Abstract
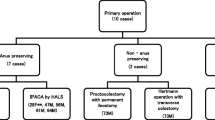
PURPOSE: Preservation of the anal transitional zone during ileal pouch-anal anastomosis is still controversial because of the risk of dysplasia and the theoretical risk of associated cancer. Without long-term follow-up data, the natural history and optimal treatment of anal transitional zone dysplasia are unknown. The aim of this study was to determine the long-term risk of dysplasia in the anal transitional zone and to evaluate the outcome of a conservative management policy for anal transitional zone dysplasia. METHODS: Two hundred ten patients undergoing anal transitional zone-sparing ileal pouch-anal anastomosis for ulcerative or indeterminate colitis between 1987 and 1992 and who were studied with serial anal transitional zone biopsies for at least five years postoperatively were included. Median follow up was 77 (range, 60–124) months. RESULTS: Anal transitional zone dysplasia developed in seven patients 4 to 51 (median, 11) months postoperatively. There was no association with gender, age, preoperative disease duration or extent of colitis, but the risk of anal transitional zone dysplasia was significantly increased in patients with prior cancer or dysplasia in the colon or rectum. Dysplasia was high grade in one and low grade in six. Two patients each with low-grade dysplasia detected on three separate occasions underwent mucosectomy 29 and 38 months after detection of low-grade dysplasia, but no cancer was found. The five other patients with dysplasia on one or two occasions were treated expectantly and were apparently dysplasia-free for a median of 72 (range, 48–100) months. CONCLUSIONS: Anal transitional zone dysplasia after ileal pouch-anal anastomosis is infrequent, is most common in the first two to three years postoperatively and may apparently disappear on repeated biopsy. Anal transitional zone preservation did not lead to the development of cancer in the anal transitional zone after five to ten years of follow-up. Long-term surveillance is recommended to monitor dysplasia. If repeat biopsy confirms persistent dysplasia, anal transitional zone excision with neoileal pouch-anal anastomosis is recommended.
Similar content being viewed by others
References
Fazio VW, Ziv Y, Church JM, Oakley JR, Lavery IC, Milsom JW, Schroeder TK. Ileal pouch-anal anastomoses complications and function in 1005 patients. Ann Surg 1995;222:120–7.
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. BMJ 1978;2:85–8.
Ziv Y, Fazio VW, Sirimarco MT, Lavery IC, Goldblum JR, Petras RE. Incidence, risk factors, and treatment of dysplasia in the anal transitional zone after ileal pouch-anal anastomosis. Dis Colon Rectum 1994;37:1281–5.
Riddell RH, Goldman H, Ransohoff DF,et al. Dysplasia in inflammatory bowel disease: standardized classification with provisional clinical applications. Hum Pathol 1983;14:931–68.
Fenger C. The anal transitional zone. Location and extent. APMIS 1979(Sect A);87:379–86:
Ziv Y, Fazio VW, Church JM, Lavery IC, King TM, Ambrosetti P. Stapled ileal pouch anal anastomoses are safer than handsewn anastomoses in patients with ulcerative colitis. Am J Surg 1996;171:320–3.
Miller R, Bartolo DC, Orrom WJ, Mortensen NJ, Roe AM, Cervro F. Improvement of anal sensation with preservation of the anal transitional zone after ileoanal anastomosis for ulcerative colitis. Dis Colon Rectum 1990;33:414–8.
Wexner SD. Ileal pouch anal function after endoanal mucosectomy and handsewn ileoanal anastomosis versus stapled anastomosis without mucosectomy. Eur J Surg 1995;161:922–3.
Sugerman HJ, Newsome HH, Decosta G,et al. Stapled ileoileoanal anastomosis for ulcerative colitis and familial polyposis coli without a temporary diverting ileostomy. Ann Surg 1991;213:606–19.
Lavery IC, Sirimarco MT, Ziv Y, Fazio VW. Anal canal inflammation after ileal pouch-anal anastomosis: the need for treatment. Dis Colon Rectum 1995;38:803–6.
Haray PN, Amarnath B, Weiss EG, Nogueras JJ, Wexner SD. Low malignant potential of the double-stapled ileal pouch-anal anastomosis. Br J Surg 1996;83:1406.
Emblem R, Bergan A, Larsen S. Straight ileo-anal anastomosis with preserved anal mucosa for ulcerative colitis and familial polyposis. Scand J Gastroenterol 1988;23:913–9.
Dixon MF, Brown LJ, Gilmour HM,et al. Observer variation in the assessment of dysplasia in ulcerative colitis. Histopathology 1988;13:385–97.
Tsunoda A, Talbot IC, Nicholls RJ. Incidence of dysplasia in the anorectal mucosa in patients having restorative proctocolectomy. Br J Surg 1990;77:506–8.
Woolrich AJ, DaSilva MD, Korelitz BI. Surveillance in the routine management of ulcerative colitis: the predictive value of low grade dysplasia. Gastroenterology 1992;103:431–8.
Axon AT. Colonic cancer surveillance is not essential in every patient. Eur J Cancer 1995;31A:1183–6.
Connell WR, Lennard-Jones JE, Williams CB, Talbot IC, Price AB, Wilkinson KH. Factors affecting the outcome of endoscopic surveillance for cancer in ulcerative colitis. Gastroenterology 1994;107:934–44.
Rugge M, Farinati F, Baffa R,et al. Gastric epithelial dysplasia in the natural history of gastric cancer: a multicentre prospective follow-up study. Gastroenterology 1994;107:1288–96.
Fazio VW, Tjandra JJ. Transanal mucosectomy: ileal pouch advancement for anorectal dysplasia or inflammation after restorative proctocolectomy. Dis Colon Rectum 1994;37:1008–11.
Sequens R. Cancer in the anal canal (transitional zone) after restorative proctocolectomy with stapled ileal pouch-anal anastomosis. Int J Colorectal Dis 1997;12:254–5.
Barrett M, Schoetz D, Semple J,et al. Long-term risk of neoplastic changes in ileoanal pouches in patients with ulcerative colitis [meeting abstract]. Dis Colon Rectum 1998;41(Suppl):A26.
Author information
Authors and Affiliations
About this article
Cite this article
O'Riordain, M.G., Fazio, V.W., Lavery, I.C. et al. Incidence and natural history of dysplasia of the anal transitional zone after ileal pouch-anal anastomosis. Dis Colon Rectum 43, 1660–1665 (2000). https://doi.org/10.1007/BF02236846
Issue Date:
DOI: https://doi.org/10.1007/BF02236846