Abstract
Introduction
Inflammation is a defensive response of the organism to irritation which is manifested by redness, swelling, heat, pain and dysfunction. The inflammatory response underlies the role of various diseases. Ferroptosis, a unique modality of cell death, driven by iron-dependent lipid peroxidation, is regulated by multifarious cellular metabolic pathways, including redox homeostasis, iron processing and metabolism of lipids, as well as various signaling pathways associated with diseases. A growing body of evidence suggests that ferroptosis is involved in inflammatory response, and targeting ferroptosis has great prospects in preventing and treating inflammatory diseases.
Materials and methods
Relevant literatures on ferroptosis, inflammation, inflammatory factors and inflammatory diseases published from January 1, 2010 to now were searched in PubMed database.
Conclusion
In this review, we summarize the regulatory mechanisms associated with ferroptosis, discuss the interaction between ferroptosis and inflammation, the role of mitochondria in inflammatory ferroptosis, and the role of targeting ferroptosis in inflammatory diseases. As more and more studies have confirmed the relationship between ferroptosis and inflammation in a wide range of organ damage and degeneration, drug induction and inhibition of ferroptosis has great potential in the treatment of immune and inflammatory diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ferroptosis, a relatively new form of cell death first discovered in 2012, is induced by small molecule compound erastin (an inducer of ferroptosis) and dependent on iron and lipid peroxidation, which is different from autophagy, pyrosis and other forms of cell death [1]. The morphological features are observed as cell swelling, dense electron of mitochondria, rupture of outer membrane, reduction or disappearance of mitochondrial cristae. Three fundamental hallmarks define ferroptosis: the dysfunction of lipid peroxide scavenging, the existence of redox active iron and the oxidation of phospholipids containing polyunsaturated fatty acids (PUFA) [1,2,3]. The molecular basis of ferroptosis includes glutamate/cystine anti-transporter, antioxidant system (glutathione peroxidase 4, GPX4), iron metabolism, unsaturated fatty acid metabolism, and ferroptosis suppressor protein 1 (FSP1)-ubiquinone system. As a kind of stress response, ferroptosis has pathological roles in a wide variety of diseases, including neurodegenerative diseases, cancer, inflammatory diseases of various organs, ischemia–reperfusion injury (IRI), and brain injury, among others.
Inflammation is the activation of innate immune cells by damage and microbe-associated molecular patterns, manifested as the recruitment of macrophages and neutrophils, as well as the appearance of five major signs: rubor (redness), calor (heat), tumor (swelling), dolor (pain), and functio laesa (loss of function) [4]. On the one hand, inflammation is beneficial to the body. Inflammation benefits the host by promoting the removal of invading pathogens and removing cell debris after tissue damage. Inflammation also stimulates tissue repair and regeneration to restore homeostasis and body health [5, 6]. On the other hand, immune cells activated by inflammatory responses are usually accompanied by further inevitable damages to the host through the release of cytokines such as reactive oxygen species (ROS). It is the basis of a variety of physiological and pathological processes, which can cause serious damage to the body.
The complexity of the known regulatory pathways of ferroptosis makes it inevitably play an important pathological role in a variety of diseases, such as inflammatory diseases. Ferroptosis is accompanied by the release of pro-inflammatory molecules, such as interleukin (IL)-1β and IL-18 [7]. Elucidating the relationship between ferroptosis and inflammation may provide valuable insights into developing novel targets for inflammatory diseases. In recent years, more and more studies have shown that ferroptosis inhibitors are of great benefit in the treatment of inflammation [2, 8, 9]. Mitochondria are important organelles in inflammatory response. Here, we also discussed the relationship among mitochondria, inflammation and ferroptosis. This article reviews the molecular mechanisms of ferroptosis, describes the role of ferroptosis in inflammation, and summarizes the role of ferroptosis inhibitors in the treatment of inflammatory diseases.
Methodology
A systematic literature review of PubMed database was conducted with “ferroptosis” and “inflammation” as keywords. Inflammation, Ferroptosis, Lipid Metabolism, Iron Metabolism, IL-6, TNF-α, IL-1β, PUFA, arachidonic acid (AA), COX2, Mitochondria, NF-κB, Liposome, acute kidney injury (AKI), acute lung injury (ALI), inflammatory bowel disease (IBD), Neurodegenerative Diseases, IRI, etc. are the keywords to collect and summarize the articles published so far in 2010 to understand the role of Ferroptosis in inflammatory diseases (Fig. 1).
Mechanism of ferroptosis
Regulation of intracellular iron homeostasis
Iron is a transition metal that is a basic component of almost all living cells and organisms. It is a component of a variety of metal proteins, involved in tissue oxygen transport, mitochondrial respiratory electron transfer reaction, DNA synthesis and repair, metabolism of exogenous substances and other key biochemical process. Overload of iron content can cause multiple organ damage (e.g., liver, kidney, spleen, etc.) and cell death. Therefore, maintaining the homeostasis of iron is crucial to human body.
Iron metabolism is the dynamic process of absorption, storage, utilization and excretion. Many mRNAs involved in iron metabolism include iron-responsive elements (IREs): stem-loop structures located in the 5ʹ- or 3ʹ-untranslated regions (UTRs) on the flanking of coding sequence (CDS) [10]. Intracellular iron homeostasis is associated with iron regulatory proteins 1 and 2 (IRP1, IRP2) and the IRE system. IRP is a protein that can bind to the 5ʹ or 3ʹ UTRs of IRE mRNAs. These key mRNAs are involved in iron regulation, including iron uptake (e.g., DMT1, TFR1), iron retention (e.g., ferritin subunits: FTH1, FTL) and iron export [e.g., ferroportin (FPN)]. Upon cellular iron deficiency, IRP not only binds to the 5′ IRE of ferritin and FPN to inhibit their translation, but also binds to the 3′ IRE of TFR1 to inhibit their degradation. When iron meets the demand, IRP degrades and these bindings stop [11]. Therefore, in response to the cell demands for iron, IRE/IRP interaction promotes the stability of TFR1 mRNA and inhibits FTH translation, thereby regulating the uptake and storage of cell iron [12]. Furthermore, hepcidin the main regulator of iron homeostasis, involves in iron metabolism through the internalization and degradation of FPN [13].
Ferroptosis is a new type of cell death that is distinct from other cell deaths. Excessive iron accumulation is easy to induce fenton reaction, resulting in a large amount of ROS along with membrane lipid peroxidation and further inducing ferroptosis. The signaling pathways affecting iron metabolism have been proved to regulate ferroptosis [14]. PPARα activation attenuates iron overload-induced ferroptosis in mouse liver by promoting GPX4 expression and decreasing TRF expression [15]. One of the markers of liver injury after liver transplantation is the high level of serum ferritin. Yamada et al. found that the iron chelation of deferoxamine (DFO) can significantly inhibit liver ischemia–reperfusion (I/R) ferroptosis and reduce liver I/R injury [16]. In culture and xenotransplantation models, downregulation of HSPB1 or HSF1 gene increases the sensitivity of cancer cells to ferroptosis through intracellular iron accumulation and related lipid peroxidation, while overexpression of HSPB1 inhibits ferroptosis [17].
The sensitivity of cancer cells to ferroptosis is affected by regulating intracellular iron homeostasis, and the effect of cancer treatment is achieved. A recent report shows that artemisinin compounds can sensitize cancer cells to ferroptosis by regulating iron homeostasis [18]. The specific mechanism is the ability of dihydroartemisinin (DAT) to induce lysosomal degradation of ferritin in a non-autophagic manner, increasing free iron levels and making cells more sensitive to ferroptosis [18]. In addition, by binding to free iron in cells, the binding of IRPs to mRNA molecules containing IRE sequence is stimulated. Cells contain a small amount of incompatible and redox active Fe2+, the so-called “labile iron pool” (LIP). Ferroptosis inhibitors and iron chelators (such as deferiprone (DFP)) can inhibit the fenton reaction by reducing the availability of iron in the LIP and inhibiting the production of free radicals [19]. Therefore, iron homeostasis is closely related to ferroptosis, and iron accumulation is a necessary condition for ferroptosis (Fig. 2).
DMT1 and TFR1 mediate the transfer of Fe2+ into cells, and Heme in the cytoplasm can release Fe2+, which is stored in LIP and FTH1 in the cytoplasm. FPN mediates the release of Fe2+ from the cytoplasm into the blood. Hepcidin can combine with FPN to promote its internalization and degradation. When intracellular Fe2+ is absent, IRP binds with ferritin and FPN to inhibit their translations, as well as inhibiting the degradation of TFR1, ultimately increasing the content of Fe2+ in cells. Fe2+ in the cytoplasm generates ROS through fenton reaction, resulting in ferroptosis.
Lipid peroxidation
Lipid peroxidation is a free radical-driven reaction that primarily affects PUFAs in cell membranes. PUFAs undergo enzymatic or non-enzymatic oxidation reactions to form lipid hydroperoxides. Lipid hydroperoxides can react with Fe2+ to generate toxic lipid free radicals though fenton reaction. Lipid free radicals can attack major components of cells and cause cell damage, resulting to ferroptosis. In addition, lipid free radicals can also transfer protons from adjacent PUFAs, restarting the lipid peroxidation process. Lipid peroxidation products include initial lipid peroxides (LOOHs) and subsequent reactive aldehydes (such as malondialdehyde (MDA) and 4-hydroxynonenal (4HNE)), which increase during ferroptosis and are also among the markers of ferroptosis [1]. Lipid peroxidation directly damages phospholipids, and oxidized phospholipids can also play an important role in many inflammatory diseases and mediate pro-inflammatory changes [20].
The GPX4, together with glutathione (GSH) as an essential cofactor, is an antioxidant enzyme that neutralise LOOHs and protect the fluidity of membranes, thus protecting cells and membranes from peroxidation. GSH can be recycled by GSH reductase and nicotinamide adenine dinucleotide phosphate (NADPH)/H+ reduction oxidation of glutathione disulfide (GSSG) to inhibit ROS production [21]. Transcription factor nuclear factor erythroid 2-related factor 2 (NRF2) is a key regulator of cellular antioxidant response, which controls the expression of genes involved in antioxidant and electrophilic stress. Due to gene mutation, endogenous stress-induced modification, competitive binding of other interacting partners or exogenous pharmacological inhibition, NRF2 can be translocated to the nucleus to initiate the transcription of genes containing antioxidant response elements (ARE). NRF2 targets can be divided into three categories: iron/metal metabolism, intermediate metabolism and GSH synthesis/metabolism, all of which have validated ARE. NRF2 has been proved to regulate the activities of several ferroptosis and lipid peroxidation-related proteins [22].
Mammalian arachidonic acid lipoxygenases (ALOXs) family (arachidonic acid lipoxygenase) can mediate PUFA peroxidation to produce AA/AdA-PE-OOHs, which play a tissue or cell dependent role, leading to ferroptosis [1]. ALOX is not the only regulator of lipid peroxidation in ferroptosis. In fact, cytochrome P450 oxidoreductase (POR) combines with two cofactors [lutein mononucleotide (FMN) and lutein adenine dinucleotide (FAD)] to directly provide electrons to P450 enzymes from NADPH, the basic electron donor of all organisms, thereby promoting the peroxidation of PUFA in cancer cells in a manner independent of ALOX [23]. However, it is unclear whether other oxygenase, such as cyclooxygenase (COX) and peroxidase, play a similar role in lipid peroxidation.
At present, studies have shown that peroxisomes promote ferroptosis by synthesizing polyunsaturated ether phospholipids (PUFA-ePL), which acts as a substrate for lipid peroxidation and resulting in the induction of ferroptosis [24]. Therefore, peroxisome-driven synthesis of ether phospholipids, rather than other lipids, plays an important role in regulating susceptibility to ferroptosis. The prevailing view has long been that ferroptosis is mainly caused by peroxidation of long-chain PUFAs through non-enzymatic oxidation of free radicals or enzymatic stimulation of lipoxygenases (LOXs). There is emerging evidence revealing that long-chain saturated fatty acids (SFA) may be related to ferroptosis, and FAR1 is a key factor in ferroptosis mediated by SFA. FAR1 catalyzes the reduction of C16 or C18 SFA to fatty alcohols, which has been identified as a critical role for the synthesis of alkyl ether lipids and acetal phospholipids. FAR1 inactivation reduces SFA-dependent ferroptosis [25]. Therefore, FAR1-mediated ferroptosis depends on peroxisome-driven ether phospholipid biosynthesis (Fig. 3).
PUFA is oxidized under the action of ACSL4 and other factors, while NRF2 pathway can inhibit the oxidation of PUFA, thereby reducing the degree of lipid peroxidation and ultimately inhibiting ferroptosis. Cystine is transferred into cells mediated by System Xc-, and promotes the expression of GPX4 through GSH-GSSG pathway, thereby inhibiting lipid peroxidation and ferroptosis.
Regulatory pathway of ferroptosis
Ferroptosis occurs through iron-catalyzed lipid peroxidation, which is triggered by non-enzymatic (fenton reaction) and enzymatic mechanism (LOX). The accumulation of LOOHs, mainly phosphatidylethanolamine-OOH (PE-OOH), eventually leads to ferroptosis, while iron acts as a catalyst or a key regulator of ferroptosis [26]. PUFAs are the main targets of membrane lipid peroxidation [27]. It is currently believed that the initial signal of ferroptosis induction is the production of ROS from various sources, especially iron metabolism, mitochondrial electron transport chain and NADPH oxidase (NOX) protein family [28].
The system Xc–-GSH-GPX4 axis
System xc− consists of a regulatory subunit solute carrier family 3 member 2 (SLC3A2) and a catalytic subunit solute carrier family 7 member 11 (SLC7A11) [29], which promotes the exchange of extracellular cystine and intracellular glutamate on the plasma membrane. SLC7A11 is a major functional subunit that can transport cystine into cells for GSH synthesis. SLC7A11 knockout mice appear healthy and fertile, and fibroblasts isolated from these mice undergo cell death, which can be rescued by the presence of β-mercaptoethanol (β-ME), N-acetylcysteine (NAC) or vitamin E [30]. Badgley MA et al. found that the deletion of the system XC− subunit SLC7A11 can induce tumor-selective ferroptosis and inhibit the growth of pancreatic ductal adenocarcinoma (PDAC) [31]. Therefore, when the cystine/glutamate transporter is disrupted, GSH is depleted, thus causing inactivation of GPX4, ultimately resulting in lipid peroxidation accumulation and ferroptosis. Other than that, GPX4 can use tripeptide GSH as a cofactor to detoxify the lipid peroxidation formed during oxidative stress, thereby inhibiting the occurrence of ferroptosis.
Non GPX4 dependent pathways
Recently, an antioxidant pathway independent of GPX4 has been found, which relies on AIFM2-mediated coenzyme Q (CoQ) production [32, 33]. CoQ, also known as panquinone, is an endogenously generated isoprenoid benzoquinone compound, which is ubiquitous in nature. In addition, ubiquinol-10 (CoQ10H2), the reduction form of CoQ10, was used as an effective lipophilic antioxidant involved in the recovery of other antioxidants, such as tocopherol and ascorbic acid. CoQ10 is a key component of mitochondrial electron transport chain, which can inhibit lipid peroxidation by capturing free radical intermediates in this process [34]. AIFM2 (now renamed FSP1) was screened by gene screening, which can block lipid peroxidation and inhibit ferroptosis by regenerating reduced CoQ, independently of any demand for GPX4 or GSH [32, 33]. In addition, recent studies have reported DHODH inactivation induces extensive mitochondrial lipid peroxidation and ferroptosis in GPX4low cancer cells, whereas DHODH inactivation synergizes with ferroptosis inducers to induce mitochondrial lipid peroxidation and ferroptosis in GPX4high cancer cells. Mechanistically, DHODH operates in parallel to mitochondrial GPX4 (but independent of cytosolic GPX4 or FSP1) to inhibit ferroptosis in the mitochondrial inner membrane, through reducing ubiquinone (CoQ) to ubiquinol (CoQH2), a radical-trapping antioxidant with anti-ferroptosis activity [33]. In addition to mediating the reduction of CoQ10 production, AIFM2 supports the anti-injury effect of membrane AIFM2 by activating the inner sorting complex required for plasma membrane transport (ESCRT) -III dependent membrane repair, which is related to ferroptosis resistance [35]. In addition, another pathway independent of GPX4 has been reported. The metabolic derivative tetrahydrobiopterin/dihydrobiopterin (BH4/BH2) synthesized by GCH1 (GTP hydrolase 1) may also antagonize ferroptosis by controlling the production of CoQ10 [30].
The NRF2-HO-1 signaling pathway
NRF2 is a transcription factor and phosphorylated NRF2 translocate into the nucleus to transactivate its target genes, including heme oxygenase-1(HO-1), as well as NRF2 itself [36]. HO-1 is an enzyme that exerts anti-inflammatory and antioxidant stress effects [37]. NRF2 is a critical modulator of the expression of HO-1. HO-1 mediates heme decomposition into carbon monoxide, iron and biliverdin [38]. Among them, biliverdin and its reduced bilirubin have an effective ROS scavenging activity to resist peroxides, peroxynitrite, hydroxyl and superoxide radicals. It’s proved that tagitinin C induces ferroptosis through ER stress-mediated activation of PERK-NRF2-HO-1 signaling pathway [36]. So how does the NRF2-HO-1 axis regulate ferroptosis? As a matter of common knowledge that NRF2 is a key regulator of endogenous antioxidant pathways. NRF2 targets play a key role in the regulation of iron metabolism. The light and heavy chains of ferritin (FTL/FTH1), which is a key iron storage protein, and also the FPN responsible for iron flowing out of cells, are controlled by NRF2 [39]. In addition to iron metabolism, NRF2 is also involved in the regulation of GSH antioxidant system. The expression of enzymes involved in GSH synthesis was controlled by NRF2, including glutamate cysteine ligase (GCLC/GCLM), glutathione synthase (GSS), and SLC7A11 [22]. Iron metabolism and GSH synthesis are important regulatory processes of ferroptosis, and NRF2/HO-1 is the main signal pathway regulating ferroptosis. Moreover, activation of NRF2-HO-1 antioxidant element signaling pathway is the main mechanism of cellular defense against oxidative stress. For example, zinc increased the expression of NRF2/HO-1, thereby increasing the contents of GPX4, SOD, and GHS and reducing the levels of LOOHs, MDA, and ROS [40], ultimately thereby inhibiting the onset of ferroptosis.
Correlation between ferroptosis and inflammation
The inducing factors of inflammation are generally divided into three types: loss or damage of tissue structure, temporary or permanent loss of tissue function, and destruction of body regulation function [41]. As we all know, controlling inflammatory response can play a protective role by enabling the body adapt to stimulation, while improper regulation may cause harmful stimulus, such as aggravating collateral tissue damage [41, 42].
It is reported that as a new form of cell death, ferroptosis is closely related to inflammation. Through the mediums of some ferroptosis regulators, such as GPX4, ROS, LOXs, and inflammatory mediators produced in the process of ferroptosis, ferroptosis can aggravate inflammatory response to varying degrees. Here, we describe the relevance of several inflammatory mediators and metabolic pathways that mediate inflammation and ferroptosis (Fig. 4; Table 1).
Proinflammatory cytokines
The expression of pro-inflammatory cytokines can be regulated by a variety of factors, including cytokines themselves or LPS [43]. Previous studies have shown that circulating inflammatory mediators, such as IL-1β, IL-6 and tumor necrosis factor-α (TNF-α), play a considerable role in the induction of endocrine disorder during inflammation [43]. In the process of immune response to infection, the activation of coagulation pathways leads to the excessive production of proinflammatory cytokines, which ultimately leads to multiple organ injury.
IL-6
Iron calmodulin participates in the intestinal absorption and release of iron, thus maintaining iron homeostasis, and plays a pivotal role in a variety of ferroptosis-related diseases [44, 45]. Some studies have shown that IL-6 participates in iron metabolism by mediating the expression of ferritin, and iron overload in turn promotes the expression of pro-inflammatory cytokines, such as IL-6 and IL-1β, via regulating the redox balance [46]. IL-6 has been documented in a variety of chronic inflammation, such as IBD, multiple sclerosis (MS), rheumatoid arthritis (RA) and inflammatory lung disease [47]. IL-6, highly expressed in degenerative chondrocytes, induces lipid peroxidation and iron imbalance through the IL-6/miR-10a-5p/IL-6R axis, which promotes the occurrence of ferroptosis and aggravates the inflammatory response of intervertebral disc lesions [48]. Some chronic diseases are along with the activation of NF-κB pathway and IL-6, the downstream factor, while IL-6 further plays the role of anti-ferritin through JAK1/STAT3 pathway. IL-6 and sIL-6R α synergism can promote inflammation and the transformation of inflammatory types through leukocyte recruitment [44, 49]. Similarly, IL-6–IL-2 axis can regulate and maintain the homeostasis of T17/Treg cells, and then regulate the process of inflammation [50].
TNF-α
The content of serum TNF-α in tissues was significantly increased when ferroptosis occurs. Studies have shown that ferroptosis inhibitors can inhibit TNF-α [51]. TNF-α has complex pathophysiological functions: it participates in the formation of vasodilation and edema, as well as the adhesion between leukocytes and epithelial cells via the expression of adhesion molecules, regulates blood coagulation, and indirectly induces fever [52]. Under the action of pro-inflammatory factors (such as virus, infection, etc.), M1 macrophages polarize and secrete TNF-α and iNOS [53]. TNF-α, inducing the production of iNOS, prostaglandins (PGE2, PGF2α, PGI2) and ROS, participates in and promotes inflammatory response such as aggravating the oxidative stress at the inflammatory site and participating in the formation of edema, which leads to the vicious circle of inflammation. The phenomenon of high expression of systemic TNF-α is manifested in RA, IBD and sepsis, and is associated with the high incidence rate of CVD, as well as atherothrombotic events, indicating that TNF-α is closely related to pathophysiology [54].
In addition, LPS induced sepsis and systemic inflammation are closely related to ferroptosis. Ferrostatin-1 (Fer-1, a ferroptosis inhibitor) and lipoxstatin-1 (a kind of ferroptosis inhibitors) have been shown to inhibit elevated levels of TNF- α and IL-6 in sepsis [55,56,57]. In addition, TNF treatment of cells can result in sustained downregulation of GPX4 expression, which is critical for the production of lipid mediators [58]. ROS, one of the markers of ferroptosis, activates NF-κB/NOX pathway, which inducing the production of inflammatory mediators (including TNF-α).
IL-1β
IL-1β is one of the IL-1 family members with the most pro-inflammatory characteristics [59]. As an upstream signal of NLRP3 inflammasome assembly, mitochondrial dysfunction, ROS and lysosomal destruction activate NLRP3 inflammasome, leading to subsequent IL-1β maturation [60]. The pro-inflammatory pattern of IL-1β indicates that it can participate in the occurrence of a variety of inflammatory diseases. It has been reported that IL-1β can induce liver injury and inflammation in mice, and participate in the formation of systemic inflammation, RA, periodontitis and secondary inflammatory injury in the brain caused by asthma [61,62,63,64,65].
It is worthy of note that in osteoarthritis (OA), IL-1β can inhibit the expression of SLC7A11 and GPX4, the markers of ferroptosis, and increase the expression of P53 and ACSL4, indicating that IL-1β is one of the bridges between inflammation and ferroptosis [66]. In addition, the existing research results show that IL-1β induces the activation of P53-XCT-GSH axis in endothelial cells and inhibits the expression of xCT and the uptake of cystine, which leads to ferroptosis and endothelial dysfunction. There is no doubt that the occurrence of endothelial dysfunction often increases the incidence of vasculitis and other symptoms [66, 67]. IL-1β and TNF can strongly induce highly active COX2 with low GPX4 activity, indicating that IL-1β is expected to become a vital target for the treatment of ferroptosis-related inflammation.
PUFA
Under oxidative stress, phospholipids and cholesterol esters containing PUFA in cell membranes and lipoproteins are easily oxidized by free radical-induced lipid peroxidation to form complex mixtures of oxidation products. A large body of evidence suggests that these oxidized lipids actively participate in the inflammatory response of atherosclerosis by interacting with immune cells (such as macrophages) and endothelial cells [68]. PUFA rich in Western diet plays an important role in the induction of inflammation, especially intestinal inflammation [3], PUFA-induced metabolic enteritis as a fuel for Crohn's Disease (CD) [69]. PUFA, such as AA, can be metabolized into bioactive lipid mediators through COX, LOX and cytochrome P450 enzymes, mediating the production of inflammatory cytokines in IECs and the balance of intestinal microbiota [3, 70]. Moreover, PUFA derived lipid mediators, such as AA and docosahexaenoic acid (DHA), are synthesized under stress and play a role as inflammatory activators [71]. However, studies have shown that increasing Omega-3 PUFA intake may reduce the risk of inflammatory storms [72].
In the process of lipid peroxidation, oxidants (such as ROS) attack lipid carbon double bonds (especially PUFA), indicating the importance of PUFA as a substrate of lipid peroxidation in ferroptosis [30]. ACSL4 is the key factor of sensitivity to ferroptosis, which can catalyze coenzyme A to promote the esterification of PUFA to phospholipids. This may also reveal a new combined therapeutic strategy, blocking ferroptosis by inhibiting ACSL4 and PUFA-ePL biosynthesis enzymes [24, 30].
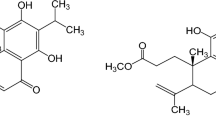
Metabolites of AA
AA, a 20-carbon fatty acid, is the main precursor of AA and an integral part of all cells [73]. The oxidation of PUFA to AA mediated by ALOX accelerates the occurrence of ferroptosis. COX, a bifunctional enzyme in line with dioxygenase and peroxidase, carries out complex free radical reactions and participates in the catalytic oxidation and cyclization of AA. Under the action of inflammatory stimulation, COX-2 is rapidly induced and acts at the inflammatory site to accelerate the inflammatory process [73, 74]. The state of these enzymes is directly affected by the redox state and peroxide tone in the cells. Peroxide hue refers to the steady-state level of cellular lipid hydroperoxide required for the final activation of LOX and COX. Therefore, this metabolic process is related to the regulation of GSH/GPX4 metabolism [73, 74]. Consistent with the production of PGs and leukotrienes during AA metabolism, PGs is expressed in a variety of cells and tissues, and widely regulates life activities. The formation of bioactive prostaglandins from PGH2 occurs through the action of a group of synthases expressed in a selective manner of tissue and cell type. These synthase include prostaglandin D synthase (PGDs), prostaglandin E synthase (PGEs), prostaglandin F synthase (PGFs), prostaglandin I synthase (PGIS) and thromboxane A synthase (txas), which form PGD2, PGE2 and PGF2 α, PGI2 (also known as prostacyclin) and TXA2. PGE2 and PGI2 are involved in many studies, including but not limited to enhancing vasodilation and edema formation. Furthermore, PGE2 is related to neuroinflammation and participates in allergic inflammation by regulating lymphocyte function. Patients with IBD also show elevated levels of PG and other AA derived eicosanoids in the inflammatory mucosa. In addition, leukotriene produced through PPAR γ-dependent mechanism up regulates the expression of COX-2, leading to the production of PGD2, thus forming a vicious circle of enhancing inflammatory response in a positive feedback way [74].
An important feature of ferroptosis-sensitive cells or ferroptosis-related cancer cells is the synthesis of a large number of oxidative lipid mediators. It was previously described that AA anchored in phosphatidylethanolamine is a target of LOX and can be enriched by ACSL4, thus being one of the major components of ferroptosis [75]. Relevant studies in gastric and colorectal cancer cells have shown that AA supplementation increases their susceptibility to ferroptosis [75]. Not hard to find, AA provides a mediator of the association between ferroptosis and inflammatory diseases. For example, GPX4, a key regulator of ferroptosis, helps promote resolution of inflammation by eliminating the oxide species produced by the AA metabolic network [76].
COX-2
I/R is the main cause of many inflammatory diseases and cell damage. At present, ferroptosis has been regarded as a new target for the treatment of I/R injury. COX-2/prostaglandin E2 (PGE2) pathway is closely related to I/R. COX-2 is regarded as a marker gene of ferroptosis, and the increase of its expression is considered to be an important sign of ferroptosis [77]. It has been reported that BMP4/ROS/COX-2 pathway is involved in cerebral ischemia/reperfusion injury (IRI), and the activation and recovery of this pathway can mediate the combination of ischemic preconditioning (IPC) and resveratrol (RES) to provide brain protection after I/R [78].
A study on SH-SY5Y cells showed that the activation of COX2/PGE2 pathway could reverse the reduction of iron accumulation and lipid peroxidation caused by EXSmir-137 co-incubation, and reduce the expression of GSH and GPX4 which represent the reverse of the inhibition of ferroptosis [79]. In addition, in brain I/R, the inhibition of ferroptosis by DFO can completely inactivate the synthase and degrading enzyme in COX-2/PGE2 pathway, and ultimately lead to the reduction of PGE2 [80]. Fer-1 reduced the increase of pro-inflammatory factors, including COX-2, while inhibiting ferroptosis in astrocytes [81].
Mitochondria
Mitochondria are important organelles involved in the regulation of energy metabolism, cell signal transduction and cell death pathways (including ferroptosis). Studies have shown that mitochondrial fatty acid metabolism genes, including citrate synthase (CS) and acyl CoA synthase family member 2 (ACSF2), may be necessary for ferroptosis induced by erastin [82]. Mitochondrial voltage dependent anion channel (VDAC) has been proved to be a potential target of erastin. The opening of VDAC leads to the production of mitochondrial ROS, the increase of mitochondrial potential, and then oxidative stress induces cell death [83].
Inhibition of mitochondrial TCA cycle or electron transfer chain (ETC) can reduce mitochondrial membrane potential hyperpolarization, lipid peroxidation accumulation and thus ferroptosis. The blocking of glutamine dissolution has the same inhibitory effect and can be offset by the provision of intermediates through the downstream TCA cycle. Similarly, the loss of function of fumarate hydratase (a tumor suppressor and TCA cycle component) makes people resistant to ferroptosis induced by cysteine deprivation [84].
The increase of mitochondrial ROS can induce the accumulation of lipid peroxidation. There is experimental evidence that activation of NRF2 can protect mitochondria, avoid mitochondrial damage and inflammation induced ROS accumulation, and regulate the occurrence of ferroptosis. The increase of active iron in mitochondria can lead to the accumulation of ROS during ferroptosis, so increasing mitochondrial iron storage may inhibit ferroptosis [83]. Consistent with this, mitochondrial ferritin (FTMT) is an iron storage protein. It is reported that FTMT regulates iron metabolism by regulating the redistribution of iron from mitochondria to cytoplasm and inhibits oxidative stress-dependent injury, especially in some high oxygen consuming tissues. FTMT can significantly inhibit the level of LIP, ROS and subsequent ferroptosis induced by erastin [85].
There are at least three mechanisms by which mitochondria damage or kill the host: ROS generation, pro-inflammatory signal or mitochondrial membrane permeability [86]. Some mitochondrial components may participate in the activation of PRRS by playing the role of PRR ligands to further stimulate the process of inflammatory response. In addition, four mitochondrial components, SMAC, N-formyl peptides, cardiolipin and cytochrome c, have been shown to promote inflammatory response [87]. Mitochondrial dysfunction and ROS production are closely related to the assembly and activation of inflammatory body NLRP3, and then affect the inflammatory process of intestinal inflammation and obesity induced inflammation [88,89,90,91]. In addition, the change of mitochondrial membrane permeability has become an important pro-inflammatory signal leading to inflammation through the release of mitochondrial DNA (mtDNA) and the down-regulation of apoptosis protein inhibitors (IAPS) [91]. It can’t be ignored that the transfer of mitochondria and mtDNA between cells can promote the spread of inflammation [92].
NF-κB
The transcription factor NF-κB is a nuclear factor that binds to an enhancer element of the activated B-cell immunoglobulin Kappa light chain (hence the abbreviation for NF-κB) [93]. It is a protein with specific DNA-binding activity that is expressed in almost all cell types and regulates many target genes with a wide variety of functions. Because NF-κB plays a key role in the expression of proinflammatory genes, including cytokines, chemokines, and adhesion molecules. NF-κB signaling is considered to be a typical proinflammatory signaling pathway. More and more evidence indicate that genes/drugs regulate the inflammatory response and reduce inflammatory damage by regulating NF-κB signaling pathway. In addition, NF-κB is involved in the regulation of iron metabolism pathway during inflammation. Transcription factor Spic in macrophages downregulates pro-inflammatory cytokines and promotes iron efflux by regulating FPN expression in activated macrophages [94]. Iron metabolism is an indispensable process in cell energy cycle, and the disturbance of its homeostasis may lead to inflammation. Targeting iron metabolism regulates NF-κB to regulate inflammatory response and plays a role in the prevention and treatment of inflammatory diseases [95]. Since iron metabolism is an important physiological process in ferroptosis, we hypothesized that ferroptosis links NF-κB with inflammation. In AKI, curcumin inhibits ferroptosis by inhibiting TLR4/NF-κB axis and activating HO-1, which further reduces inflammation and oxidative stress and plays a therapeutic role [96]. Therefore, NF-κB signaling pathway checkpoints may be important targets in the regulation of inflammatory diseases by targeting ferroptosis.
Liposomes
Liposomes, vesicles with an aqueous core entrapped in one or more lipid bilayers, are widely used as drug delivery systems. Liposomes can be used as delivery vehicles for a variety of drugs and biological agents, including small molecules, peptides, proteins, nucleic acids and vaccine antigens. Previous studies show that nanoliposomes can effectively target infected and inflamed tissue [97]. Sea cucumber saponin liposomes could effectively alleviate adipose tissue inflammation by reducing pro-inflammatory cytokine releases and macrophage infiltration [98]. In addition, folic acid and PEG conjugated Pae-loaded liposomes (PAE-LS) inhibited STAT1 phosphorylation, decreased the levels of proinflammatory cytokines (IL-1β, IL-6 and TNF-α) and iNOS expression, and significantly increased the levels of anti-inflammatory cytokines (IL-10) and CD206 by increasing p-STAT6, reduce the inflammatory response in RA [99]. Recently, it has been reported that Fer-1 liposomes can treat corneal injury caused by alkali burn by inhibiting ferroptosis, inflammation and neovascularization [100]. Based on the close relationship between ferroptosis and inflammation, Fer-1 liposomes are expected to become a therapeutic strategy for more inflammatory diseases. Because liposomes can be produced in large quantities with good production practices and stored for long periods at high antigen/vesicle mass ratios, there is great promise for future development of more liposomes to treat inflammatory diseases by targeting ferroptosis checkpoints.
The occurrence of ferroptosis promotes the generation of AAs, which is metabolized to generate PGs and so on under the action of LOX, COX2, and further promotes inflammatory responses. Mitochondrial ROS stimulates NLRP3 inflammatory corpuscles to promote inflammatory factor IL-1β, and inhibits the expression of anti-oxidation factor GPX4 at the same time, thus weakening the inflammatory reaction mediated by the activation of LOX and COX2 though GPX4. ROS stimulates the NRF2-Keap1 pathway, which in turn causes HO-1 to transfer from the nucleus to the cytoplasm and inhibits the inflammatory response.
Ferroptosis and inflammatory disease
AKI
AKI, formerly known as acute renal failure (ARF), is a common and critical disease caused by ischemia, nephrotoxic drugs, and urinary tract obstruction. An important feature of AKI is a rapid decline in renal function. However, the pathogenesis of AKI remains unclear, but it has long been recognized that one of the key factors is prolonged or excessive inflammation [110]. A large number of studies have shown that renal impairment can be slowed by suppressing inflammation in AKI, such as hydrogen sulfide [111], Gasdermin E [112] and Gypenoside XLIX [113]. In addition, early studies have shown that certain inflammatory cytokines can be used as therapeutic targets to reduce renal injury in AKI by inhibiting inflammation.
Significant advances have been made in the treatment of AKI in recent years, yet there are still no specific drugs developed to prevent and treat AKI. The underlying role of ferroptosis in AKI has attracted widespread attention, and recent findings suggest that ferroptosis is a potential avenue for the treatment of AKI. Changes in various ferroptosis metabolic sensors were observed in cisplatin-induced AKI models, including lipid peroxidation, GPX4 activity, NADPH and reduced GSH levels, and ferritinophagy [114]. Ferroptosis inhibitors have anti-inflammatory effects in AKI. In a mouse model of oxalate-induced AKI, Fer-1 alleviates neutrophil infiltration and pro-inflammatory cytokine release [115]. Irisin attenuated renal injury in AKI by upregulating GPX4 downregulated the inflammatory response and inhibited ferroptosis [116]. In addition, it has been shown that curcumin can reduce renal injury in AKI by inhibiting ferroptosis in renal tubular epithelial cells [116]. How ferroptosis participates in the pathogenesis of AKI is still a mystery. Studies have reported that cells with ferroptosis can recruit macrophages and stimulate macrophages to recruit neutrophils, thereby causing an inflammatory cascade of AKI [117]. Future exploration by targeting ferroptosis in AKI may be a major breakthrough in the treatment of AKI.
ALI
Acute lung injury/acute respiratory distress syndrome (ALI/ARDS) is a common and critical disease caused by infection, trauma, radiotherapy, ischemia reperfusion and other factors. The pathogenesis of ALI was previously thought to be related to oxidative stress, apoptosis, inflammation and hypoxia. Recent studies suggest that ferroptosis may be involved in the development and progression of ALI, and targeting the ferroptosis pathway has become an important approach for the treatment of ALI. AUF1 inhibits ferroptosis and attenuates sepsis-induced ALI by regulating NRF2 and ATF3 [118]. Panaxydol inhibits ferroptosis and inflammatory response through the Keap1-NRF2/HO-1 pathway that attenuated LPS-induced ALI in mice [119]. Astaxanthin attenuates ferroptosis via Keap1-NRF2/HO-1 signaling pathways in LPS-induced ALI [120]. In addition, it has also been shown that isoliquiritin apioside attenuates ALI induced by intestinal I/R by blocking HIF-1α mediated ferroptosis [121]. All these studies suggest that ferroptosis is involved in the development of ALI disease pathology. Ferroptosis may regulate ALI through neutrophil extracellular traps mediate m6A modification [122]. The future development of additional drugs or potential targets is essential for the treatment of ALI by targeting ferroptosis.
IBD
IBD is a family of chronic autoimmune diseases of the gastrointestinal tract that includes CD and ulcerative colitis (UC). Symptoms can manifest as intermittent relapses and quiescent inflammatory remissions. It is well known that inflammation caused by an abnormal immune system response in the intestinal mucosa plays an important role in the pathogenesis of IBD. Ferroptosis has been reported to be associated with intestinal epithelial cell death, research shows that STAT3-mediated ferroptosis is involved in the pathogenesis of UC [123]. Moreover, ferroptosis is involved in intestinal epithelial cell death in UC via endoplasmic reticulum stress [124]. Pharmacological inhibition of MELK significantly alleviates the inflammatory response and reduces intestinal injury in mice with colitis. Among them, the MELK inhibitor OTSSP167 significantly inhibited ferroptosis in intestinal tissues, suppressed macrophage infiltration and M1 polarization, and reduced the secretion of pro-inflammatory factors [125]. A study has shown that intestinal epithelial cells in CD showed impaired GPX4 activity and ferroptosis. The diet is rich in ω-6-PUFA-AA, which increases the risk of IBD [3]. In the future, finding more biomarkers of IBD ferroptosis has great prospects for the treatment of IBD.
Brain and neurodegenerative diseases
Neurodegenerative diseases are a kind of chronic progressive degeneration and loss of neurons in the brain and spinal cord. Major diseases include Parkinson's disease (PD), Alzheimer's disease (AD), Huntington's disease (HD), etc. Iron is essential to the physiology of all tissues in the body. However, in some cases, it can be harmful, especially to the brain. Although cellular metabolism in the central nervous system requires iron as a REDOX metal for energy production and primary ATP production, neural tissue is vulnerable to oxidative damage from excess iron and the reduction of antioxidant systems. Due to the lack of specific biomarkers, several factors that may be involved in the ferroptosis process and prevent the unambiguous recognition of iron in the body. However, there is substantial evidence that ferroptosis is associated with the pathophysiology of neurodegenerative changes. Ferroptosis involves the accumulation of iron in the brain, consumption of GSH, and lipid peroxidation, while triggering a series of events including inflammatory activation, neurotransmitter oxidation, neuronal communication failure, myelin degeneration, astrocyte dysplasia, dementia, and cell death. Iron or free iron overload can trigger lipid peroxidation in neurons, astrocytes, oligodendrocytes, microglias, and Schwann cells [126]. In addition, low activity of the GPX4 and GSH systems has been shown to be associated with ferroptosis in motor neurodegeneration. The level of endogenous α-synuclein can determine the sensitivity of dopaminergic neurons to ferroptosis, by regulating the composition of ether phospholipid membrane [127]. In AD, ferroptosis may induce iron homeostasis disorder by downregulating FPN, and excess iron exacerbates oxidative damage and cognitive defects [128]. This suggests that the use of iron chelators (DFO) and ferroptosis inhibitors may be an alternative approach to the treatment of neurodegenerative diseases.
IRI
I/R is a pathological process that occurs in numerous organs throughout the human body, and it is frequently associated with severe cellular damage and death. Recently it has emerged that ferroptosis plays a significant detrimental role in many I/R models. Myocardial reperfusion injury, also known as lethal reperfusion injury, results in the death of cardiac myocytes, which are viable before reperfusion. The destruction of viable cardiac myocytes upon reperfusion ensures that the rate of death or cardiac failure is still high, even with optimally controlled myocardial reperfusion. Clinical studies indicate that residual myocardial iron is a risk factor for inadequate left ventricular remodeling after reperfusion [129]. Notably, evidence indicates that the mitochondria-specific overexpression of GPX4 in mitochondria alleviates cardiac dysfunction following I/R [130]. Inhibition of glutaminolysis, a component of the GSH generation pathway, can also attenuate I/R-associated heart injury by blocking ferroptosis. The cardiac mechanistic target of rapamycin (mTOR) protects the heart against IRI and was found to exert protective effects against excess iron and ferroptosis. Fer-1 and iron chelation can also ameliorate heart failure induced by both acute and chronic I/R [131], consistent with the notion that targeting ferroptosis can serve as a potential strategy to prevent cardiomyopathy. A recent study found that inhibition of ferroptosis reduced endoplasmic reticulum damage and myocardial damage. At the same time, inhibition of endoplasmic reticulum can reduce ferroptosis and cell damage [132]. Tissue pigment (HC), with an effective antioxidant component and iron chelating capacity, is now used in clinical practice. However, data on HC's protective effect on ferroptosis in myocardial I/R injury are limited. A recent study found that early myocardial intervention prior to reperfusion can salvage myocardial I/R injury by preventing ferroptosis. Therefore, HC is a promising treatment option to provide secondary cardiac protection for patients undergoing coronary reperfusion therapy [133].
Indeed, there are many gaps in the specific mechanisms of ferroptosis involved in inflammatory diseases. The future development of more drugs, targets or mechanisms that target ferroptosis in inflammatory diseases could help in the treatment of inflammatory diseases, and targeting ferroptosis could be the dawn of treatment for inflammatory diseases (Table 2).
Conclusions and perspectives
The susceptibility to ferroptosis is closely linked to cellular metabolism (especially lipids, iron and amino acids), which involves a complex network structure. This also provides a possible and involvement of ferroptosis in the development of various diseases. As inflammation is present in various human diseases, further studies on the interaction between ferroptosis and the immune system are needed in the future. Regulation of ferroptosis is considered to be an effective intervention strategy for the prevention and treatment of inflammatory diseases. Damage-associated molecular patterns (DAMPs) are immune mediators of various types of regulatory cell death (RCD) [30]. HMGB1 (high mobility group box 1) is a typical DAMP that is released by ferroptosis cells and drives inflammation by activating macrophages to produce pro-inflammatory cytokines [167]. This suggests that pharmacological induction of ferroptosis is a promising means of treating inflammatory diseases. However, the establishment of drug targets, active ingredients, potential side effects, pharmacokinetic studies, and preclinical toxicology studies are all urgent problems to be solved. In addition, how to control the side effects of ferroptosis regulation in preclinical studies and patient clinical trials is also a potential problem.
There is increasing evidence of cross-talk between various cell death modes, such as ferroptosis, apoptosis and autophagy. Studies have shown that hesperidin can alleviate cisplatin-induced AKI by reducing oxidative stress, inflammation and apoptosis [168]. This suggests that ferroptosis and apoptosis play a synergistic role in AKI, and inhibition of ferroptosis and apoptosis can exert the greatest protective effect. Some factors are involved in both apoptosis and ferroptosis control, such as P53. P53 is a tumor suppressor that can be stimulated by apoptosis stimulating proteins to induce apoptosis. In addition, P53 can also regulate ferroptosis by regulating SLC7A11. Autophagy is a protective physiological process that phagocytoses metabolites produced by cells under pressure such as starvation and hypoxia, and protects cells from the effects of these harmful metabolites. However, NCOA4-mediated ferritinophagy can induce ferroptosis by promoting ferritin degradation. This suggests that autophagy plays an essential role in the regulation of cell ferroptosis. Therefore, therapy combining ferroptosis inhibitors and autophagy or apoptosis inhibitors may provide a potential therapeutic strategy for treating inflammatory diseases, but the mechanisms underlying the interaction between ferroptosis and other cell death modes require further investigation.
In this review, we summarize the molecular mechanisms of ferroptosis and the possible mechanisms of ferroptosis involved in inflammation and inflammatory diseases. Ferroptosis is considered as a target for the treatment of inflammatory diseases. The development of more ferroptosis inhibitors or drugs targeting ferroptosis will greatly improve the therapeutic effect of inflammatory diseases. However, practical applications still face many difficulties. First, it is difficult to determine whether the effects of ferroptosis inhibitors or drugs that target ferroptosis are specific to a particular class of inflammatory diseases with unique characteristics or are generally applicable to most inflammatory diseases. Since the specific mechanisms by which ferroptosis is involved in various inflammatory diseases have not been fully elucidated, a deeper understanding of the mechanisms associated with ferroptosis and inflammation will help to achieve this goal. Second, besides inflammatory diseases, ferroptosis is associated with pathological cell death associated with a variety of diseases, such as cancer. While avoiding systemic adverse reactions, it is particularly important to develop specific treatments that inhibit ferroptosis in inflammatory diseases. Third, there is still a lack of ferroptosis biomarkers for specific inflammatory diseases. Exploring appropriate biomarkers will further promote the development of research and treatment of various inflammatory diseases in vivo and in vitro. Fourth, even though targeting ferroptosis is considered a promising approach for the treatment of inflammatory diseases, the crosstalk between ferroptosis and other forms of cell deaths makes the treatment of ferroptosis-specific inhibitors targeting inflammatory diseases limited and resistant. Can combination of ferroptosis inhibitors with other cell death inhibitors improve the efficacy of inflammatory diseases? To address this issue, further exploration of the link between ferroptosis, inflammatory diseases, and other types of cell death will be necessary in the future. Last but not least, although selective inhibition of ferroptosis has been shown to significantly improve inflammatory diseases in a variety of animal models, no clinical trials using specific inhibitors of ferroptosis have been conducted to date. More population-based data are urgently needed to determine whether selective blocking of ferroptosis can improve the prognosis of inflammatory diseases in clinical settings.
Data availability
Not available.
References
Tang D, Chen X, Kang R, Kroemer G. Ferroptosis: Molecular mechanisms and health implications. Cell Res. 2021;31:107–25.
Martin-Sanchez D, Ruiz-Andres O, Poveda J, Carrasco S, Cannata-Ortiz P, Sanchez-Niño MD, Ruiz Ortega M, Egido J, Linkermann A, Ortiz A, Sanz AB. Ferroptosis, but not necroptosis, is important in nephrotoxic folic acid-induced AKI. J Am Soc Nephrol. 2017;28:218–29.
Mayr L, Grabherr F, Schwärzler J, Reitmeier I, Sommer F, Gehmacher T, Niederreiter L, He GW, Ruder B, Kunz KTR, Tymoszuk P, Hilbe R, Haschka D, Feistritzer C, Gerner RR, Enrich B, Przysiecki N, Seifert M, Keller MA, Oberhuber G, Sprung S, Ran Q, Koch R, Effenberger M, Tancevski I, Zoller H, Moschen AR, Weiss G, Becker C, Rosenstiel P, Kaser A, Tilg H, Adolph TE. Dietary lipids fuel GPX4-restricted enteritis resembling Crohn’s disease. Nat Commun. 2020;11:1775.
Karin M, Shalapour S. Regulation of antitumor immunity by inflammation-induced epigenetic alterations. Cell Mol Immunol. 2022;19:59–66.
Zhong F, Liang S, Zhong Z. emerging role of mitochondrial DNA as a major driver of inflammation and disease progression. Trends Immunol. 2019;40:1120–33.
Cooke JP. Inflammation and its role in regeneration and repair. Circ Res. 2019;124:1166–8.
Sun Y, Chen P, Zhai B, Zhang M, Xiang Y, Fang J, Xu S, Gao Y, Chen X, Sui X, Li G. The emerging role of ferroptosis in inflammation. Biomed Pharmacother. 2020;127: 110108.
Liu P, Feng Y, Li H, Chen X, Wang G, Xu S, Li Y, Zhao L. Ferrostatin-1 alleviates lipopolysaccharide-induced acute lung injury via inhibiting ferroptosis. Cell Mol Biol Lett. 2020;25:10.
Kong Z, Liu R, Cheng Y. Artesunate alleviates liver fibrosis by regulating ferroptosis signaling pathway. Biomed Pharmacother. 2019;109:2043–53.
Kühn LC. Iron regulatory proteins and their role in controlling iron metabolism. Metallomics. 2015;7:232–43.
Anderson CP, Shen M, Eisenstein RS, Leibold EA. Mammalian iron metabolism and its control by iron regulatory proteins. Biochim Biophys Acta. 1823;2012:1468–83.
Zhang DL, Ghosh MC, Rouault TA. The physiological functions of iron regulatory proteins in iron homeostasis—an update. Front Pharmacol. 2014;5:124.
Yu Y, Jiang L, Wang H, Shen Z, Cheng Q, Zhang P, Wang J, Wu Q, Fang X, Duan L, Wang S, Wang K, An P, Shao T, Chung RT, Zheng S, Min J, Wang F. Hepatic transferrin plays a role in systemic iron homeostasis and liver ferroptosis. Blood. 2020;136:726–39.
Bogdan AR, Miyazawa M, Hashimoto K, Tsuji Y. Regulators of iron homeostasis: new players in metabolism, cell death, and disease. Trends Biochem Sci. 2016;41:274–86.
Xing G, Meng L, Cao S, Liu S, Wu J, Li Q, Huang W, Zhang L. PPARα alleviates iron overload-induced ferroptosis in mouse liver. EMBO Rep. 2022;23: e52280.
Yamada N, Karasawa T, Wakiya T, Sadatomo A, Ito H, Kamata R, Watanabe S, Komada T, Kimura H, Sanada Y, Sakuma Y, Mizuta K, Ohno N, Sata N, Takahashi M. Iron overload as a risk factor for hepatic ischemia-reperfusion injury in liver transplantation: potential role of ferroptosis. Am J Transplant. 2020;20:1606–18.
Sun X, Ou Z, Xie M, Kang R, Fan Y, Niu X, Wang H, Cao L, Tang D. HSPB1 as a novel regulator of ferroptotic cancer cell death. Oncogene. 2015;34:5617–25.
Chen GQ, Benthani FA, Wu J, Liang D, Bian ZX, Jiang X. Artemisinin compounds sensitize cancer cells to ferroptosis by regulating iron homeostasis. Cell Death Differ. 2020;27:242–54.
Han S, Lin F, Qi Y, Liu C, Zhou L, Xia Y, Chen K, Xing J, Liu Z, Yu W, Zhang Y, Zhou X, Rao T, Cheng F. HO-1 contributes to luteolin-triggered ferroptosis in clear cell renal cell carcinoma via increasing the labile iron pool and promoting lipid peroxidation. Oxid Med Cell Longev. 2022;2022:3846217.
Que X, Hung MY, Yeang C, Gonen A, Prohaska TA, Sun X, Diehl C, Määttä A, Gaddis DE, Bowden K, Pattison J, MacDonald JG, Ylä-Herttuala S, Mellon PL, Hedrick CC, Ley K, Miller YI, Glass CK, Peterson KL, Binder CJ, Tsimikas S, Witztum JL. Oxidized phospholipids are proinflammatory and proatherogenic in hypercholesterolaemic mice. Nature. 2018;558:301–6.
Ribas V, García-Ruiz C, Fernández-Checa JC. Glutathione and mitochondria. Front Pharmacol. 2014;5:151.
Dodson M, Castro-Portuguez R, Zhang DD. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23: 101107.
Zou Y, Li H, Graham ET, Deik AA, Eaton JK, Wang W, Sandoval-Gomez G, Clish CB, Doench JG, Schreiber SL. Cytochrome P450 oxidoreductase contributes to phospholipid peroxidation in ferroptosis. Nat Chem Biol. 2020;16:302–9.
Zou Y, Henry WS, Ricq EL, Graham ET, Phadnis VV, Maretich P, Paradkar S, Boehnke N, Deik AA, Reinhardt F, Eaton JK, Ferguson B, Wang W, Fairman J, Keys HR, Dančík V, Clish CB, Clemons PA, Hammond PT, Boyer LA, Weinberg RA, Schreiber SL. Plasticity of ether lipids promotes ferroptosis susceptibility and evasion. Nature. 2020;585:603–8.
Cui W, Liu D, Gu W, Chu B. Peroxisome-driven ether-linked phospholipids biosynthesis is essential for ferroptosis. Cell Death Differ. 2021;28:2536–51.
Toyokuni S, Ito F, Yamashita K, Okazaki Y, Akatsuka S. Iron and thiol redox signaling in cancer: an exquisite balance to escape ferroptosis. Free Radic Biol Med. 2017;108:610–26.
Yang WS, Kim KJ, Gaschler MM, Patel M, Shchepinov MS, Stockwell BR. Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc Natl Acad Sci U S A. 2016;113:E4966-4975.
Liu J, Kang R, Tang D (2021) Signaling pathways and defense mechanisms of ferroptosis. FEBS J
Tang D, Kang R, Berghe TV, Vandenabeele P, Kroemer G. The molecular machinery of regulated cell death. Cell Res. 2019;29:347–64.
Chen X, Li J, Kang R, Klionsky DJ, Tang D. Ferroptosis: machinery and regulation. Autophagy. 2021;17:2054–81.
Badgley MA, Kremer DM, Maurer HC, DelGiorno KE, Lee HJ, Purohit V, Sagalovskiy IR, Ma A, Kapilian J, Firl CEM, Decker AR, Sastra SA, Palermo CF, Andrade LR, Sajjakulnukit P, Zhang L, Tolstyka ZP, Hirschhorn T, Lamb C, Liu T, Gu W, Seeley ES, Stone E, Georgiou G, Manor U, Iuga A, Wahl GM, Stockwell BR, Lyssiotis CA, Olive KP. Cysteine depletion induces pancreatic tumor ferroptosis in mice. Science. 2020;368:85–9.
Doll S, Freitas FP, Shah R, Aldrovandi M, da Silva MC, Ingold I, Goya Grocin A, Xavier da Silva TN, Panzilius E, Scheel CH, Mourão A, Buday K, Sato M, Wanninger J, Vignane T, Mohana V, Rehberg M, Flatley A, Schepers A, Kurz A, White D, Sauer M, Sattler M, Tate EW, Schmitz W, Schulze A, O’Donnell V, Proneth B, Popowicz GM, Pratt DA, Angeli JPF, Conrad M. FSP1 is a glutathione-independent ferroptosis suppressor. Nature. 2019;575:693–8.
Bersuker K, Hendricks JM, Li Z, Magtanong L, Ford B, Tang PH, Roberts MA, Tong B, Maimone TJ, Zoncu R, Bassik MC, Nomura DK, Dixon SJ, Olzmann JA. The CoQ oxidoreductase FSP1 acts parallel to GPX4 to inhibit ferroptosis. Nature. 2019;575:688–92.
Kraft VAN, Bezjian CT, Pfeiffer S, Ringelstetter L, Müller C, Zandkarimi F, Merl-Pham J, Bao X, Anastasov N, Kössl J, Brandner S, Daniels JD, Schmitt-Kopplin P, Hauck SM, Stockwell BR, Hadian K, Schick JA. GTP cyclohydrolase 1/tetrahydrobiopterin counteract ferroptosis through lipid remodeling. ACS Cent Sci. 2020;6:41–53.
Dai E, Zhang W, Cong D, Kang R, Wang J, Tang D. AIFM2 blocks ferroptosis independent of ubiquinol metabolism. Biochem Biophys Res Commun. 2020;523:966–71.
Wei R, Zhao Y, Wang J, Yang X, Li S, Wang Y, Yang X, Fei J, Hao X, Zhao Y, Gui L, Ding X. Tagitinin C induces ferroptosis through PERK-Nrf2-HO-1 signaling pathway in colorectal cancer cells. Int J Biol Sci. 2021;17:2703–17.
Zhu X, Guo F, Tang H, Huang C, Xie G, Huang T, Li Y, Liu C, Wang H, Chen B. Islet transplantation attenuating testicular injury in type 1 diabetic rats is associated with suppression of oxidative stress and inflammation via Nrf-2/HO-1 and NF-κB pathways. J Diabetes Res. 2019;2019:8712492.
Schipper HM, Song W, Tavitian A, Cressatti M. The sinister face of heme oxygenase-1 in brain aging and disease. Prog Neurobiol. 2019;172:40–70.
Campbell MR, Karaca M, Adamski KN, Chorley BN, Wang X, Bell DA. Novel hematopoietic target genes in the NRF2-mediated transcriptional pathway. Oxid Med Cell Longev. 2013;2013: 120305.
Ge MH, Tian H, Mao L, Li DY, Lin JQ, Hu HS, Huang SC, Zhang CJ, Mei XF. Zinc attenuates ferroptosis and promotes functional recovery in contusion spinal cord injury by activating Nrf2/GPX4 defense pathway. CNS Neurosci Ther. 2021;27:1023–40.
Medzhitov R. The spectrum of inflammatory responses. Science. 2021;374:1070–5.
Serhan CN, Levy BD. Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. J Clin Investig. 2018;128:2657–69.
Wojtulewicz K, Krawczyńska A, Tomaszewska-Zaremba D, Wójcik M, Herman AP. Effect of acute and prolonged inflammation on the gene expression of proinflammatory cytokines and their receptors in the anterior pituitary gland of ewes. Int J Mol Sci. 2020;21:6939.
Zhang Z, Tang J, Song J, Xie M, Liu Y, Dong Z, Liu X, Li X, Zhang M, Chen Y, Shi H, Zhong J. Elabela alleviates ferroptosis, myocardial remodeling, fibrosis and heart dysfunction in hypertensive mice by modulating the IL-6/STAT3/GPX4 signaling. Free Radic Biol Med. 2022;181:130–42.
Yang L, Guo J, Yu N, Liu Y, Song H, Niu J, Gu Y. Tocilizumab mimotope alleviates kidney injury and fibrosis by inhibiting IL-6 signaling and ferroptosis in UUO model. Life Sci. 2020;261: 118487.
Wang C, Yuan W, Hu A, Lin J, Xia Z, Yang CF, Li Y, Zhang Z. Dexmedetomidine alleviated sepsis-induced myocardial ferroptosis and septic heart injury. Mol Med Rep. 2020;22:175–84.
Yao X, Huang J, Zhong H, Shen N, Faggioni R, Fung M, Yao Y. Targeting interleukin-6 in inflammatory autoimmune diseases and cancers. Pharmacol Ther. 2014;141:125–39.
Bin S, Xin L, Lin Z, Jinhua Z, Rui G, Xiang Z. Targeting miR-10a-5p/IL-6R axis for reducing IL-6-induced cartilage cell ferroptosis. Exp Mol Pathol. 2021;118: 104570.
Yang L, Wang H, Yang X, Wu Q, An P, Jin X, Liu W, Huang X, Li Y, Yan S, Shen S, Liang T, Min J, Wang F. Auranofin mitigates systemic iron overload and induces ferroptosis via distinct mechanisms. Signal Transduct Target Ther. 2020;5:138.
Hirano T. IL-6 in inflammation, autoimmunity and cancer. Int Immunol. 2021;33:127–48.
Liao S, Apaijai N, Luo Y, Wu J, Chunchai T, Singhanat K, Arunsak B, Benjanuwattra J, Chattipakorn N, Chattipakorn SC. Cell death inhibitors protect against brain damage caused by cardiac ischemia/reperfusion injury. Cell Death Discov. 2021;7:312.
Zelová H, Hošek J. TNF-α signalling and inflammation: interactions between old acquaintances. Inflamm Res. 2013;62:641–51.
Wang Y, Zhang H, Chen Q, Jiao F, Shi C, Pei M, Lv J, Zhang H, Wang L, Gong Z. TNF-α/HMGB1 inflammation signalling pathway regulates pyroptosis during liver failure and acute kidney injury. Cell Prolif. 2020;53: e12829.
Davizon-Castillo P, McMahon B, Aguila S, Bark D, Ashworth K, Allawzi A, Campbell RA, Montenont E, Nemkov T, D’Alessandro A, Clendenen N, Shih L, Sanders NA, Higa K, Cox A, Padilla-Romo Z, Hernandez G, Wartchow E, Trahan GD, Nozik-Grayck E, Jones K, Pietras EM, DeGregori J, Rondina MT, Di Paola J. TNF-α-driven inflammation and mitochondrial dysfunction define the platelet hyperreactivity of aging. Blood. 2019;134:727–40.
Oh BM, Lee SJ, Park GL, Hwang YS, Lim J, Park ES, Lee KH, Kim BY, Kwon YT, Cho HJ, Lee HG. Erastin inhibits septic shock and inflammatory gene expression via suppression of the NF-κB pathway. J Clin Med. 2019;8:2210.
Ma D, Li C, Jiang P, Jiang Y, Wang J, Zhang D. Inhibition of ferroptosis attenuates acute kidney injury in rats with severe acute pancreatitis. Dig Dis Sci. 2021;66:483–92.
Xiao Z, Kong B, Fang J, Qin T, Dai C, Shuai W, Huang H. Ferrostatin-1 alleviates lipopolysaccharide-induced cardiac dysfunction. Bioengineered. 2021;12:9367–76.
Friedmann Angeli JP, Krysko DV, Conrad M. Ferroptosis at the crossroads of cancer-acquired drug resistance and immune evasion. Nat Rev Cancer. 2019;19:405–14.
Lopez-Castejon G, Brough D. Understanding the mechanism of IL-1β secretion. Cytokine Growth Factor Rev. 2011;22:189–95.
Huang Y, Xu W, Zhou R. NLRP3 inflammasome activation and cell death. Cell Mol Immunol. 2021;18:2114–27.
Fu JJ, McDonald VM, Baines KJ, Gibson PG. Airway IL-1β and systemic inflammation as predictors of future exacerbation risk in asthma and COPD. Chest. 2015;148:618–29.
Lee CH, Chiang CF, Kuo FC, Su SC, Huang CL, Liu JS, Lu CH, Hsieh CH, Wang CC, Lee CH, Shen PH. High-molecular-weight hyaluronic acid inhibits IL-1β-induced synovial inflammation and macrophage polarization through the GRP78-NF-κB signaling pathway. Int J Mol Sci. 2021;22:11917.
Chen Q, Liu X, Wang D, Zheng J, Chen L, Xie Q, Liu X, Niu S, Qu G, Lan J, Li J, Yang C, Zou D. Periodontal inflammation-triggered by periodontal ligament stem cell pyroptosis exacerbates periodontitis. Front Cell Dev Biol. 2021;9: 663037.
Lopez-Rodriguez AB, Hennessy E, Murray CL, Nazmi A, Delaney HJ, Healy D, Fagan SG, Rooney M, Stewart E, Lewis A, de Barra N, Scarry P, Riggs-Miller L, Boche D, Cunningham MO, Cunningham C. Acute systemic inflammation exacerbates neuroinflammation in Alzheimer’s disease: IL-1β drives amplified responses in primed astrocytes and neuronal network dysfunction. Alzheimers Dement. 2021;17:1735–55.
Shen Y, Malik SA, Amir M, Kumar P, Cingolani F, Wen J, Liu Y, Zhao E, Farris AB, Raeman R, Czaja MJ. Decreased hepatocyte autophagy leads to synergistic IL-1β and TNF mouse liver injury and inflammation. Hepatology. 2020;72:595–608.
Yao X, Sun K, Yu S, Luo J, Guo J, Lin J, Wang G, Guo Z, Ye Y, Guo F. Chondrocyte ferroptosis contribute to the progression of osteoarthritis. J Orthop Transl. 2021;27:33–43.
Luo EF, Li HX, Qin YH, Qiao Y, Yan GL, Yao YY, Li LQ, Hou JT, Tang CC, Wang D. Role of ferroptosis in the process of diabetes-induced endothelial dysfunction. World J Diabetes. 2021;12:124–37.
Zhong S, Li L, Shen X, Li Q, Xu W, Wang X, Tao Y, Yin H. An update on lipid oxidation and inflammation in cardiovascular diseases. Free Radic Biol Med. 2019;144:266–78.
Schwärzler J, Mayr L, Vich Vila A, Grabherr F, Niederreiter L, Philipp M, Grander C, Meyer M, Jukic A, Tröger S, Enrich B, Przysiecki N, Tschurtschenthaler M, Sommer F, Kronberger I, Koch J, Hilbe R, Hess MW, Oberhuber G, Sprung S, Ran Q, Koch R, Effenberger M, Kaneider NC, Wieser V, Keller MA, Weersma RK, Aden K, Rosenstiel P, Blumberg RS, Kaser A, Tilg H, Adolph TE. PUFA-induced metabolic enteritis as a fuel for Crohn’s disease. Gastroenterology. 2022;162:1690–704.
Cândido FG, Valente FX, Grześkowiak M, Moreira APB, Rocha D, Alfenas RCG. Impact of dietary fat on gut microbiota and low-grade systemic inflammation: mechanisms and clinical implications on obesity. Int J Food Sci Nutr. 2018;69:125–43.
Ajabnoor SM, Thorpe G, Abdelhamid A, Hooper L. Long-term effects of increasing omega-3, omega-6 and total polyunsaturated fats on inflammatory bowel disease and markers of inflammation: a systematic review and meta-analysis of randomized controlled trials. Eur J Nutr. 2021;60:2293–316.
Artiach G, Carracedo M, Plunde O, Wheelock CE, Thul S, Sjövall P, Franco-Cereceda A, Laguna-Fernandez A, Arnardottir H, Bäck M. Omega-3 polyunsaturated fatty acids decrease aortic valve disease through the resolvin E1 and ChemR23 axis. Circulation. 2020;142:776–89.
Bennett M, Gilroy DW. Lipid mediators in inflammation. Microbiol Spectr. 2016;4:343–66.
Raphael W, Sordillo LM. Dietary polyunsaturated fatty acids and inflammation: the role of phospholipid biosynthesis. Int J Mol Sci. 2013;14:21167–88.
Lee JY, Nam M, Son HY, Hyun K, Jang SY, Kim JW, Kim MW, Jung Y, Jang E, Yoon SJ, Kim J, Kim J, Seo J, Min JK, Oh KJ, Han BS, Kim WK, Bae KH, Song J, Kim J, Huh YM, Hwang GS, Lee EW, Lee SC. Polyunsaturated fatty acid biosynthesis pathway determines ferroptosis sensitivity in gastric cancer. Proc Natl Acad Sci U S A. 2020;117:32433–42.
Li C, Deng X, Xie X, Liu Y, Friedmann Angeli JP, Lai L. Activation of glutathione peroxidase 4 as a novel anti-inflammatory strategy. Front Pharmacol. 2018;9:1120.
Chen B, Chen Z, Liu M, Gao X, Cheng Y, Wei Y, Wu Z, Cui D, Shang H. Inhibition of neuronal ferroptosis in the acute phase of intracerebral hemorrhage shows long-term cerebroprotective effects. Brain Res Bull. 2019;153:122–32.
Yan Y, Tong F, Chen J. Endogenous BMP-4/ROS/COX-2 mediated IPC and resveratrol alleviated brain damage. Curr Pharm Des. 2019;25:1030–9.
Li Y, Wang J, Chen S, Wu P, Xu S, Wang C, Shi H, Bihl J. miR-137 boosts the neuroprotective effect of endothelial progenitor cell-derived exosomes in oxyhemoglobin-treated SH-SY5Y cells partially via COX2/PGE2 pathway. Stem Cell Res Ther. 2020;11:330.
Xu Y, Liu Y, Li K, Yuan D, Yang S, Zhou L, Zhao Y, Miao S, Lv C, Zhao J. COX-2/PGE2 pathway inhibits the ferroptosis induced by cerebral ischemia reperfusion. Mol Neurobiol. 2022;59:1619–31.
Li S, Zhou C, Zhu Y, Chao Z, Sheng Z, Zhang Y, Zhao Y. Ferrostatin-1 alleviates angiotensin II (Ang II)-induced inflammation and ferroptosis in astrocytes. Int Immunopharmacol. 2021;90: 107179.
Xu T, Ding W, Ji X, Ao X, Liu Y, Yu W, Wang J. Molecular mechanisms of ferroptosis and its role in cancer therapy. J Cell Mol Med. 2019;23:4900–12.
Wang H, Liu C, Zhao Y, Gao G. Mitochondria regulation in ferroptosis. Eur J Cell Biol. 2020;99: 151058.
Gao M, Yi J, Zhu J, Minikes AM, Monian P, Thompson CB, Jiang X. Role of mitochondria in ferroptosis. Mol Cell. 2019;73:354-363.e353.
Wang P, Cui Y, Ren Q, Yan B, Zhao Y, Yu P, Gao G, Shi H, Chang S, Chang YZ. Mitochondrial ferritin attenuates cerebral ischaemia/reperfusion injury by inhibiting ferroptosis. Cell Death Dis. 2021;12:447.
Green DR, Galluzzi L, Kroemer G. Mitochondria and the autophagy-inflammation-cell death axis in organismal aging. Science. 2011;333:1109–12.
Marchi S, Guilbaud E, Tait SWG, Yamazaki T, Galluzzi L (2022) Mitochondrial control of inflammation. Nat Rev Immunol 1–15
Missiroli S, Patergnani S, Caroccia N, Pedriali G, Perrone M, Previati M, Wieckowski MR, Giorgi C. Mitochondria-associated membranes (MAMs) and inflammation. Cell Death Dis. 2018;9:329.
Cosin-Roger J, Simmen S, Melhem H, Atrott K, Frey-Wagner I, Hausmann M, de Vallière C, Spalinger MR, Spielmann P, Wenger RH, Zeitz J, Vavricka SR, Rogler G, Ruiz PA. Hypoxia ameliorates intestinal inflammation through NLRP3/mTOR downregulation and autophagy activation. Nat Commun. 2017;8:98.
Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, Ravussin E, Stephens JM, Dixit VD. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17:179–88.
Deng Y, Xie M, Li Q, Xu X, Ou W, Zhang Y, Xiao H, Yu H, Zheng Y, Liang Y, Jiang C, Chen G, Du D, Zheng W, Wang S, Gong M, Chen Y, Tian R, Li T. Targeting mitochondria-inflammation circuit by β-hydroxybutyrate mitigates HFpEF. Circ Res. 2021;128:232–45.
Riley JS, Tait SW. Mitochondrial DNA in inflammation and immunity. EMBO Rep. 2020;21: e49799.
Hoesel B, Schmid JA. The complexity of NF-κB signaling in inflammation and cancer. Mol Cancer. 2013;12:86.
Alam Z, Devalaraja S, Li M, To TKJ, Folkert IW, Mitchell-Velasquez E, Dang MT, Young P, Wilbur CJ, Silverman MA, Li X, Chen YH, Hernandez PT, Bhattacharyya A, Bhattacharya M, Levine MH, Haldar M. Counter regulation of spic by NF-κB and STAT signaling controls inflammation and iron metabolism in macrophages. Cell Rep. 2020;31: 107825.
Kang DY, Sp N, Jo ES, Lee JM, Jang KJ. New insights into the pivotal role of iron/heme metabolism in TLR4/NF-κB signaling-mediated inflammatory responses in human monocytes. Cells. 2021;10:2549.
Guerrero-Hue M, García-Caballero C, Palomino-Antolín A, Rubio-Navarro A, Vázquez-Carballo C, Herencia C, Martín-Sanchez D, Farré-Alins V, Egea J, Cannata P, Praga M, Ortiz A, Egido J, Sanz AB, Moreno JA. Curcumin reduces renal damage associated with rhabdomyolysis by decreasing ferroptosis-mediated cell death. FASEB J. 2019;33:8961–75.
Schroeder A, Turjeman K, Schroeder JE, Leibergall M, Barenholz Y. Using liposomes to target infection and inflammation induced by foreign body injuries or medical implants. Expert Opin Drug Deliv. 2010;7:1175–89.
Chen C, Han X, Dong P, Li Z, Yanagita T, Xue C, Zhang T, Wang Y. Sea cucumber saponin liposomes ameliorate obesity-induced inflammation and insulin resistance in high-fat-diet-fed mice. Food Funct. 2018;9:861–70.
Wang D, Yang F, Shang W, Zhao Z, Shen J, Cai H. Paeoniflorin-loaded pH-sensitive liposomes alleviate synovial inflammation by altering macrophage polarity via STAT signaling. Int Immunopharmacol. 2021;101: 108310.
Wang K, Jiang L, Zhong Y, Zhang Y, Yin Q, Li S, Zhang X, Han H, Yao K. Ferrostatin-1-loaded liposome for treatment of corneal alkali burn via targeting ferroptosis. Bioeng Transl Med. 2022;7: e10276.
Han F, Li S, Yang Y, Bai Z. Interleukin-6 promotes ferroptosis in bronchial epithelial cells by inducing reactive oxygen species-dependent lipid peroxidation and disrupting iron homeostasis. Bioengineered. 2021;12:5279–88.
Guo Z, Lin J, Sun K, Guo J, Yao X, Wang G, Hou L, Xu J, Guo J, Guo F. Deferoxamine alleviates osteoarthritis by inhibiting chondrocyte ferroptosis and activating the Nrf2 pathway. Front Pharmacol. 2022;13: 791376.
Morris G, Walker AJ, Berk M, Maes M, Puri BK. Cell death pathways: a novel therapeutic approach for neuroscientists. Mol Neurobiol. 2018;55:5767–86.
Hayden MS, Ghosh S. Regulation of NF-κB by TNF family cytokines. Semin Immunol. 2014;26:253–66.
Yu Y, Yan Y, Niu F, Wang Y, Chen X, Su G, Liu Y, Zhao X, Qian L, Liu P, Xiong Y. Ferroptosis: a cell death connecting oxidative stress, inflammation and cardiovascular diseases. Cell Death Discov. 2021;7:193.
Lee JY, Kim WK, Bae KH, Lee SC, Lee EW. Lipid metabolism and ferroptosis. Biology (Basel). 2021;10:184.
Lei P, Bai T, Sun Y. Mechanisms of ferroptosis and relations with regulated cell death: a review. Front Physiol. 2019;10:139.
Liu Y, Zhou L, Lv C, Liu L, Miao S, Xu Y, Li K, Zhao Y, Zhao J (2022) PGE(2) pathway mediates oxidative stress-induced ferroptosis in renal tubular epithelial cells. FEBS J
Yan N, Xu Z, Qu C, Zhang J. Dimethyl fumarate improves cognitive deficits in chronic cerebral hypoperfusion rats by alleviating inflammation, oxidative stress, and ferroptosis via NRF2/ARE/ NF-κB signal pathway. Int Immunopharmacol. 2021;98: 107844.
Jin L, Yu B, Armando I, Han F. Mitochondrial DNA-mediated inflammation in acute kidney injury and chronic kidney disease. Oxid Med Cell Longev. 2021;2021:9985603.
Chen Y, Jin S, Teng X, Hu Z, Zhang Z, Qiu X, Tian D, Wu Y. Hydrogen sulfide attenuates LPS-induced acute kidney injury by inhibiting inflammation and oxidative stress. Oxid Med Cell Longev. 2018;2018:6717212.
Xia W, Li Y, Wu M, Jin Q, Wang Q, Li S, Huang S, Zhang A, Zhang Y, Jia Z. Gasdermin E deficiency attenuates acute kidney injury by inhibiting pyroptosis and inflammation. Cell Death Dis. 2021;12:139.
Yang Q, Zang HM, Xing T, Zhang SF, Li C, Zhang Y, Dong YH, Hu XW, Yu JT, Wen JG, Jin J, Li J, Zhao R, Ma TT, Meng XM. Gypenoside XLIX protects against acute kidney injury by suppressing IGFBP7/IGF1R-mediated programmed cell death and inflammation. Phytomedicine. 2021;85: 153541.
Deng F, Sharma I, Dai Y, Yang M, Kanwar YS. Myo-inositol oxygenase expression profile modulates pathogenic ferroptosis in the renal proximal tubule. J Clin Investig. 2019;129:5033–49.
Linkermann A, Skouta R, Himmerkus N, Mulay SR, Dewitz C, De Zen F, Prokai A, Zuchtriegel G, Krombach F, Welz PS, Weinlich R, Vanden Berghe T, Vandenabeele P, Pasparakis M, Bleich M, Weinberg JM, Reichel CA, Bräsen JH, Kunzendorf U, Anders HJ, Stockwell BR, Green DR, Krautwald S. Synchronized renal tubular cell death involves ferroptosis. Proc Natl Acad Sci U S A. 2014;111:16836–41.
Zhang J, Bi J, Ren Y, Du Z, Li T, Wang T, Zhang L, Wang M, Wei S, Lv Y, Wu R. Involvement of GPX4 in irisin’s protection against ischemia reperfusion-induced acute kidney injury. J Cell Physiol. 2021;236:931–45.
Wang Y, Zhang M, Bi R, Su Y, Quan F, Lin Y, Yue C, Cui X, Zhao Q, Liu S, Yang Y, Zhang D, Cao Q, Gao X. ACSL4 deficiency confers protection against ferroptosis-mediated acute kidney injury. Redox Biol. 2022;51: 102262.
Wang Y, Chen D, Xie H, Jia M, Sun X, Peng F, Guo F, Tang D. AUF1 protects against ferroptosis to alleviate sepsis-induced acute lung injury by regulating NRF2 and ATF3. Cell Mol Life Sci. 2022;79:228.
Li J, Lu K, Sun F, Tan S, Zhang X, Sheng W, Hao W, Liu M, Lv W, Han W. Panaxydol attenuates ferroptosis against LPS-induced acute lung injury in mice by Keap1-Nrf2/HO-1 pathway. J Transl Med. 2021;19:96.
Luo L, Huang F, Zhong S, Ding R, Su J, Li X. Astaxanthin attenuates ferroptosis via Keap1-Nrf2/HO-1 signaling pathways in LPS-induced acute lung injury. Life Sci. 2022;311: 121091.
Zhongyin Z, Wei W, Juan X, Guohua F. Isoliquiritin apioside relieves intestinal ischemia/reperfusion-induced acute lung injury by blocking Hif-1α-mediated ferroptosis. Int Immunopharmacol. 2022;108: 108852.
Zhang H, Liu J, Zhou Y, Qu M, Wang Y, Guo K, Shen R, Sun Z, Cata JP, Yang S, Chen W, Miao C. Neutrophil extracellular traps mediate m(6)A modification and regulates sepsis-associated acute lung injury by activating ferroptosis in alveolar epithelial cells. Int J Biol Sci. 2022;18:3337–57.
Huang F, Zhang S, Li X, Huang Y, He S, Luo L. STAT3-mediated ferroptosis is involved in ulcerative colitis. Free Radic Biol Med. 2022;188:375–85.
Xu M, Tao J, Yang Y, Tan S, Liu H, Jiang J, Zheng F, Wu B. Ferroptosis involves in intestinal epithelial cell death in ulcerative colitis. Cell Death Dis. 2020;11:86.
Tang B, Zhu J, Fang S, Wang Y, Vinothkumar R, Li M, Weng Q, Zheng L, Yang Y, Qiu R, Xu M, Zhao Z, Ji J. Pharmacological inhibition of MELK restricts ferroptosis and the inflammatory response in colitis and colitis-propelled carcinogenesis. Free Radic Biol Med. 2021;172:312–29.
Reichert CO, de Freitas FA, Sampaio-Silva J, Rokita-Rosa L, Barros PL, Levy D, Bydlowski SP. Ferroptosis mechanisms involved in neurodegenerative diseases. Int J Mol Sci. 2020;21:8765.
Mahoney-Sanchez L, Bouchaoui H, Boussaad I, Jonneaux A, Timmerman K, Berdeaux O, Ayton S, Krüger R, Duce JA, Devos D, Devedjian JC. Alpha synuclein determines ferroptosis sensitivity in dopaminergic neurons via modulation of ether-phospholipid membrane composition. Cell Rep. 2022;40: 111231.
Bao WD, Pang P, Zhou XT, Hu F, Xiong W, Chen K, Wang J, Wang F, Xie D, Hu YZ, Han ZT, Zhang HH, Wang WX, Nelson PT, Chen JG, Lu Y, Man HY, Liu D, Zhu LQ. Loss of ferroportin induces memory impairment by promoting ferroptosis in Alzheimer’s disease. Cell Death Differ. 2021;28:1548–62.
Bulluck H, Rosmini S, Abdel-Gadir A, White SK, Bhuva AN, Treibel TA, Fontana M, Ramlall M, Hamarneh A, Sirker A, Herrey AS, Manisty C, Yellon DM, Kellman P, Moon JC, Hausenloy DJ. Residual myocardial iron following intramyocardial hemorrhage during the convalescent phase of reperfused ST-segment-elevation myocardial infarction and adverse left ventricular remodeling. Circ Cardiovasc Imaging. 2016;9: e004940.
Miyamoto HD, Ikeda M, Ide T, Tadokoro T, Furusawa S, Abe K, Ishimaru K, Enzan N, Sada M, Yamamoto T, Matsushima S, Koumura T, Yamada KI, Imai H, Tsutsui H. Iron overload via heme degradation in the endoplasmic reticulum triggers ferroptosis in myocardial ischemia-reperfusion injury. JACC Basic Transl Sci. 2022;7:800–19.
Fang X, Wang H, Han D, Xie E, Yang X, Wei J, Gu S, Gao F, Zhu N, Yin X, Cheng Q, Zhang P, Dai W, Chen J, Yang F, Yang HT, Linkermann A, Gu W, Min J, Wang F. Ferroptosis as a target for protection against cardiomyopathy. Proc Natl Acad Sci U S A. 2019;116:2672–80.
Wang N, Ma H, Li J, Meng C, Zou J, Wang H, Liu K, Liu M, Xiao X, Zhang H, Wang K. HSF1 functions as a key defender against palmitic acid-induced ferroptosis in cardiomyocytes. J Mol Cell Cardiol. 2021;150:65–76.
Hwang JW, Park JH, Park BW, Kim H, Kim JJ, Sim WS, Mishchenko NP, Fedoreyev SA, Vasileva EA, Ban K, Park HJ, Baek SH. Histochrome attenuates myocardial ischemia-reperfusion injury by inhibiting ferroptosis-induced cardiomyocyte death. Antioxidants (Basel). 2021;10:1624.
Wang Y, Quan F, Cao Q, Lin Y, Yue C, Bi R, Cui X, Yang H, Yang Y, Birnbaumer L, Li X, Gao X. Quercetin alleviates acute kidney injury by inhibiting ferroptosis. J Adv Res. 2021;28:231–43.
Hu Z, Zhang H, Yi B, Yang S, Liu J, Hu J, Wang J, Cao K, Zhang W. VDR activation attenuate cisplatin induced AKI by inhibiting ferroptosis. Cell Death Dis. 2020;11:73.
Jiang GP, Liao YJ, Huang LL, Zeng XJ, Liao XH. Effects and molecular mechanism of pachymic acid on ferroptosis in renal ischemia reperfusion injury. Mol Med Rep. 2021;23:11.
Zhao Z, Wu J, Xu H, Zhou C, Han B, Zhu H, Hu Z, Ma Z, Ming Z, Yao Y, Zeng R, Xu G. XJB-5-131 inhibited ferroptosis in tubular epithelial cells after ischemia-reperfusion injury. Cell Death Dis. 2020;11:629.
Qiongyue Z, Xin Y, Meng P, Sulin M, Yanlin W, Xinyi L, Xuemin S. Post-treatment with irisin attenuates acute kidney injury in sepsis mice through anti-ferroptosis via the SIRT1/Nrf2 pathway. Front Pharmacol. 2022;13: 857067.
Adedoyin O, Boddu R, Traylor A, Lever JM, Bolisetty S, George JF, Agarwal A. Heme oxygenase-1 mitigates ferroptosis in renal proximal tubule cells. Am J Physiol Renal Physiol. 2018;314:F702-f714.
Lu Q, Wang M, Gui Y, Hou Q, Gu M, Liang Y, Xiao B, Zhao AZ, Dai C. Rheb1 protects against cisplatin-induced tubular cell death and acute kidney injury via maintaining mitochondrial homeostasis. Cell Death Dis. 2020;11:364.
Xiao J, Yang Q, Zhang Y, Xu H, Ye Y, Li L, Yang Y, Jin S. Maresin conjugates in tissue regeneration-1 suppresses ferroptosis in septic acute kidney injury. Cell Biosci. 2021;11:221.
Tao WH, Shan XS, Zhang JX, Liu HY, Wang BY, Wei X, Zhang M, Peng K, Ding J, Xu SX, Li LG, Hu JK, Meng XW, Ji FH. Dexmedetomidine attenuates ferroptosis-mediated renal ischemia/reperfusion injury and inflammation by inhibiting ACSL4 via α2-AR. Front Pharmacol. 2022;13: 782466.
Li X, Zou Y, Fu YY, Xing J, Wang KY, Wan PZ, Zhai XY. A-lipoic acid alleviates folic acid-induced renal damage through inhibition of ferroptosis. Front Physiol. 2021;12: 680544.
Zhou L, Yu P, Wang TT, Du YW, Chen Y, Li Z, He ML, Feng L, Li HR, Han X, Ma H, Liu HB. Polydatin attenuates cisplatin-induced acute kidney injury by inhibiting ferroptosis. Oxid Med Cell Longev. 2022;2022:9947191.
Yang J, Sun X, Huang N, Li P, He J, Jiang L, Zhang X, Han S, Xin H. Entacapone alleviates acute kidney injury by inhibiting ferroptosis. FASEB J. 2022;36: e22399.
Kim DH, Choi HI, Park JS, Kim CS, Bae EH, Ma SK, Kim SW. Farnesoid X receptor protects against cisplatin-induced acute kidney injury by regulating the transcription of ferroptosis-related genes. Redox Biol. 2022;54: 102382.
Sun Z, Wu J, Bi Q, Wang W. Exosomal lncRNA TUG1 derived from human urine-derived stem cells attenuates renal ischemia/reperfusion injury by interacting with SRSF1 to regulate ASCL4-mediated ferroptosis. Stem Cell Res Ther. 2022;13:297.
Li Y, Cao Y, Xiao J, Shang J, Tan Q, Ping F, Huang W, Wu F, Zhang H, Zhang X. Inhibitor of apoptosis-stimulating protein of p53 inhibits ferroptosis and alleviates intestinal ischemia/reperfusion-induced acute lung injury. Cell Death Differ. 2020;27:2635–50.
Dong H, Xia Y, Jin S, Xue C, Wang Y, Hu R, Jiang H. Nrf2 attenuates ferroptosis-mediated IIR-ALI by modulating TERT and SLC7A11. Cell Death Dis. 2021;12:1027.
Dong H, Qiang Z, Chai D, Peng J, Xia Y, Hu R, Jiang H. Nrf2 inhibits ferroptosis and protects against acute lung injury due to intestinal ischemia reperfusion via regulating SLC7A11 and HO-1. Aging (Albany NY). 2020;12:12943–59.
Qiang Z, Dong H, Xia Y, Chai D, Hu R, Jiang H. Nrf2 and STAT3 alleviates ferroptosis-mediated IIR-ALI by regulating SLC7A11. Oxid Med Cell Longev. 2020;2020:5146982.
Yang Y, Ma Y, Li Q, Ling Y, Zhou Y, Chu K, Xue L, Tao S. STAT6 inhibits ferroptosis and alleviates acute lung injury via regulating P53/SLC7A11 pathway. Cell Death Dis. 2022;13:530.
He R, Liu B, Xiong R, Geng B, Meng H, Lin W, Hao B, Zhang L, Wang W, Jiang W, Li N, Geng Q. Itaconate inhibits ferroptosis of macrophage via Nrf2 pathways against sepsis-induced acute lung injury. Cell Death Discov. 2022;8:43.
Liu X, Wang L, Xing Q, Li K, Si J, Ma X, Mao L. Sevoflurane inhibits ferroptosis: a new mechanism to explain its protective role against lipopolysaccharide-induced acute lung injury. Life Sci. 2021;275: 119391.
Li J, Deng SH, Li J, Li L, Zhang F, Zou Y, Wu DM, Xu Y. Obacunone alleviates ferroptosis during lipopolysaccharide-induced acute lung injury by upregulating Nrf2-dependent antioxidant responses. Cell Mol Biol Lett. 2022;27:29.
Luo M, Wu L, Zhang K, Wang H, Zhang T, Gutierrez L, O’Connell D, Zhang P, Li Y, Gao T, Ren W, Yang Y. miR-137 regulates ferroptosis by targeting glutamine transporter SLC1A5 in melanoma. Cell Death Differ. 2018;25:1457–72.
Wang S, Liu W, Wang J, Bai X. Curculigoside inhibits ferroptosis in ulcerative colitis through the induction of GPX4. Life Sci. 2020;259: 118356.
Chen Y, Wang J, Li J, Zhu J, Wang R, Xi Q, Wu H, Shi T, Chen W. Astragalus polysaccharide prevents ferroptosis in a murine model of experimental colitis and human Caco-2 cells via inhibiting NRF2/HO-1 pathway. Eur J Pharmacol. 2021;911: 174518.
Dong S, Lu Y, Peng G, Li J, Li W, Li M, Wang H, Liu L, Zhao Q. Furin inhibits epithelial cell injury and alleviates experimental colitis by activating the Nrf2-Gpx4 signaling pathway. Dig Liver Dis. 2021;53:1276–85.
Tian Y, Lu J, Hao X, Li H, Zhang G, Liu X, Li X, Zhao C, Kuang W, Chen D, Zhu M. FTH1 inhibits ferroptosis through ferritinophagy in the 6-OHDA model of Parkinson’s disease. Neurotherapeutics. 2020;17:1796–812.
Van Do B, Gouel F, Jonneaux A, Timmerman K, Gelé P, Pétrault M, Bastide M, Laloux C, Moreau C, Bordet R, Devos D, Devedjian JC. Ferroptosis, a newly characterized form of cell death in Parkinson’s disease that is regulated by PKC. Neurobiol Dis. 2016;94:169–78.
Shi L, Huang C, Luo Q, Xia Y, Liu W, Zeng W, Cheng A, Shi R, Zhengli C. Clioquinol improves motor and non-motor deficits in MPTP-induced monkey model of Parkinson’s disease through AKT/mTOR pathway. Aging (Albany NY). 2020;12:9515–33.
Bai L, Yan F, Deng R, Gu R, Zhang X, Bai J. Thioredoxin-1 rescues MPP(+)/MPTP-induced ferroptosis by increasing glutathione peroxidase 4. Mol Neurobiol. 2021;58:3187–97.
Hu CB, Jiang H, Yang Y, Wang GH, Ji QH, Jia ZZ, Shen LH, Luo QQ. DL-3-n-butylphthalide alleviates motor disturbance by suppressing ferroptosis in a rat model of Parkinson’s disease. Neural Regen Res. 2023;18:194–9.
Southon A, Szostak K, Acevedo KM, Dent KA, Volitakis I, Belaidi AA, Barnham KJ, Crouch PJ, Ayton S, Donnelly PS, Bush AI. Cu(II) (atsm) inhibits ferroptosis: Implications for treatment of neurodegenerative disease. Br J Pharmacol. 2020;177:656–67.
Sun Y, He L, Wang W, Xie Z, Zhang X, Wang P, Wang L, Yan C, Liu Z, Zhao J, Cui Z, Wang Y, Tang L, Zhang Z. Activation of Atg7-dependent autophagy by a novel inhibitor of the Keap1-Nrf2 protein-protein interaction from Penthorum chinense Pursh. attenuates 6-hydroxydopamine-induced ferroptosis in zebrafish and dopaminergic neurons. Food Funct. 2022;13:7885–900.
Chen R, Kang R, Tang D. The mechanism of HMGB1 secretion and release. Exp Mol Med. 2022;54:91–102.
Chen X, Wei W, Li Y, Huang J, Ci X. Hesperetin relieves cisplatin-induced acute kidney injury by mitigating oxidative stress, inflammation and apoptosis. Chem Biol Interact. 2019;308:269–78.
Acknowledgements
We thank the Public Service Platform of South China Sea for R&D Marine Biomedicine Resources for support.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82174157); The Science and technology program of Guangdong Province (2019B090905011).
Author information
Authors and Affiliations
Contributions
LXL and SSH conceived and designed the review. LYD, NQG and LXL wrote the manuscript; WT helped with the illustration; LXL, SSH and WZZ reviewed the paper and provided comments. All authors contributed to this article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deng, L., He, S., Guo, N. et al. Molecular mechanisms of ferroptosis and relevance to inflammation. Inflamm. Res. 72, 281–299 (2023). https://doi.org/10.1007/s00011-022-01672-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-022-01672-1