Abstract
Accumulating evidence suggests that fatty acids (FAs) play an essential role in regulating skeletal muscle mass and function throughout life. This systematic review and meta-analysis aimed to examine the relationship between dietary or circulatory levels of monounsaturated FAs (MUFAs) and sarcopenia in observational studies. A comprehensive literature search was performed in three databases (PubMed, Scopus, and Web of Science) from inception until August 2022. Of 414 records, a total of 12 observational studies were identified for this review. Ten studies were meta-analysed, comprising a total of 3704 participants. The results revealed that MUFA intake is inversely associated with sarcopenia (standardized mean difference = − 0.28, 95% CI − 0.46 to − 0.11; p < 0.01). Despite the limited number of studies, our results suggest that lower MUFA intake is associated with a higher risk of sarcopenia. However, the available evidence is still insufficient and further investigations are needed to demonstrate this relationship.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcopenia is a progressive skeletal muscle disorder characterized by an accelerated decrease in muscle mass, muscle strength, and physical function [1, 2]. The prevalence of sarcopenia ranges from 10 to 27% in people over 60 years of age [3]. Elderly people suffering from sarcopenia are at high risk of adverse outcomes such as falls, fractures, poor quality of life, physical disability, hospitalization, and mortality [4, 5]. Since the aging population is increasing globally, sarcopenia has become a major public health issue [3]. In the past decade, sarcopenia has become the focus of intense investigations to better understand its pathophysiology and to identify effective preventive and treatment strategies [6, 7].
Besides insufficient protein intake and physical inactivity, accumulating evidence suggests that oxidative stress and inflammation are the main contributors to the complex etiology of sarcopenia [8, 9]. During aging, excessive production of reactive oxygen species (ROS), which controls the redox signal pathway, results in oxidative damage and mitochondrial dysfunction, impaired protein homeostasis, and eventually skeletal muscle dysfunction [10,11,12]. Age-related impairments in mitochondrial function may also increase oxidative stress and enhance the loss of proteostasis [9]. In addition, chronic low-grade inflammation during aging affects the metabolism of skeletal muscle cells through interactions among various cytokines [13]. Furthermore, inflammation causes oxidative stress and anabolic resistance, leading to the loss of muscle mass, strength, and function [13].
Although the association between diet and sarcopenia is still under investigation, a growing body of evidence suggests that nutrition has an important role in both the prevention and treatment of sarcopenia, in particular, a dietary pattern that ensure an adequate protein intake [14]. In addition, higher intakes of antioxidant nutrients play an important role in the regulation of muscle mass and function throughout life [15]. Indeed, current observational and clinical data show that increasing fruit and vegetable consumption could be effective tools to prevent or treat sarcopenia, especially by enhancing muscle strength and function [16]. Monounsaturated fatty acids (MUFA) have recently attracted considerable attention because of their role in health and disease prevention. MUFA are dietary nutrients most commonly found in olive oil, nuts, seeds, and some animal-based foods [17]. The most common MUFA in the diet is oleic acid (C18:1n-9, OL), which is also the highest MUFA provided in the diet (around 90% of all MUFA), followed by palmitoleic acid (16:1n-7, PLA) and vaccenic acid (18:1n-7) [17]. Detailed studies have shown that olive oil, the main source of MUFA, may attenuate oxidative stress, the main mechanism of sarcopenia pathogenesis [18,19,20]. Additionally, the Mediterranean diet, which is particularly rich in MUFA, reduces inflammation related to aging [21, 22].
Previous observational studies have evaluated the effects of MUFA on muscle parameters and sarcopenia, however, inconclusive results are reported. Therefore, the purpose of this systematic review and meta-analysis was to evaluate the association between dietary intake of MUFA and sarcopenia. In addition, we investigated whether this association is influenced by population characteristics, methods for MUFA assessment, and the diagnostic criteria of sarcopenia.
Materials and methods
This systematic review and meta-analysis were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [23].
Eligibility criteria
Studies were eligible for this systematic review if they met the following criteria: (1) observational studies (cohort, case–control, cross-sectional) that evaluated the association between dietary or circulatory MUFA levels with sarcopenia, determined as confirmed/severe sarcopenia, probable sarcopenia, sarcopenic index, or sarcopenia risk score; (2) included adult people (aged 18 years and more); and (3) studies published in English. On the contrary, the exclusion criteria included: (1) randomized controlled trials; and (2) studies with secondary data (conference abstracts, meta-analyses, reviews, letters, and case reports). The PICOS criteria (i.e., participants, interventions, comparisons, outcomes, and study design) used to define the research question are shown in Table 1.
Search strategy
A systematic search was performed using three databases: PubMed, Scopus, and Web of Science. The following keywords and Boolean operators were used for the literature search: ("monounsaturated fatty acid" OR "monounsaturated fat" OR "MUFA" OR "palmitoleic acid" OR "oleic acid") AND ("sarcopenia" OR "sarcopenic" OR "muscular atrophy" OR "muscle strength" OR "muscle mass" OR "muscle fatigue" OR "physical performance"). At the same time, similar queries were respectively used for controlled vocabulary search: “monounsaturated fatty acids” [Mesh] AND “sarcopenia” [Mesh], INDEX TERMS “monounsaturated fatty acids” AND “sarcopenia”. The search was conducted from inception to August 2022. The search queries used to search in PubMed, Scopus, and Web of Science databases are presented in Table S1.
Study selection and data extraction
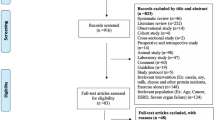
After removing duplicate records with the reference management software EndNote X9 (Clarivate Analytics, Philadelphia, PA, USA), titles and abstracts of retrieved articles were screened for eligibility by two researchers (SA and SD). If an abstract did not provide enough information for evaluation, the full text was retrieved. Disagreements were resolved by a third reviewer (GC). Articles that met the eligibility criteria were selected for inclusion in the final review (Fig. 1). A data extraction table for the included studies was then developed. The following information was extracted: the first author (along with the year of publication and country of the study), study design, participant characteristics (sample size, age, gender), exposure assessment, outcome measure and sarcopenia definition, and the main findings.
Quality assessment
Methodological quality assessments of the included studies were performed using the Newcastle–Ottawa Scale (NOS) for observational studies [24]. The NOS assesses three quality domains (selection, comparability, and outcome) divided into eight specific items. The NOS gives a maximum score of 9 points. Studies with NOS scores of 0–3, 4–6, and 7–9 were considered low, moderate and high quality, respectively [25].
Statistical analysis
The meta-analysis was conducted using the R Software, version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria) and the interface RStudio version 1.4.1717 (R studio, PBC, Boston, MA, USA). Mean values and standard deviations (SD) of MUFA levels were extracted for the meta-analysis. The standardized mean difference (SMD) was used as a summary statistic because the studies assessed the outcome using different techniques and tools. A p-value of less than 0.05 was considered to be statistically significant. Heterogeneity among studies was examined with I2 statistics [26]. Random-effects models were used for the analyses and the possibility of small study effects was assessed qualitatively by a visual estimate of the funnel plot and quantitatively by calculation of the Egger and Begg’s tests [27]. In addition, subgroup analyses were performed that included consideration of sarcopenic obesity, participants' age (< 65 and ≥ 65 years to evaluate the aging effect), gender (men, women, and both), sarcopenia classification (confirmed/severe sarcopenia and probable sarcopenia), sarcopenia diagnostic criteria (the European Working Group on Sarcopenia (EWGSOP) [6], EWGSOP2 [7], the Asian Working Group for Sarcopenia (AWGS) [28], and the other diagnostic criteria), MUFA exposure assessment (dietary and circulatory), and MUFA intake unit (percent of total energy, percent of total FA, grams/day, MUFA/saturated FA (SFA) ratio).
Results
Study identification and selection
The PRISMA flow diagram of this systematic review and meta-analysis is presented in Fig. 1. A total of 414 potentially relevant articles (PubMed: 60, Scopus: 300, and Web of Science: 54) were yielded during initial literature searches. After eliminating 112 duplicated articles, 302 articles were screened by titles and abstracts. Eventually, a total of 12 articles were identified to be included in our study [29,30,31,32,33,34,35,36,37,38,39,40].
Study characteristics
The main characteristics of the included studies are presented in Table 2. The studies were published between 2006 and 2021. The countries in which the studies were conducted were Spain [29, 31], Brazil [32, 33], Japan [36, 38], Canada [30], Iran [34], Finland [35], the Netherlands [39], and UK [40], and one study was conducted in multiple European countries [37]. All studies included both men and women, except for one study that included only men [35] and one that included only women [30]. The sample size ranged from 22 to 1535 subjects. The diagnostic criteria for sarcopenia were the EWGSOP [31], the EWGSOP2 [33,34,35, 37, 39], the AWGS [36, 38], and other diagnostic criteria [29, 30, 32, 40]. Seven of the included studies diagnosed confirmed/severe sarcopenia [31, 33, 35, 36, 38,39,40], and two studies determined probable sarcopenia among the participants [34, 35]. Additionally, Abete 2019 calculated sarcopenic index [29]. The sarcopenic index in this study was estimated by dividing the amount of appendicular skeletal muscle mass (kg) by body weight (kg) × 100. The authors then categorized the participants according to sex-specific sarcopenic index tertiles, providing an estimate of the amount of skeletal muscle mass relative to body size, where a higher index implied better health. Furthermore, Montiel-Rojas 2020 determined a continuous clustered sarcopenia risk score, which was estimated based on skeletal muscle mass index (SMI) and handgrip strength [37]. The authors first calculated sex-specific standardized values of SMI and handgrip strength and averaged them into composite z-scores, where higher scores implied a higher sarcopenia risk.
Two studies measured circulatory MUFA levels [36, 39], whereas the remaining ten studies estimated dietary intake of MUFA. The dietary MUFA were determined by food-frequency questionnaire (FFQ) [29, 34], 24-h dietary recall [31, 33], 3-day food diary [35, 40], 7-day food diary [37], dietary recall questionnaires [32], and brief-type self-administered diet history questionnaire (BDHQ) [38].
Quality of the included studies
The quality of the included studies, based on NOS quality assessment, is shown in Table S2. One study achieved NOS scores of 6 (moderate quality) [30], and 11 studies was rated as “high” quality (7–9 points) [29, 31,32,33,34,35,36,37,38, 40].
Meta-analysis of the effects of MUFA on sarcopenia
Ten of the 12 studies were included in the meta-analysis as the required pooling data were available [29,30,31,32,33,34,35,36, 38, 40]. These studies involved a total of 3704 participants. The overall combined SMD showed that the dietary or circulatory MUFA level is inversely associated with the risk of sarcopenia (SMD = − 0.28, 95% CI − 0.46 to − 0.11; p < 0.01) (Fig. 2). A high level of heterogeneity was found among the studies (I2 = 79%, p < 0.01). The funnel plots showed no evidence of publication bias in the included studies (Fig. 3). Likewise, Egger’s and Begg’s rank tests detected no evidence of publication bias (p = 0.09 and p = 0.7, respectively).
The results of the subgroup analyses are shown in Table 3. The pooled analysis of three studies that involved 1087 subjects with sarcopenic obesity did not show a significant association between MUFA intake and sarcopenic obesity (SMD = 0.11, 95% CI − 0.01 to 0.22, p = 0.08). Eight studies on 3532 people over 65 years of age confirmed a significant effect of MUFA on sarcopenia (SMD = − 0.26, 95% CI − 0.45 to − 0.07, p < 0.01). The remaining two studies involved 172 subjects with an overall mean age less than 65 years, and the pooled analysis showed a negative, although not significant, association between MUFA levels and sarcopenia (SMD = – 0.45, 95% CI − 0.92 to 0.02, p = 0.06). Likewise, eight studies included both men and women and showed a negative association (SMD = – 0.26, 95% CI − 0.45 to − 0.07, p < 0.01). Regarding the diagnostic criteria of sarcopenia, the significant result existed in EWGSOP2 (SMD = – 0.46, 95% CI − 0.71 to − 0.21; p < 0.01) and AWGS (SMD = – 0.33, 95% CI − 0.50 to − 0.15; p < 0.01), but lost in others (SMD = – 0.09, 95% CI − 0.02 to 0.20; p = 0.12). The above findings were also confirmed in dietary MUFA levels (SMD = – 0.27, 95% CI − 0.47 to − 0.07, p < 0.01), considering dietary recall tools (SMD = – 0.37, 95% CI − 0.55 to − 0.19, p < 0.01). Additionally, MUFA levels expressed as a percent of total energy (SMD = – 0.29, 95% CI − 0.57 to − 0.01, p = 0.04), grams/day (SMD = – 0.28, 95% CI − 0.48 to − 0.08, p < 0.01), and MUFA/SFA ratio (SMD = – 0.34, 95% CI − 0.57 to − 0.12, p < 0.01) showed significant negative associations between MUFA and sarcopenia.
Discussion
Despite the limited number of observational studies included in our systematic review and meta-analysis, the results suggest that MUFA intake is inversely associated with the risk of sarcopenia. In addition, the corresponding result subsisted in several subgroup analyses that were performed based on population characteristics, MUFA assessment tools, and sarcopenia diagnosis. Among the 10 studies that were meta-analysed, six studies reported a significantly lower MUFA intake in sarcopenic subjects compared to non-sarcopenic ones [31, 33,34,35,36, 38]. On the other hand, the remaining four studies did not report any significant difference in MUFA intake between sarcopenic and control participants [29, 30, 32, 40]. Furthermore, two more studies that were included in the review but not in the meta-analysis did not find a significant association between MUFA intake and the risk of sarcopenia [37, 39]. Montiel-rojas 2020 reported that substituting SFAs by MUFAs does not affect sex-specific sarcopenia risk score in 986 older European adults [37]. Similarly, ter Borg 2018 found no significant associations between blood MUFA status and sarcopenia in 227 community-dwelling older adults [39]. Therefore, although MUFA intake showed a negative association with sarcopenia in our meta-analysis, the available data are still insufficient to confirm this association, and further investigations are required.
Our finding that a higher intake of MUFA may have positive effects on sarcopenia is consistent with previous reports indicating that MUFA may inhibit muscle atrophy by enhancing mitochondrial oxidative ability, protein synthesis, insulin sensitivity, and reducing inflammation [41]. For example, MUFA have been reported to prevent SFA-induced insulin resistance and exert anti-inflammatory effects in skeletal muscle cells [42,43,44]. MUFA protects against SFA-induced inflammation and insulin resistance by promoting triglyceride accumulation and mitochondrial beta-oxidation through peroxisome proliferator-activated receptor-alpha (PPAR-α) and protein kinase A-dependent mechanisms [43]. Likewise, OL inhibits SFA-mediated activation of the mammalian target of rapamycin complex 1 (mTORC1)/p70S6K, leading to a reduction in intracellular inflammatory signalling and cytotoxicity [45]. Additionally, in aging individuals, there is an elevation of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukin 6 (IL-6) and C-reactive protein (CRP), that contribute to low muscle mass and strength [46]. MUFA, such as OL is shown to reduce serum CRP and increase anti-inflammatory gene expression [47, 48]. These anti-inflammatory actions of MUFA in skeletal muscle cells may contribute to their ability to preserve muscle mass and function [41]. MUFA also prevents muscle atrophy and increase muscle differentiation by enhancing mitochondrial function and reducing mitochondrial ROS [49, 50]. It is demonstrated that an OL-enriched diet may increase muscle protein synthesis, associated with increased expression of genes implicated in stimulating mitochondrial β-oxidation including PPAR-α and PPAR-beta (PPAR-β), as well as carnitine palmitoyl transferase 1 beta (CPT-1β) [51, 52]. Therefore, MUFA intake, particularly OL, may have the potential as an effective nutrition-based preventive or therapeutic strategy against sarcopenia.
Of the 10 studies included in our meta-analysis, three studies involved subjects with sarcopenic obesity [29, 30, 32]. Sarcopenic obesity is defined as the presence of both obesity (high body fat percentage or fat mass index) and sarcopenia [53]. It is associated with an increased risk of cardiovascular disease and mortality in the aging population [54]. Sarcopenic obesity is proposed to be considered a distinctive clinical condition because its effect on health and clinical outcomes is different from those related to obesity or sarcopenia. Due to the negative interaction between fat mass accumulation and low muscle mass/function, sarcopenic obese subjects have a higher risk for metabolic disorders and functional declines compared to sarcopenic or obese individuals. The management of sarcopenic obesity is challenging and preventive/treatment strategies may not only be a combination of the methods used to manage obesity and sarcopenia. It is suggested that personalized multidisciplinary approaches with dietary, physical, psychological, and pharmacological mechanisms may be ideal to manage this condition [53]. Beside the effects of MUFAs on muscle health, previous studies indicate that MUFAs may accelerate overall lipid oxidation in peroxisome and mitochondria by stimulating peroxisomal and mitochondrial beta-oxidation [43, 55]. Long-chain MUFAs can also improve obesity-related metabolic dysfunction by upregulation of PPAR-gamma (PPAR-γ) and downregulation of inflammatory markers in the adipose tissue [56]. Indeed, the anti-inflammatory effect of MUFA-rich Mediterranean diet is described to decrease the risk of obesity-related metabolic syndrome [57]. Nevertheless, our analysis of three studies involving 1087 participants did not show a significant association between MUFA intake and sarcopenic obesity (Table 3).
Although the number of studies with sex descriptions is limited, some sex-related differences in experimental models are described to be associated with the effect of diet on sarcopenia [58]. The majority of the studies included in our review were designed for both men and women and sex-specific analyses were not performed. The pooled analysis of these studies showed that MUFA levels are significantly lower in sarcopenic subjects compared to the non-sarcopenic ones (Table 3). On the other hand, the study by Jyväkorpi et al. examined community-living oldest old men, and Aubertin-Leheudre et al. studied a group of sarcopenic and non-sarcopenic obese post-menopausal women [30, 35]. Jyväkorpi et al. reported that higher MUFA intake and MUFA/SFA ratio are both associated with lower sarcopenia risk [35]. In contrast, the results of the Aubertin-Leheudre et al. study did not show any significant difference in MUFA intake among the two groups [30]. In this study, however, the non-sarcopenic women had a greater body mass index (BMI), abdominal fat mass, and visceral fat mass than the sarcopenic women [30]. The BMI and body fat are reported to be associated with sarcopenia [59, 60]. In addition, Aubertin-Leheudre et al. included 22 women, suggesting that a large sample-sized study may be more reliable to address the correlation [30].
The articles included in our study were published between 2006 and 2021, involving a period with considerable changes in the diagnostic criteria of sarcopenia. Sarcopenia was first described in 1989 as an age-related reduction in muscle mass [1, 2]. In 2000, sarcopenia was defined as two SD below the mean value of appendicular skeletal muscle mass divided by height squared of sex-specific young adult reference value [61]. Other definitions of sarcopenia later emerged that required measurement of a combination of three parameters, which are muscle mass, muscle strength, and physical performance. In 2010, the EWGSOP proposed an operational definition of sarcopenia that added muscle function to previous definitions based on low muscle mass [6]. According to the EWGSOP, the diagnosis of sarcopenia requires the detection of low muscle mass with low muscle function (muscle strength or physical performance). The EWGSOP was then updated in 2019 as EWGSOP2 [7]. The EWGSOP2 used poor muscle strength as the primary parameter of sarcopenia instead of low muscle mass. According to the EWGSOP2, sarcopenia is probable when low muscle strength is detected, sarcopenia diagnosis is confirmed when low muscle quantity and quality are identified, and sarcopenia is severe when low muscle strength, low muscle quantity/quality and poor physical performance are detected altogether. Although the EWGSOP did not advise specific cut-off points, the EWGSOP2 provided clear cut-off points of the parameters used for sarcopenia diagnosis [6, 7]. Furthermore, in 2014, the AWGS was proposed, which has a similar definition as the EWGSOP and was later revised in 2019 [28]. The AWGS established an EWGSOP-based consensus that denoted cut-off points for diagnostic variables of sarcopenia in Asian populations. When we performed a subgroup analysis by the diagnostic criteria of sarcopenia, the corresponding result existed in EWGSOP2 and AWGS but was lost in the other diagnostic criteria. In addition, we observed a significant decrease in heterogeneity in this subgroup analysis (Table 3).
This systematic review and meta-analysis have some limitations. First, there was a substantial level of heterogeneity in the meta-analysis, which could be due to the heterogeneity in the methods and diagnostic criteria used to define sarcopenia among the included articles. Second, previous evidence suggests that there is sex-specific differences in pathophysiological mechanisms and risk factors for sarcopenia [62, 63]. However, many of the included studies did not consider sex differences, and therefore, a subgroup analysis by sex could not be performed in these studies. Another limitation of our study is that due to scarcity of data, we were unable to perform a subgroup analysis based on co-diseases present in the population, which could certainly affect sarcopenia. Finally, there is a limitation of relevant literature, in which 12 studies were identified and only 10 of them could be meta-analysed. Our study also has several strengths. First, to our knowledge, this is the first meta-analysis of observational studies on the relationship between dietary or circulatory MUFA levels and sarcopenia based on a comprehensive literature search. In addition, almost all of the included studies were published in recent years, suggesting a potential novel topic in our systematic review and meta-analysis.
Overall, this systematic review and meta-analysis provide preliminary evidence that MUFA intake is different among people with sarcopenia compared to people without sarcopenia. However, current evidence is still insufficient to demonstrate the definite relationship between MUFA intake and sarcopenia. More well-designed prospective cohort studies along with clinical trials are still needed.
Availability of data and materials
From authors upon request.
References
Rosenberg IH (1989) Summary comments. Am J Clin Nutr 50:1231–1233. https://doi.org/10.1093/ajcn/50.5.1231
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127:990s-s991. https://doi.org/10.1093/jn/127.5.990S
Petermann-Rocha F, Balntzi V, Gray SR et al (2022) Global prevalence of sarcopenia and severe sarcopenia: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 13:86–99. https://doi.org/10.1002/jcsm.12783
Cruz-Jentoft AJ, Sayer AA (2019) Sarcopenia. Lancet 393:2636–2646. https://doi.org/10.1016/s0140-6736(19)31138-9
Bruyère O, Beaudart C, Locquet M et al (2016) Sarcopenia as a public health problem. Eur Geriatr Med 7:272–275. https://doi.org/10.1016/j.eurger.2015.12.002
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Chen M, Wang Y, Deng S et al (2022) Skeletal muscle oxidative stress and inflammation in aging: Focus on antioxidant and anti-inflammatory therapy. Front Cell Dev Biol. 10:964130. https://doi.org/10.3389/fcell.2022.964130
Coen PM, Musci RV, Hinkley JM et al (2018) Mitochondria as a target for mitigating sarcopenia. Front Physiol 9:1883. https://doi.org/10.3389/fphys.2018.01883
Lourenço Dos Santos S, Baraibar MA, Lundberg S et al (2015) Oxidative proteome alterations during skeletal muscle ageing. Redox Biol 5:267–74. https://doi.org/10.1016/j.redox.2015.05.006
Granic A, Sayer AA, Robinson SM (2019) Dietary patterns, skeletal muscle health, and sarcopenia in older adults. Nutrients. https://doi.org/10.3390/nu11040745
Bellanti F, Buglio AL, Vendemiale G (2020) Chapter 9 - oxidative stress and sarcopenia. In: Preedy VR, Patel VB (eds) Aging, 2nd edn. Academic Press, pp 95–103. https://doi.org/10.1016/B978-0-12-818698-5.00009-2
Dalle S, Rossmeislova L, Koppo K (2017) The role of inflammation in age-related sarcopenia. Front Physiol 8:1045. https://doi.org/10.3389/fphys.2017.01045
Beasley JM, Shikany JM, Thomson CA (2013) The role of dietary protein intake in the prevention of sarcopenia of aging. Nutr Clin Pract 28:684–690. https://doi.org/10.1177/0884533613507607
Ganapathy A, Nieves JW (2020) Nutrition and sarcopenia-what do we know? Nutrients. https://doi.org/10.3390/nu12061755
Besora-Moreno M, Llauradó E, Valls RM et al (2022) Antioxidant-rich foods, antioxidant supplements, and sarcopenia in old-young adults ≥55 years old: a systematic review and meta-analysis of observational studies and randomized controlled trials. Clin Nutr 41:2308–2324. https://doi.org/10.1016/j.clnu.2022.07.035
Schwingshackl L, Hoffmann G (2014) Monounsaturated fatty acids, olive oil and health status: a systematic review and meta-analysis of cohort studies. Lipids Health Dis 13:154. https://doi.org/10.1186/1476-511X-13-154
Quiles JL, Barja G, Battino M et al (2006) Role of olive oil and monounsaturated fatty acids in mitochondrial oxidative stress and aging. Nutr Rev 64:S31–S39. https://doi.org/10.1111/j.1753-4887.2006.tb00261.x
Yazihan N, Akdas S, Olgar Y et al (2020) Olive oil attenuates oxidative damage by improving mitochondrial functions in human keratinocytes. J Funct Foods 71:104008. https://doi.org/10.1016/j.jff.2020.104008
Musumeci G, Maria Trovato F, Imbesi R et al (2014) Effects of dietary extra-virgin olive oil on oxidative stress resulting from exhaustive exercise in rat skeletal muscle: a morphological study. Acta Histochem 116:61–69. https://doi.org/10.1016/j.acthis.2013.05.006
Tsigalou C, Konstantinidis T, Paraschaki A et al (2020) Mediterranean diet as a tool to combat inflammation and chronic diseases. An overview. Biomedicines 8:201. https://doi.org/10.3390/biomedicines8070201
Sureda A, Bibiloni MDM, Julibert A et al (2018) Adherence to the Mediterranean diet and inflammatory markers. Nutrients 10:62
Moher D, Shamseer L, Clarke M et al (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Cui C-J, Wang G-J, Yang S et al (2018) Tissue Factor-bearing MPs and the risk of venous thrombosis in cancer patients: a meta-analysis. Sci Rep 8:1675. https://doi.org/10.1038/s41598-018-19889-8
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Chen LK, Liu LK, Woo J et al (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101. https://doi.org/10.1016/j.jamda.2013.11.025
Abete I, Konieczna J, Zulet MA et al (2019) Association of lifestyle factors and inflammation with sarcopenic obesity: data from the PREDIMED-Plus trial. J Cachexia Sarcopenia Muscle 10:974–984. https://doi.org/10.1002/jcsm.12442
Aubertin-Leheudre M, Lord C, Goulet ÉDB et al (2006) Effect of sarcopenia on cardiovascular disease risk factors in obese postmenopausal women. Obesity 14:2277–2283. https://doi.org/10.1038/oby.2006.267
Bibiloni MM, Karam J, Bouzas C et al (2018) Association between physical condition and body composition, nutrient intake, sociodemographic characteristics, and lifestyle habits in older Spanish adults. Nutrients. https://doi.org/10.3390/nu10111608
de França NAG, Peters BSE, dos Santos EA et al (2020) Obesity associated with low lean mass and low bone density has higher impact on general health in middle-aged and older adults. J Obes. https://doi.org/10.1155/2020/8359616
Dos Reis AS, Limirio LS, Santos HO et al (2021) Intake of polyunsaturated fatty acids and ω-3 are protective factors for sarcopenia in kidney transplant patients. Nutrition 81:110929. https://doi.org/10.1016/j.nut.2020.110929
Esmaeily Z, Tajary Z, Daei S et al (2021) Association between Healthy Eating Index-2015 scores and probable sarcopenia in community-dwelling Iranian older adults: a cross-sectional study. J Nutr Sci 10:e20. https://doi.org/10.1017/jns.2021.12
Jyväkorpi SK, Urtamo A, Kivimäki M et al (2020) Macronutrient composition and sarcopenia in the oldest-old men: The Helsinki Businessmen Study (HBS). Clin Nutr 39:3839–3841. https://doi.org/10.1016/j.clnu.2020.04.024
Katoh A, Ikeda H, Matsushima Y et al (2020) Long-chain fatty acids in sarcopenia patients with cardiovascular diseases: importance of n-9 monounsaturated fatty acids. JCSM Clinical Reports 5:121–128. https://doi.org/10.1002/crt2.27
Montiel-Rojas D, Santoro A, Nilsson A et al (2020) Beneficial role of replacing dietary saturated fatty acids with polyunsaturated fatty acids in the prevention of sarcopenia: findings from the nu- age cohort. Nutrients 12:3079. https://doi.org/10.3390/nu12103079
Otsuka Y, Iidaka T, Horii C et al (2021) Dietary intake of vitamin E and fats associated with sarcopenia in community-dwelling older Japanese people: a cross-sectional study from the Fifth Survey of the ROAD Study. Nutrients. https://doi.org/10.3390/nu13051730
ter Borg S, Luiking YC, van Helvoort A et al (2019) Low levels of branched chain amino acids, eicosapentaenoic acid and micronutrients are associated with low muscle mass, strength and function in community-dwelling older adults. J Nutr Health Aging 23:27–34. https://doi.org/10.1007/s12603-018-1108-3
Verlaan S, Aspray TJ, Bauer JM et al (2017) Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case-control study. Clin Nutr 36:267–274. https://doi.org/10.1016/j.clnu.2015.11.013
Lipina C, Hundal HS (2017) Lipid modulation of skeletal muscle mass and function. J Cachexia Sarcopenia Muscle 8:190–201. https://doi.org/10.1002/jcsm.12144
Salvadó L, Coll T, Gómez-Foix AM et al (2013) Oleate prevents saturated-fatty-acid-induced ER stress, inflammation and insulin resistance in skeletal muscle cells through an AMPK-dependent mechanism. Diabetologia 56:1372–1382. https://doi.org/10.1007/s00125-013-2867-3
Coll T, Eyre E, Rodríguez-Calvo R et al (2008) Oleate reverses palmitate-induced insulin resistance and inflammation in skeletal muscle cells. J Biol Chem 283:11107–11116. https://doi.org/10.1074/jbc.M708700200
Macrae K, Stretton C, Lipina C et al (2013) Defining the role of DAG, mitochondrial function, and lipid deposition in palmitate-induced proinflammatory signaling and its counter-modulation by palmitoleate. J Lipid Res 54:2366–2378. https://doi.org/10.1194/jlr.M036996
Kwon B, Querfurth HW (2015) Palmitate activates mTOR/p70S6K through AMPK inhibition and hypophosphorylation of raptor in skeletal muscle cells: reversal by oleate is similar to metformin. Biochimie 118:141–150. https://doi.org/10.1016/j.biochi.2015.09.006
Taaffe DR, Harris TB, Ferrucci L et al (2000) Cross-sectional and prospective relationships of interleukin-6 and C-reactive protein with physical performance in elderly persons: MacArthur studies of successful aging. J Gerontol A Biol Sci Med Sci 55:M709–M715. https://doi.org/10.1093/gerona/55.12.m709
Yoneyama S, Miura K, Sasaki S et al (2007) Dietary intake of fatty acids and serum C-reactive protein in Japanese. J Epidemiol 17:86–92. https://doi.org/10.2188/jea.17.86
van Dijk SJ, Feskens EJ, Bos MB et al (2009) A saturated fatty acid-rich diet induces an obesity-linked proinflammatory gene expression profile in adipose tissue of subjects at risk of metabolic syndrome. Am J Clin Nutr 90:1656–1664. https://doi.org/10.3945/ajcn.2009.27792
Lee H, Lim JY, Choi SJ (2017) Oleate Prevents palmitate-induced atrophy via modulation of mitochondrial ROS production in skeletal myotubes. Oxid Med Cell Longev 2017:2739721. https://doi.org/10.1155/2017/2739721
Xue M, Zhang F, Ji X et al (2021) Oleate ameliorates palmitate-induced impairment of differentiative capacity in C2C12 myoblast cells. Stem Cells Dev 30:289–300. https://doi.org/10.1089/scd.2020.0168
Muoio DM, Way JM, Tanner CJ et al (2002) Peroxisome proliferator-activated receptor-alpha regulates fatty acid utilization in primary human skeletal muscle cells. Diabetes 51:901–909. https://doi.org/10.2337/diabetes.51.4.901
Tardif N, Salles J, Landrier JF et al (2011) Oleate-enriched diet improves insulin sensitivity and restores muscle protein synthesis in old rats. Clin Nutr 30:799–806. https://doi.org/10.1016/j.clnu.2011.05.009
Gortan Cappellari G, Guillet C, Poggiogalle E et al (2023) Sarcopenic obesity research perspectives outlined by the sarcopenic obesity global leadership initiative (SOGLI)—Proceedings from the SOGLI consortium meeting in Rome November 2022. Clin Nutr 42:687–699. https://doi.org/10.1016/j.clnu.2023.02.018
Atkins JL, Whincup PH, Morris RW (2014) Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc 62:253–260. https://doi.org/10.1111/jgs.12652
Halvorsen B, Rustan AC, Madsen L et al (2001) Effects of long-chain monounsaturated and n-3 fatty acids on fatty acid oxidation and lipid composition in rats. Ann Nutr Metab 45:30–37. https://doi.org/10.1159/000046703
Yang Z-H, Miyahara H, Iwasaki Y et al (2013) Dietary supplementation with long-chain monounsaturated fatty acids attenuates obesity-related metabolic dysfunction and increases expression of PPAR gamma in adipose tissue in type 2 diabetic KK-Ay mice. Nutr Metab 10:16. https://doi.org/10.1186/1743-7075-10-16
Ravaut G, Légiot A, Bergeron KF et al (2020) Monounsaturated fatty acids in obesity-related inflammation. Int J Mol Sci. https://doi.org/10.3390/ijms22010330
Kob R, Fellner C, Bertsch T et al (2015) Gender-specific differences in the development of sarcopenia in the rodent model of the ageing high-fat rat. J Cachexia Sarcopenia Muscle 6:181–191. https://doi.org/10.1002/jcsm.12019
Han P, Zhao J, Guo Q et al (2016) Incidence, risk factors, and the protective effect of high body mass index against sarcopenia in suburb-dwelling elderly Chinese populations. J Nutr Health Aging 20:1056–1060. https://doi.org/10.1007/s12603-016-0704-3
Cho YJ, Lim Y-H, Yun JM et al (2020) Sex- and age-specific effects of energy intake and physical activity on sarcopenia. Sci Rep 10:9822. https://doi.org/10.1038/s41598-020-66249-6
Baumgartner RN (2000) Body composition in healthy aging. Ann N Y Acad Sci 904:437–448. https://doi.org/10.1111/j.1749-6632.2000.tb06498.x
Tay L, Ding YY, Leung BP et al (2015) Sex-specific differences in risk factors for sarcopenia amongst community-dwelling older adults. Age (Dordr) 37:121. https://doi.org/10.1007/s11357-015-9860-3
Hwang J, Park S (2022) Sex differences of sarcopenia in an elderly Asian population: the prevalence and risk factors. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph191911980
Funding
Open access funding provided by Università degli Studi del Molise within the CRUI-CARE Agreement. This research did not receive any funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: SD, GS, and GC; literature search and data analysis: SA, GC, and SD; writing—original draft preparation: SA and AM; writing—review and editing: SD, GC, and MI.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to disclose.
Human and animal rights
This review does not contain any experiments involving human participants or animals performed by the authors.
Informed consent
Not required since this is a systematic review and meta-analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ali, S., Corbi, G., Medoro, A. et al. Relationship between monounsaturated fatty acids and sarcopenia: a systematic review and meta-analysis of observational studies. Aging Clin Exp Res 35, 1823–1834 (2023). https://doi.org/10.1007/s40520-023-02465-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02465-0