Abstract
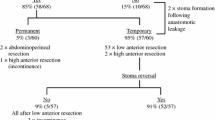
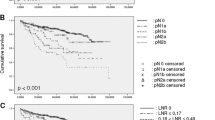
PURPOSE: The aim of this study was to determine whether the number of involved or uninvolved lymph nodes in resected specimens can be used to predict the effectiveness of surgical resection for rectal cancer. METHODS: Local recurrence and survival rates for 118 patients undergoing curative resection for rectal carcinoma, without adjuvant therapy, were retrospectively studied. RESULTS: Mean follow-up was 62±37 months. Mean number of involved or uninvolved lymph nodes per resected specimen was 12±7. Overall local recurrence rate was 15.2 percent. In patients without involved lymph nodes (N0 patients) and with T1 or T2 tumors, the local recurrence rate ranged from 0 to 8 percent (not significant), depending on the number of lymph nodes on the specimen. In patients without involved lymph nodes and those with T3 tumors, the actuarial survival rate at ten years was significantly lower (P<0.05), and the local recurrence rate was higher (P<0.02) in patients with fewer than ten lymph nodes than in those with more than ten nodes. In patients with involved lymph nodes, the mean number of nodes on the resected specimen correlated closely with the mean number involved by the tumor. CONCLUSION: The assessment of the effectiveness of rectal excision for cancer is in part helped by the number of involved or uninvolved lymph nodes found on the resected specimen. This is of particular interest in patients without involved lymph nodes and those having infiltrating T3 tumors, for whom the long-term survival and local recurrence rates were significantly better when more than ten lymph nodes were present. On the other hand, when fewer than ten nodes were found, whatever the cause, adjuvant radiotherapy had to be considered, because of the high risk of local failure rate.
Similar content being viewed by others
References
Krook JE, Moertel CG, Gunderson LL,et al. Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med 1991;324:709–15.
Adam IJ, Mohamdee MO, Martin IG,et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet 1994;344:707–11.
Hautefeuille P, Valleur P, Perniceni T,et al. Functional and oncologic results after coloanal anastomosis for low rectal carcinoma. Ann Surg 1988;207:61–4.
Abulafi AM, Williams NS. Local recurrence of colorectal cancer: the problem, mechanisms, management and adjuvant therapy. Br J Surg 1994;81:7–19.
Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1986;1:1479–82.
Enker WE, Thaler HT, Cranor ML, Polyak T. Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg 1995;181:335–46.
Reid JD, Robins RE, Atkinson KG. Pelvic recurrence after anterior resection and EEA stapling anastomosis for potentially curable carcinoma of the rectum. Am J Surg 1984;147:629–32.
Malassagne B, Valleur P, Serra J,et al. Relationship of apical lymph node involvement to survival in resected colon carcinoma. Dis Colon Rectum 1993;36:645–53.
Jass JR. Lymphocytic infiltration and survival in rectal cancer. J Clin Pathol 1986;39:585–9.
Pihl E, Malahy MA, Khankhanian N, Hersh EM, Mavligit GM. Immunomorphological features of prognostic significance in Dukes' Stage B colorectal carcinoma. Cancer Res 1977;37:4145–9.
Halvorsen TB, Seim E. Association between invasiveness, inflammatory reaction, desmoplasia and survival in colorectal cancer. J Clin Pathol 1989;42:162–6.
Fischer ER, Sass R, Palekar A, Fischer B, Wolmark N. Dukes' classification revisited: findings from the national surgical adjuvant breast and bowel projects (protocol R-01). Cancer 1989;64:2354–60.
Tang R, Wang J-Y, Chen J-S,et al. Survival impact of lymph node metastasis in TNM stage III carcinoma of the colon and rectum. J Am Coll Surg 1995;180:705–12.
Hermanek P, Sobin LH, eds. UICC TNM classification of malignant tumors. 4th ed. Berlin: Springer-Verlag, 1987:47–9.
Author information
Authors and Affiliations
About this article
Cite this article
Pocard, M., Panis, Y., Malassagne, B. et al. Assessing the effectiveness of mesorectal excision in rectal cancer. Dis Colon Rectum 41, 839–845 (1998). https://doi.org/10.1007/BF02235362
Issue Date:
DOI: https://doi.org/10.1007/BF02235362