Abstract
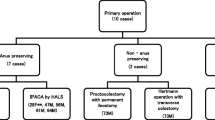
Preservation of the anal transitional zone (ATZ) after restorative proctocolectomy and stapled ileal pouch-anal anastomosis (IPAA) for ulcerative colitis is controversial. PURPOSE: To evaluate the incidence, risk factors, and treatment options for dysplasia and/or cancer after restorative proctocolectomy and stapled IPAA. METHODS: We reviewed the records of all 254 patients operated on for ulcerative colitis who had a restorative proctocolectomy, stapled IPAA, and annual postoperative biopsies of ATZ. Follow-up studies included an annual questionnaire and physical examination. RESULTS: During a follow-up of 2.3±1.4 (mean ± standard deviation) years, low-grade dysplasia was found in eight patients (3.1 percent), 16 (median: range, 6–56) months after surgery. Repeated biopsies revealed dysplasia in only two of eight patients, and completion mucosectomy was performed. Dysplasia in ATZ was associated with a preoperative (P=0.02) or postoperative (P=0.04) pathologic diagnosis of ulcerative colitis with concurrent dysplasia or cancer. No association (P>0.05) was found between dysplasia and the following: age, sex, preoperative length of disease, use of a double-stapledversus single-stapled technique, or anastomotic distance from the dentate line. CONCLUSIONS: Incidence of low-grade dysplasia in ATZ was low. Restorative proctocolectomy with total mucosectomy of the anal canal and handsewn IPAA is recommended for patients with preoperative diagnosis of ulcerative colitis and concurrent cancer or dysplasia. Frequent follow-up with biopsies is recommended for patients with incidental finding of cancer or high-grade dysplasia after restorative proctocolectomy and stapled IPAA with preservation of ATZ. For persistent or recurrent low-grade dysplasia, we recommend a completion mucosectomy
Similar content being viewed by others
References
Seow-Choen A, Tsunoda A, Nicholls RJ. Prospective randomized trial comparing anal function after hand sewn ileoanal anastomosis with mucosectomyversus stapled ileoanal anastomosis without mucosectomy in restorative procto-colectomy. Br J Surg 1991;78:430–4.
Tuckson WB, McNamara MJ, Fazio VW, Lavery IC, Oakley JR. Impact of anal manipulation and pouch design on ileal pouch function. JAMA 1989;83:1089–92.
Tuckson W, Lavery IC, Fazio VW, Oakley JR, Church JM, Milsom JW. Manometric and functional comparison of ileal pouch anal anastomosis with and without anal manipulation. Am J Surg 1991;161:90–6.
Lavery IC, Tuckson WB, Easley KA. Internal anal sphincter function after total abdominal colectomy and stapled IPAA without mucosal proctectomy. Dis Colon Rectum 1989;32:950–3.
Landi E, Fianchini A, Landa L,et al. Proctocolectomy and stapled ileoanal anastomosis without mucosal proctectomy. Int J Colorectal Dis 1990;5:151–6.
Lavery IC, Tuckson WB, Fazio VW, Oakley JR, Church JM, Milsom JW. Pouch surgery: the importance of the transitional zone. Can J Gastroenterol 1990;4:428–31.
O'Connell PR, Pemberton JH, Weiland LH,et al. Does rectal mucosa regenerate after ileoanal anastomosis? Dis Colon Rectum 1987;30:1–5.
Ambroze WL, Pemberton JH, Dozois RR, Carpenter HA. Does retaining the anal transition zone (ATZ) fail to extirpate chronic ulcerative colitis (CUC) after ileal pouch-anal anastomosis (IPAA)? [meeting abstract]. Dis Colon Rectum 1991;35:P20.
Tsunoda A, Talbot IC, Nicholls RJ. Incidence of dysplasia in the anorectal mucosa in patients having restorative proctocolectomy. Br J Surg 1990;77:506–8.
Riddell RH. Cancer and dysplasia in ulcerative colitis: an insoluble problem? Carcinoma of the large bowel and its precursors. New York: Alan R. Liss, 1985:77–90.
Woolrich AJ, Dasilva MD, Korelitz BI. Surveillance in the routine management of ulcerative colitis: the predictive value of low-grade dysplasia. Gastroenterology 1992;103:431–8.
Riddell RH, Goldman H, Ransohoff DF,et al. Dysplasia in inflammatory bowel disease: standard classification with provisional clinical applications. Hum Pathol 1983;14:931–68.
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. BMJ 1978;2:85–8.
Kmiot WA, Keighley MR. Totally stapled abdominal restoration proctocolectomy. Br J Surg 1989;79:961–4.
Williams NS, Marzouk DE, Hallan RI, Waldron DJ. Function after ileal pouch and stapled pouch-anal anastomosis for ulcerative colitis. Br J Surg 1989;76:1168–71.
Heppell J, Weiland H, Perrault J, Pemberton JH, Telander RL, Beart RW. Fate of rectal mucosa after rectal mucosectomy and ileoanal anastomosis. Dis Colon Rectum 1983;26:768–71.
Emblem R, Bergan A, Larsen S. Straight ileoanal anastomosis with preserved anal mucosa for ulcerative colitis and familial polyposis. Scand J Gastroenterol 1988;23:913–9.
Author information
Authors and Affiliations
Additional information
Read at the meeting of The American Society of Colon and Rectal Surgeons, Orlando, Florida, May 8 to 13, 1994.
About this article
Cite this article
Ziv, Y., Fazio, V.W., Sirimarco, M.T. et al. Incidence, risk factors, and treatment of dysplasia in the anal transitional zone after ileal pouch-anal anastomosis. Dis Colon Rectum 37, 1281–1285 (1994). https://doi.org/10.1007/BF02257797
Issue Date:
DOI: https://doi.org/10.1007/BF02257797