Abstract
Background
Total open thyroidectomy can be performed either with the conventional knot tying technique (nHS) or using the ultrasonically activated shears (harmonic scalpel, HS). The HS, developed in the ‘90s, initially used for laparoscopic surgery, is an innovative method for haemostasis that has been tested in thyroid surgery. Here, the use of the HS in conventional thyroid surgery compared with nHS is investigated in order to assess safety, cost-effectiveness, and the impact on the surgical outcome from an hospital and societal perspective.
Methods
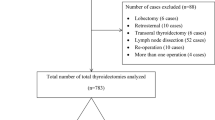
A randomized controlled trial was conducted at the University Hospital A. Gemelli in Rome from March 2007 till March 2008. Data refer to 198 patients eligible for total thyroidectomy (TT), randomized to either surgery with nHS (n = 96) or HS (n = 102) and followed for 3 months after hospital discharge. During hospitalization, operative time and resource consumption were recorded. Main clinical outcomes investigated were: pain (VAS score), quality of life (QoL, evaluated with EQ-5D), complications and cosmetic results. Direct medical and indirect costs were prospectively collected during the follow-up as well.
Results
The analysis was performed on 198 patients, mean age 51 years old, 46 male (23%) and 152 female (77%), randomized to either nHS group (n = 96) or HS (n = 102). The two groups were well balanced in terms of age, sex, preoperative diagnosis, anesthesia type and QoL at enrolment. A significantly shorter operative time (nHS: 76.36 vs HS: 54.16 minutes, p < 0.001) and total operating room (OR) occupancy time (100.59 vs 76.86 minutes, p < 0.001) were observed, even if length of hospital stay was similar in both groups (median 5 days). From a clinical point of view complication rates and voice changes showed no significant differences. No significant improvement in QoL was perceived in HS group at discharge (0.83 vs 0.78, p = 0.063), whilst at 1 month (0.90 vs 0.83, p < 0.002), and at 3 months after surgery (0.91 vs 0.84, p = 0.002) differences were statistically significant. A lower postoperative pain was reported by HS patients 6 hours after surgery (VAS: nHS: 44,56 vs HS: 41.35), but pain was similar after 48 hours (VAS: nHS: 20.97 vs HS: 22.75). 55% nHS patients were satisfied with scar’s cosmetic result vs 71% HS patients (p = 0.029) 1 month after surgery. The economic evaluation considered direct medical costs and indirect costs. Total direct medical costs were €2,540.52 and €2,400.34 for nHS and HS, respectively. From the hospital perspective, HS allows savings of €119/patient, mainly due to lower charges for OR staff (nHS: €452.90 vs HS: €294.19), OR utilization (nHS: €815.40 vs HS: €620.61), drugs (nHS: €93.28 vs HS: €63.29), and diagnostic tests (nHS: €160.36 vs HS: €132.91). From a societal perspective, HS is also related to lower medical resource consumption during a 3 month follow-up after discharge (nHS: €129.03 vs HS: €107.82) and lower non-medical resource utilization (transport/hotels costs: nHS: €535.51 vs HS: €342.77). No statistical difference was found in productivity losses up to 3 months (nHS: €377.71 vs HS: €385.51).
Conclusion
Harmonic is safe and effective in conventional TT, allowing a significant reduction of the operative time (−22 min), total OR utilization time (−24 min), and improvement in QoL at 3 months (HS: 0.23 vs nHS: 0.21), without increasing complication rates and saving €119 per patient from the hospital perspective. A positive impact on hospital resource consumption is also related to the surgical team skill in performing the TT. Harmonic should be adopted in TT to reduce impact on patient life and society, since it allows a overall saving of €325.36 per patient.
Similar content being viewed by others
Bibliografia
Amaral JF. The experimental development of an ultrasonically activated scalpel for laparoscopic use. Surg Laparoscop Endosc 1994; 4: 92–9
Amaral JF, Chrostek C. Depth of thermal injury: ultrasonically activated scalpel vs. electrosurgery. Surg Endosc 1995; 9: 226 [abstract]
Bellantone R, Lombardi CP, Bossola M, et al. Total thyroidectomy for management of benign thyroid disease: review of 526 cases. World J Surg 2002; 26: 1468–71
Cordón C, Fajardo R, Ramirez J, et al. A randomised, prospective, parallel group study comparing the harmonic scalpel to electrocautery in thyroidectomy. Surgery 2005; 137: 337–41
Giddings E. The history of thyroidectomy. J R Soc Med 1998; 91 (Suppl. 33): 3–6
Karvounaris DC, Antonopoulos V, Psarras K, Sakadamis A. Efficacy and safety of ultrasonically activated shears in thyroid surgery. Head Neck 2006; 28: 1028–31
Randolph GW. History of thyroid and parathyroid surgery. In: Donley S (editor). Surgery of the Thyroid and Parathyoid Glands. Philadelphia, PA: Saunders, 2003: 3–11
Shemen L. Thyroidectomy using the harmonic scalpel: analysis of 105 consecutive cases. Otolaryngol Head Neck Surg 2002; 127: 284–8
Siperstein A, Berber E, Morkoyun E. The use of the harmonic scalpel vs conventional knot tying for vessel ligation in thyroid surgery. Arch Surg 2002; 137: 137–42
Defechereux T, Rinken F, Maweja S, et al. Evaluation of the ultrasonic dissector in thyroid surgery. A prospective randomised study. Acta Chir Belg 2003; 103: 274–7
Hallgrimsson P, Lovén L, Westerdahl AB. Use of the harmonic scalpel versus conventional haemostatic techniques in patients with Grave disease undergoing total thyroidectomy: a prospective randomised controlled trial. Langenbecks Arch Surg 2008; 393: 675–80
Kilic M, Keskek M, Ertan T, et al. A prospective randomized trial comparing the harmonic scalpel with conventional knot tying in thyroidectomy. Adv Ther 2007; 24: 632–8
Miccoli P, Berti P, Dionisi G, et al. Randomized controlled trial of harmonic scalpel use during thyroidectomy. Arch Otolaryngol Head Neck Surg 2006; 132: 1069–73
Miccoli P, Berti P, Raffaelli M, et al. Comparison between minimally invasive video-assisted thyroidectomy and conventional thyroidectomy: a prospective randomized study. Surgery 2001; 130: 1039–43
http://www.prontuariofarmaceutico.it/ Accesso del 21/07/2010 ore 17:30
Regione Lazio. Nomenclatore Tariffario Prestazioni Specialistiche Ambulatoriali, DGR 731/05, DGR 143/06, DGR 922/06 e DGR 538/07
http://www.bancaditalia.it/pubblicazioni/econo/bollec/2007/bolls49/bollec49. Accesso del 21/7/2010 ore 17:20
McMillan C, Bradley C, Razvi S, et al. Psychometric evaluation of a new questionnaire measuring treatment satisfaction in hypothyroidism: the ThyTSQ. Value Health 2006; 9: 132–9
Briggs A. Statistical approaches to handling uncertainty in health economic evaluation. Eur J Gastroenterol Hepatol 2004; 16: 551–61
Briggs A. Probabilistic analysis of cost-effectiveness models: statistical representation of parameter uncertainty. Value Health 2005; 8: 1–2
Claxton K, Sculpher M, McCabe C, et al. Probabilistic sensitivity analysis for NICE technology assessment: not an optional extra. Health Econ 2005; 14: 339–47
Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10: 779–87
Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves-facts, fallacies and frequently asked questions. Health Econ 2004; 13: 405–15
Lombardi CP, Raffaelli M, Cicchetti A, et al. The use of “harmonic scalpel” versus “knot tying” for conventional “open” thyroidectomy: results of a prospective randomized study. Langen becks Arch Surg 2008; 393: 627–31
http://uif.bancaditalia.it/UICFEWebroot/index.jsp?whichArea=Cambi&lingua=it Accesso del 05/08/2010 ore 11.36
Ortega J, Sala C, Flor B, et al. Efficacy and cost-effectiveness of the UltraCision® harmonic scalpel in thyroid surgery: an analysis of 200 cases in a randomized trial. J Laparoendosc Adv Surg Tech A 2004; 14: 9–12
Stojadinovic A, Shaha AR, Orlikoff RF, et al. Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg 2002; 236: 823–32
Voutilainen PE, Haglund CH. Ultrasonically activated shears in thyroidectomies. A randomised trial. Ann Surg 2000; 231: 322–8
Yildirim O, Umit T, Ebru M, et al. Ultrasonic harmonic scalpel in total thyrodectomies. Adv Ther 2008; 25: 260–5
Viapiano J, Wards DS. Operating room utilization: the need for data. Int Anesthesiol Clin 2002; 38: 127–40
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dibidino, R., Ruggeri, M., Marchetti, M. et al. Lo studio HARMONIC: valutazione costo-efficacia dell’uso del bisturi a ultrasuoni negli interventi di tiroidectomia totale. Pharmacoeconomics-Ital-Res-Articles 12, 143–155 (2010). https://doi.org/10.1007/BF03320672
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03320672