Abstract
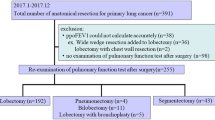
Objective: The effects of lung metastasectomy on respiration were evaluated. Subjects: From 1961 to 1999, 203 patients underwent lung metastasectomy. Of these, 102 patients who had undergone only partial lung resection, had undergone sufficient respiratory function testing, and had not suffered from other lung disease were included.Results: Unilateral thoracoscopic surgery caused less decrease in percent vital capacity than surgery through a posterolateral thoracotomy, in both the early (rate of decrease: 16.2±9.1 vs. 33.0±12.0%, p<0.01), and the late postoperative period (2.0±4.5 vs. 17.8±6.0%, p<0.0001). Two thoracoscopic operations caused less decrease in percent vital capacity than 2 operations through a posterolateral thoracotomy (21.3±13.8 vs. 61.1±8.1%, p=0.02). Bilateral metastasectomy through a median sternotomy caused less decrease in percent vital capacity than that through posterolateral thoracotomies (45.5±13.7 vs. 60.8±8.8%, p<0.05). Four (36%) of 11 patients who had undergone 3 or more metastasectomies exhibited dyspnea of degree 3 or higher on the Hugh-Jones classification.Conclusions: Thoracoscopic metastasectomy and metastasectomy through a median sternotomy caused less restrictive respiratory dysfunction than metastasectomy through a posterolateral thoracotomy. Since metastatic lung disease often necessitates repeated metastasectomy, and repeated metastasectomy often causes severe restrictive respiratory dysfunction, metastasectomy should be performed with a less invasive procedure.
Similar content being viewed by others
References
Hugh-Jones P, Lambert AV. A simple standard exercise test and its use for measuring exertion dyspnoea. Br Med J 1952; Jan 12: 65–71.
Pastorino U, Buyse M, Friedel G, Ginsberg RJ, Girard P, Goldstraw P, et al. Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg 1997; 113: 37–49.
Van Geel AN, Pastorino U, Jauch KW, Judson IR, Van Coevorden F, Buesa JM, et al. Surgical treatment of lung metastases. Cancer 1996; 77: 675–82.
Okubo T, Osaka Y, Narita Y, Iwai K, Nishibe T, Doke M, et al. Operation for pulmonary metastasis (100 cases). J Jpn Assoc Chest Surg 1995; 9: 2–8.
Ohbuchi T, Kohno T, Ohtsuka T, Nakajima J, Yagyu K, Furuse A. Comparison of pulmonary function after video assisted thoracoscopic surgery and after standard open thoracic surgery. J Jpn Assoc Chest Surg 1995; 9: 668–71.
Fujimura S, Kondo T, Yamauchi A, Okabe T, Handa M, Shionozaki F, et al. Evaluation of surgical treatment for metastatic lung tumor. J Jpn Assn Thorac Surg 1984; 32: 998–1004.
Sumitomo S. The influence of thoracotomy on the chest wall movement: difference between intercostal thoracotomy and median sternotomy. J Jpn Assn Thorac Surg 1988; 36: 1995–2004.
Kandioler D, Kromer E, Tuchler H, End A, Muller MR, Wolner E, et al. Long-term results after repeated surgical removal of pulmonary metastases. Ann Thorac Surg 1998; 65: 909–12.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ninomiya, M., Nakajima, J., Tanaka, M. et al. Effects of lung metastasectomy on respiratory function. Jpn J Thorac Cardiovasc Surg 49, 17–20 (2001). https://doi.org/10.1007/BF02913118
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02913118