Abstract
Aims
Pulmonary vein isolation (PVI) during ablation of atrial fibrillation (Afib) may be associated with long fluoroscopy duration. Although most current publications report on fluoroscopy time (FT), the dose–area product (DAP) may be a more valuable parameter for depicting radiation exposure. The aim of our study was to describe a method to reduce DAP by simple means during ablation of Afib.
Methods
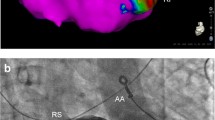
Patients undergoing Afib ablation using a three-dimensional (3D) mapping system were assigned to two fluoroscopy protocols: (1) standard settings with 7.5 pictures/s and collimation to the heart, fluoroscopy as needed for the convenience of the operator (standard group, SG); and (2) strict collimation to the left atrium, a frame rate of 4 pictures/s, shortened pulmonary vein angiography sequences, and maximal orientation by the 3D mapping system (redDAP group). The primary endpoint was DAP.
Results
The study comprised 206 patients, who were assigned to the SG (n = 101, 49 %) or to the redDAP group (n = 105, 51 %). Mean FT was significantly reduced from 29.9 ± 11.3 min (SG) to 13.3 ± 8.3 min (redDAP group); mean DAP was reduced by approximately 90 % from 8,690 ± 5,727 to 837 ± 647 cGycm2. The groups did not differ significantly in body mass index (28.8 ± 4.1 vs. 29.0 ± 5.0). PVI could be achieved in 98 of 101 patients (97 %) from the SG group and in all patients (100 %) from the redDAP group. Procedure time was significantly longer in the redDAP group (160.9 ± 35.7 vs. 138.1 ± 34.3 min).
Conclusion
Radiation exposure during Afib ablation procedures can be reduced with simple means by strict collimation to the left atrium, a frame rate of 4 pictures/s, shortened pulmonary vein angiography sequences, and maximal 3D orientation.
Zusammenfassung
Ziel
Die Pulmonalvenenisolation (PVI) bei der Ablation von Vorhofflimmern (VF) kann mit einer langen Durchleuchtungsdauer einhergehen. In den meisten aktuellen Veröffentlichungen wird zwar die Durchleuchtungsdauer angegeben, aber möglicherweise stellt das Dosis-Flächen-Produkt (DFP) einen Parameter von höherer Aussagekraft dar, um die Strahlenbelastung zu erfassen. Ziel der vorliegenden Studie war es, ein Verfahren zur Verminderung des DFP mit einfachen Mitteln bei Ablation von VF zu beschreiben.
Methoden
Patienten, bei denen eine Ablation wegen VF unter Einsatz eines dreidimensionalen (3-D-)Mapping-Systems erfolgte, wurden 2 unterschiedlichen Durchleuchtungsschemata zugeteilt: 1. Standardeinstellungen mit 7,5 Bildern/s und Einblendung auf das Herz, Durchleuchtung nach Erfordernissen des Operateurs (Standardgruppe, SG) und 2. strenge Einblendung auf den linken Vorhof, eine Bildfrequenz von 4 Bildern/s, verkürzte Pulmonalvenenangiographiesequenzen und maximale Orientierung mittels 3-D (redDAP-Gruppe). Primärer Endpunkt war das DFP.
Ergebnisse
Die Studie umfasste 206 Patienten, die der SG (n = 101, 49 %) oder der redDAP-Gruppe zugeteilt wurden (n = 105, 51 %). Die durchschnittliche Durchleuchtungsdauer wurde signifikant von 29,9 ± 11,3 min (SG) auf 13,3 ± 8,3 min (redDAP-Gruppe) reduziert; das durchschnittliche DFP wurde um annähernd 90 % von 8690 ± 5727 auf 837 ± 647 cGycm2 vermindert. Die Gruppen unterschieden sich nicht signifikant beim Body-Mass-Index (28,8 ± 4,1 vs. 29,0 ± 5,0). Die PVI wurde bei 98 von 101 Patienten (97 %) der SG und bei allen Patienten (100 %) der redDAP-Gruppe erzielt. Die Dauer der Prozedur war in der redDAP-Gruppe signifikant länger (160,9 ± 35,7 vs. 138,1 ± 34,3 min).
Schlussfolgerung
Die Strahlenbelastung bei Ablation von VF kann mit einfachen Mitteln durch strenge Einblendung auf den linken Vorhof, eine Bildfrequenz von4 Bildern/s, verkürzte PV-Angiographiesequenzen und maximale 3-D-Orientierung reduziert werden.





Similar content being viewed by others
References
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D et al (2012) 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 33(21):2719–2747
Macle L, Weerasooriya R, Jais P, Scavee C, Raybaud F, Choi KJ, Hocini M, Clementy J, Haissaguerre M (2003) Radiation exposure during radiofrequency catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol 26(1 Pt 2):288–291
Estner HL, Deisenhofer I, Luik A, Ndrepepa G, von Bary C et al (2006) Electrical isolation of pulmonary veins in patients with atrial fibrillation: reduction of fluoroscopy exposure and procedure duration by the use of a non-fluoroscopic navigation system (NavX). Europace 8(8):583–587
Finlay MC, Hunter RJ, Baker V, Richmond L, Goromonzi F et al (2012) A randomised comparison of Cartomerge vs. NavX fusion in the catheter ablation of atrial fibrillation: the CAVERN Trial. J Interv Card Electrophysiol 33(2):161–169
De Buck S, La Gerche A, Ector J, Wielandts JY, Koopman P et al (2012) Asymmetric collimation can significantly reduce patient radiation dose during pulmonary vein isolation. Europace 14(3):437–444
Steven D, Servatius H, Rostock T, Hoffmann B, Drewitz I et al (2010) Reduced fluoroscopy during atrial fibrillation ablation: benefits of robotic guided navigation. J Cardiovasc Electrophysiol 21(1):6–12
Lakkireddy D, Nadzam G, Verma A, Prasad S, Ryschon K, Di Biase L, Khan M, Burkhardt D, Schweikert R, Natale A (2009) Impact of a comprehensive safety program on radiation exposure during catheter ablation of atrial fibrillation: a prospective study. J Interv Card Electrophysiol 24(2):105–112
Shah AJ, Pascale P, Miyazaki S, Liu X, Roten L, Derval N et al (2012) Prevalence and types of pitfall in the assessment of mitral isthmus linear conduction block. Circ Arrhythm Electrophysiol 5(5):957–967
Dixit S, Marchlinski FE, Lin D, Callans DJ, Bala R, Riley MP et al (2012) Randomized ablation strategies for the treatment of persistent atrial fibrillation: RASTA study. Circ Arrhythm Electrophysiol 5(2):287–294
Kiuchi K, Kircher S, Watanabe N, Gaspar T, Rolf S, Arya A et al (2012) Quantitative analysis of isolation area and rhythm outcome in patients with paroxysmal atrial fibrillation after circumferential pulmonary vein antrum isolation using the pace-and-ablate technique. Circ Arrhythm Electrophysiol 5(4):667–675
Chao TF, Tsao HM, Lin YJ, Tsai CF, Lin WS, Chang SL et al (2012) Clinical outcome of catheter ablation in patients with nonparoxysmal atrial fibrillation: results of 3-year follow-up. Circ Arrhythm Electrophysiol 5(3):514–520
Weerasooriya R, Khairy P, Litalien J, Macle L, Hocini M et al (2011) Catheter ablation for atrial fibrillation: are results maintained at 5 years of follow-up? J Am Coll Cardiol 57(2):160–166
Rostock T, Salukhe TV, Steven D, Drewitz I, Hoffmann BA et al (2011) Long-term single- and multiple-procedure outcome and predictors of success after catheter ablation for persistent atrial fibrillation. Heart Rhythm 8(9):1391–1397
Wieczorek M, Hoeltgen R, Akin E, Salili AR, Oral H, Morady F (2010) Results of short-term and long-term pulmonary vein isolation for paroxysmal atrial fibrillation using duty-cycled bipolar and unipolar radiofrequency energy. J Cardiovasc Electrophysiol 21(4):399–405
Stabile G, Scaglione M, del Greco M, De Ponti R, Bongiorni MG et al (2012) Reduced fluoroscopy exposure during ablation of atrial fibrillation using a novel electroanatomical navigation system: a multicentre experience. Europace 14(1):60–65
Peyrol M, Sbragia P, Quatre A, Boccara G, Zerrouk Z et al (2013) Pulmonary vein isolation using a single size cryoballoon chosen according to transesophageal echocardiography information. Int J Cardiol 168(1):108–111
Rogers DP, England F, Lozhkin K, Lowe MD, Lambiase PD, Chow AW (2011) Improving safety in the electrophysiology laboratory using a simple radiation dose reduction strategy: a study of 1007 radiofrequency ablation procedures. Heart 97(5):366–70
Rolf S, Sommer P, Gaspar T, John S, Arya A et al (2012) Ablation of atrial fibrillation using novel 4-dimensional catheter tracking within autoregistered left atrial angiograms. Circ Arrhythm Electrophysiol 5(4):684–690
Letsas KP, Siklódy CH, Korantzopoulos P, Weber R, Bürkle G et al (2013) The impact of body mass index on the efficacy and safety of catheter ablation of atrial fibrillation. Int J Cardiol 164(1):94–98
Hirshfeld JW Jr, Baiter S, Brinker JA, Kern MJ, Klein LW, Lindsay BD et al (2005) American College of Cardiology Foundation; American Heart Association/; HRS; SCAI; American College of Physicians Task Force on Clinical Competence and Training. ACCF/AHA/HRS/SCAI clinical competence statement on physician knowledge to optimize patient safety and image quality in fluoroscopically guided invasive cardiovascular procedures: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training. Circulation 111(4):511–532
Caponi D, Corleto A, Scaglione M, Blandino A, Biasco L et al (2010) Ablation of atrial fibrillation: does the addition of three-dimensional magnetic resonance imaging of the left atrium to electroanatomic mapping improve the clinical outcome?: a randomized comparison of Carto-Merge vs. Carto-XP three-dimensional mapping ablation in patients with paroxysmal and persistent atrial fibrillation. Europace 12(8):1098–1104
Bänsch D, Bittkau J, Schneider R, Schneider C, Wendig I, Akin I et al (2013) Circumferential pulmonary vein isolation: wait or stop early after initial successful pulmonary vein isolation? Europace 15(2):183–188
Rivard L, Hocini M, Rostock T, Cauchemez B, Forclaz A, Jadidi AS et al (2012) Improved outcome following restoration of sinus rhythm prior to catheter ablation of persistent atrial fibrillation: a comparative multicenter study. Heart Rhythm 9(7):1025–1030
Kesek M, Wallenius N, Rönn F, Höglund N, Jensen S (2006) Reduction of fluoroscopy duration in radiofrequency ablation obtained by the use of a non-fluoroscopic catheter navigation system. Europace 8(12):1027–1030
Estner HL, Deisenhofer I, Luik A, Ndrepepa G, von Bary C, Zrenner B, Schmitt C (2006) Electrical isolation of pulmonary veins in patients with atrial fibrillation: reduction of fluoroscopy exposure and procedure duration by the use of a non fluoroscopic navigation system (NavX). Europace 8(8):583–587
Jilek C, Hessling G, Ammar S, Fichtner S, Reents T, Estner HL et al (2011) Visualization of multiple catheters in left atrial ablation procedures. Comparison of two different 3D mapping systems. Herzschrittmacherther Elektrophysiol 22(1):39–45
Reddy VY, Morales G, Ahmed H, Neuzil P, Dukkipati S, Kim S et al (2010) Catheter ablation of atrial fibrillation without the use of fluoroscopy. Heart Rhythm 7(11):1644–1653
Wielandts JY, De Buck S, Ector J, Lagerche A, Willems R, Bosmans H et al (2010) Three-dimensional cardiac rotational angiography: effective radiation dose and image quality implications. Europace 12(2):194–201
Hart D, Hillier MC, Wall BF (2009) National reference doses for common radiographic, fluoroscopic and dental X-ray examinations in the UK. Br J Radiol 82(973):1–12
Diagnostische Referenzwerte—Bundesamt für Strahlenschutz. www.bfs.de/de/ion/medizin/referenzwerte02.pdf. Accessed 22 June 2010
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Schneider, J. Lauschke, C. Schneider, T. Tischer, A. Glass, and D. Bänsch state that there are no conflicts of interest.
Additional information
R. Schneider and J. Lauschke contributed equally to this article.
Rights and permissions
About this article
Cite this article
Schneider, R., Lauschke, J., Schneider, C. et al. Reduction of radiation exposure during ablation of atrial fibrillation. Herz 40, 883–891 (2015). https://doi.org/10.1007/s00059-015-4307-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-015-4307-2
Keywords
- Atrial fibrillation
- Radiofrequency ablation
- Three-dimensional electro-anatomical reconstruction
- Fluoroscopy time
- Dose–area product