Abstract
Background
Sepsis is a systemic inflammatory response usually correlated with multi-organ failure. Myocardial dysfunction is one of the adverse outcomes in septic patients and results in high mortality rates. The aim of this study was to investigate the impact of irbesartan in attenuation of cardiac depression during polymicrobial sepsis via decreased activation of the phospho-p38MAPK/nuclear factor (NF)-κB signaling pathway.
Materials and methods
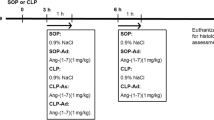
A model of polymicrobial sepsis induced via cecal ligation and puncture (CLP) with 8- to 12-week-old albino mice was used. Mice were treated with i.p. irbesartan (3 mg/kg) 1 h before CLP. Using a micro-tipped transducer catheter, the following hemodynamic parameters were evaluated after CLP: heart rate, ejection fraction, left ventricular (LV) end-diastolic pressure, LV systolic pressure, and cardiac output. Plasma levels of proinflammatory cytokines, including tumor necrosis factor (TNF)-alpha, interleukin (IL)-1 beta, IL-6, monocyte chemoattractant protein-1 (MCP-1), and cardiac troponin I (cTn-I), were measured via ELISA analysis. The degree of p38MAPK and NF-κB phosphorylation was assessed via Western blotting.
Results
Mice treated with irbesartan displayed improvement in LV function (ejection fraction: 42.4 ± 1.1% vs. 27.8 ± 3% in CLP mice). The attenuation of cardiac depression in irbesartan-treated mice was associated with lower levels of MCP-1 in plasma and a reduction in the levels of TNF-alpha, IL-1beta, and IL-6. Furthermore, irbesartan-treated mice displayed lower expression levels of p38-MAPK and NF-κB phosphorylation.
Conclusion
Irbesartan can attenuate cardiac dysfunction during polymicrobial sepsis possibly via a reduction of proinflammatory cytokines through decreased activation of the p38MAPK/NF-κB pathways.
Zusammenfassung
Hintergrund
Die Sepsis stellt eine systemische entzündliche Reaktion dar, die gewöhnlich mit Multiorganversagen einhergeht. Myokardfunktionsstörungen sind eine der ungünstigen Folgen bei septischen Patienten und führen zu einer hohen Mortalitätsrate. Ziel der vorliegenden Studie war es, den Einfluss von Irbesartan auf die Abschwächung der Kreislaufdepression bei polymikrobieller Sepsis über eine verminderte Aktivierung des Signalwegs von Phospho-p38MAPK/Nuclear-Factor(NF)-κB zu untersuchen.
Material und Methoden
Es wurde ein Modell der polymikrobiellen Sepsis verwendet, bei dem die Sepsis über eine Ligatur und Punktur des Zoekums („cecal ligation and puncture“, CLP) bei 8–12 Wochen alten Albinomäusen induziert wurde. Die Mäuse wurden i.p. mit Irbesartan (3 mg/kg) 1 h vor CLP behandelt. Unter Einsatz eines Mikrotip-Transducer-Katheters wurden die folgenden hämodynamischen Parameter nach CLP gemessen: Herzfrequenz, Ejektionsfraktion, linksventrikulärer (LV) enddiastolischer Druck, LV systolischer Druck und Herzzeitvolumen. Mittels ELISA-Test wurden die Plasmaspiegel proinflammatorischer Zytokine einschließlich Tumornekrosefaktor-alpha (TNF-α), Interleukin-1beta (IL-1β), IL-6, Monozyten-chemoattraktives Protein-1 (MCP-1) und kardiales Troponin I (cTn-I) bestimmt. Der Grad der Phosphorylierung von p38MAPK und NF-κB wurde per Western-Blot-Test ermittelt.
Ergebnisse
Die mit Irbesartan behandelten Mäuse wiesen eine Verbesserung der LV-Funktion auf (Ejektionsfraktion: 42,4 ± 1,1% vs. 27,8 ± 3% bei CLP-Mäusen). Die Abschwächung der Kreislaufdepression bei den mit Irbesartan behandelten Mäusen ging mit niedrigeren Plasmaspiegeln von MCP-1 und einer Senkung der Werte für TNF-α, IL-1β und IL-6 einher. Darüber hinaus zeigten die mit Irbesartan behandelten Mäuse eine geringere Expression der Phosphorylierung von p38-MAPK und NF-κB.
Schlussfolgerung
Irbesartan kann möglicherweise über eine Verminderung proinflammatorischer Zytokine durch geringere Aktivierung des p38MAPK/NF-κB-Signalwegs zu einer Abschwächung der kardialen Funktionsstörung bei polymikrobieller Sepsis führen.




Similar content being viewed by others
References
Drosatos K et al (2015) Pathophysiology of sepsis-related cardiac dysfunction: driven by inflammation, energy mismanagement, or both? Curr Heart Fail Rep 12(2):130–140
Wang J et al (2016) Clinical significance of plasma levels of brain natriuretic peptide and cardiac troponin T in patients with sepsis. Exp Ther Med 11(1):154–156. doi:10.3892/etm.2015.2863
Drosatos K et al (2013) PPARγ activation prevents sepsis-related cardiac dysfunction and mortality in mice: drosatos et al: PPARγ treats septic cardiac dysfunction. Circ Heart Fail 6(3):550–562
Romero-Bermejo FJ et al (2011) Sepsis-induced cardiomyopathy. Curr Cardiol Rev 7(3):163–183
Kumar A et al (1996) Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med 183(3):949–958
Prabhu SD (2004) Cytokine-induced modulation of cardiac function. Circ Res 95(12):1140–1153
Higashikuni Y et al (2013) Toll-like receptor-2 mediates adaptive cardiac hypertrophy in response to pressure overload through Interleukin-1β upregulation via nuclear factor κB activation. J Am Heart Assoc 2(6):e000267. doi:10.1161/jaha.113.000267
Layland J et al (2005) Protection against endotoxemia-induced contractile dysfunction in mice with cardiac-specific expression of slow skeletal troponin I. FASEB J 19(9):1137–1139
Zhang N et al (2015) Pharmacological TLR4 inhibition protects against acute and chronic fat-induced insulin resistance in rats. PLOS ONE 10(7):e0132575
Zbinden-Foncea H et al (2012) TLR2 and TLR4 activate p38 MAPK and JNK during endurance exercise in skeletal muscle. Med Sci Sports Exerc 44(8):1463–1472
Kim HM et al (2007) Crystal structure of the TLR4-MD-2 complex with bound endotoxin antagonist Eritoran. Cell 130(5):906–917
Dejager L et al (2011) Cecal ligation and puncture: the gold standard model for polymicrobial sepsis? Trends Microbiol 19(4):198–208
Chang CL et al (2012) Impact of apoptotic adipose-derived mesenchymal stem cells on attenuating organ damage and reducing mortality in Rat sepsis syndrome induced by cecal puncture and ligation. J Transl Med 10:244
Coletta C et al (2014) Endothelial dysfunction is a potential contributor to multiple organ failure and mortality in aged mice subjected to septic shock: preclinical studies in a murine model of cecal ligation and puncture. Crit Care. doi:10.1186/s13054-014-0511-3
Khan AI et al (2013) Erythropoietin attenuates cardiac dysfunction in experimental sepsis in mice via activation of the β‑common receptor. Dis Model Mech 6(4):1021–1030
Williams DL et al (1999) Early activation of hepatic NFkappaB and NF-IL6 in polymicrobial sepsis correlates with bacteremia, cytokine expression, and mortality. Ann Surg 230(1):95–104
Yousif NG, Al-Amran FG (2011) Novel toll-like receptor-4 deficiency attenuates trastuzumab (Herceptin) induced cardiac injury in mice. BMC Cardiovasc Disord 11:62
Slimani H et al (2014) Enhanced monocyte chemoattractant protein-1 production in aging mice exaggerates cardiac depression during endotoxemia. Crit Care 18(5):527
Turler M, Thoma S, Graves M, Lyman SM, Kasper JH (2015) Dopamine signaling attenuated myocardial injury during endotoxemia. Am J Biomed 3(7):381–391
Slimani H, Zhai Y, Yousif NG, Ao L, Zeng Q (2014) Enhanced monocyte chemoattractant protein-1 production in aging mice exaggerates cardiac depression during endotoxemia. Crit Care Med 18(5):527
Hullmann G et al (2015) Role of IL-1B in TLR4-mediated MCP-1expression: renal sepsis. Am J Biomed 3(1):22–31
Tracey SG et al (2014) Critical role of macrophage migration inhibitory factor in sepsis via interfere with MCP-1/CCL2 signaling pathway. Am J Biomed 2(6):688–701
Deshmane SL, Kremlev S, Amini S, Sawaya BE (2009) Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res 29(6):313–26; doi:10.1089/jir.2008.0027
Turler M, Thoma S, Graves M, Lyman SM, Kasper JH (2015) Dopamine signaling attenuated myocardial injury during endotoxemia. Am J Biomed 3(7):381391
Fukumoto J et al (2015) Sepsis and signal transduction pathway: cross-talk TLR4/ MyD88/TRIF. Am J Biomed 3(4):150–163
Colorado University, Everett A, Yousif N, Ao L, Cleveland J, Fullerton D, Meng X (2013) Ghrelin reduces myocardial injury following global ischemia and reperfusion via suppression of myocardial inflammatory response. Am J Biomed 1(2):38–48
Al-amran FG, Yousif NG, Meng XM (2011) A TLR4-MCP-1-macrophage IL18 cascade plays a major role in myocardial injury and cardiac dysfunction after permanent Ischemia. J Surg Res 165(2):265–266
Nasser YG, Cleveland JC Jr, Fullerton DA Jr, Meng X Jr (2012) Aging augments myocardial inflammatory response to ischemia and reperfusion: an obligatory role of TLR4. Shock 37:31–119
Yousif NG et al (2011) Expression of human interleukine-37 protects mouse heart against Ischemic injury through suppression of monocyte chemoattractant protein-1-mediated mononuclear cell accumulation. Circulation 124(Suppl 21):A8603
Yousif NG (2014) Novel therapeutic role of siglec-E in down-regulation TLR4-mediated inflammatory response after global myocardial ischemia and reperfusion. Cardiovasc Res 103:s90
Stamm C et al (2001) Inhibition of tumor necrosis factor-alpha improves postischemic recovery of hypertrophied hearts. Circulation 104(12 Suppl 1):I-350–I-355
Slimani HS et al (2014) Critical role IL-37 to ameliorate endotoxemic cardiac depression in aging mice: a critical role of suppression cardiodepressant cytokines. Cardiovasc Res 103:S92–S92
Woo J‑I et al (2010) Spiral ligament fibrocyte-derived MCP-1/CCL2 contributes to inner ear inflammation secondary to nontypeable H. influenzae-induced otitis media. BMC Infect Dis 10:314–314
Grupper R et al (2015) Critical role of microRNAs after global myocardial ischemia and reperfusuion. Am J Biomed 3(7):451–467
Gao Y‑J et al (2009) JNK-induced MCP-1 production in spinal cord astrocytes contributes to central sensitization and neuropathic pain. Neuroscience 29(13):4096–4108
Chang JH, Park JY, Kim SK (2006) Dependence on p38 MAPK signalling in the up-regulation of TLR2, TLR4 and TLR9 gene expression in Trichomonas vaginalis-treated HeLa cells. Immunology 118(2):164–170
O’Neill LA, Bowie AG (2007) The family of five: TIR-domain-containing adaptors in Toll-like receptor signalling. Nat Rev Immunol 7(5):353–364
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
N.G. Yousif, N.R. Hadi, F. Al-Amran, and Q.A. Zigam declare that they have no competing interests.
All national guidelines on the care and use of laboratory animals have been followed and that the necessary approval was obtained from the relevant authorities.
Rights and permissions
About this article
Cite this article
Yousif, N.G., Hadi, N.R., Al-Amran, F. et al. Cardioprotective effects of irbesartan in polymicrobial sepsis. Herz 43, 140–145 (2018). https://doi.org/10.1007/s00059-017-4537-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-017-4537-6