kal HB, et al. Biologically effective dose in total-body irradiation and hematopoietic stem cell transplantation. Strahlenther Onkol 2006;182: 672–9
Miralbell R, et al. Renal insufficiency in patients with hematologic malignancies undergoing total body irradiation and bone marrow transplantation: a prospective assessment. Int J Radiat Oncol Biol Phys 2004;58: 809–16
Peters LJ, et al. Radiobiological considerations in the use of total-body irradiation for bone-marrow transplantation. Radiology 1979;131:243–7
Pommier P, et al. Second cancer after total-body irradiation (TBI) in childhood. Strahlenther Onkol 2009; 185(Suppl 2):13–6
Ramm U, Licher J, Moog J, et al. In vivo dosimetry with semiconducting diodes for dose verification in total-body irradiation. A 10-year experience. Strahlenther Onkol 2008;184:376–80
Ricardi U, et al. Late toxicity in children undergoing hematopoietic stem cell transplantation with TBI-containing conditioning regimens for hematological malignancies. Strahlenther Onkol 2009;185(Suppl 2):17–20
Ringden O, et al. A comparison of busulphan versus total body irradiation combined with cyclophosphamide as conditioning for autograft or allograft bone marrow transplantation in patients with acute leukaemia. Acute Leukaemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Br J Haematol 1996;93:637–45
Robin M, et al. A 10-year median follow-up study after allogeneic stem cell transplantation for chronic myeloid leukemia in chronic phase from HLAidentical sibling donors. Leukemia 2005;19:1613–20
Sampath S, Schultheiss TE, Wong J. Dose response and factors related to interstitial pneumonitis after bone marrow transplant. Int J Radiat Oncol Biol Phys 2005;63:876–84
Savani BN, et al. Prediction and prevention of transplant-related mortality from pulmonary causes after total body irradiation and allogeneic stem cell transplantation. Biol Blood Marrow Transplant 2005;11:223–30
Socie G, et al. Busulfan plus cyclophosphamide compared with total-body irradiation plus cyclophosphamide before marrow transplantation for myeloid leukemia: long-term follow-up of 4 randomized studies. Blood 2001; 98:3569–74
Tauchmanova L, et al. High prevalence of endocrine dysfunction in longterm survivors after allogeneic bone marrow transplantation for hematologic diseases. Cancer 2002;95:1076–84
Vettenranta K. Current European practice in pediatric myeloablative conditioning. Bone Marrow Transplant 2008;41(Suppl 2):S14–7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linsenmeier, C., Thoennessen, D., Negretti, L. et al. Total Body Irradiation (TBI) in Pediatric Patients. Strahlenther Onkol 186, 614–620 (2010). https://doi.org/10.1007/s00066-010-2089-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2089-2