Abstract
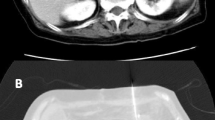
PURPOSE: Duodenal compression by the superior mesenteric artery following total proctocolectomy and ileal pouch-anal anastomosis is a rare occurrence. Previous surgical treatment involved duodenal division. The aim of this report was to describe a case with such a complication and to discuss an operative alternative. METHODS: Case report. RESULTS: Mobilization of the duodenum from its retroperitoneal attachments, without transection and reanastomosis, allowed the free passage of gas through the duodenum and recovery for the patient. CONCLUSION: This case report suggests that a more conservative approach may be successful in managing this complication.
Similar content being viewed by others
References
Taylor BM, Beart RW Jr, Dozois RR, Kelly KA, Wolff BG, Ilstrup DM. The endorectal ileal pouch-anal anastomosis: current clinical results. Dis Colon Rectum 1984;27: 347–50.
Ballantyne GH, Graham SM, Hammers L, Modlin IM. Superior mesenteric artery syndrome following ileal J-pouch anal anastomosis: an iatrogenic cause of early postoperative obstruction. Dis Colon Rectum 1987;30: 472–4.
Christie PM, Schroeder D, Hill GL. Persisting superior mesenteric artery syndrome following ileo-anal J pouch construction. Br J Surg 1988;75:1036.
Strong E. Mechanics of arteriomesenteric duodenal obstruction and direct surgical attack upon etiology. Ann Surg 1958;148:725–30.
Goes RN, Fagundes JJ, Coy CS, Amaral CA, Peres MA, Medeiros RR. The two-chamber ileal pelvic reservoir—an alternative design. Dis Colon Rectum 1993;36:403–4.
von Rokitansky K. Lehrbuch der pathologischen Anatomie, Vol. 2. Wein: W Braunmuller 1842:215.
Albrecht PA. Ueber arterio-mesenterialen darmver-schluss an der duodeno-jejunalgrenze und seine ursachliche beziehung zur magenerweiterung. Virchows Arch A Pathol Anat 1899;156:285–325.
Wayne E, Miller RE, Eiseman B. Duodenal obstruction by the superior mesenteric artery in bedridden combat casualties. Ann Surg 1971;174:339–45.
Simon M, Lerner MA. Duodenal compression by the mesenteric root in acute pancreatitis and inflammatory conditions of the bowel. Radiology 1970;94:75–81.
Ogbuokiri CG, Law EJ, MacMillan BG. Superior mesenteric artery syndrome in burned children. Am J Surg 1972;124:75–9.
Burnstein MJ, Schoetz DJ Jr, Coller JA, Veidenheimer MC. Technique of mesenteric lengthening in ileal reservoir-anal anastomosis. Dis Colon Rectum 1987;30:863–6.
Nicholls RJ. Restorative proctocolectomy with various types of anastomosis. World J Surg 1987;11:751–62.
Cherque D, Valleur P, Pernicerni T, Hautefeuille P. Inferior reach of ileal reservoir in ileoanal anastomosis. Dis Colon Rectum 1987;30:365–71.
Author information
Authors and Affiliations
Additional information
Dr. Goes is supported at the University of Southern California by grants from the Fundacao de Amparo a Pesquisa do Estado de Sao Paulo-FAPESP, Brazil.
About this article
Cite this article
Goes, R.N., Coy, C.S.R., Amaral, C.A. et al. Superior mesenteric artery syndrome as a complication of ileal pouch-anal anastomosis. Dis Colon Rectum 38, 543–544 (1995). https://doi.org/10.1007/BF02148857
Issue Date:
DOI: https://doi.org/10.1007/BF02148857