Abstract
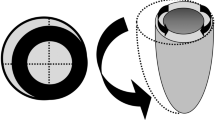
Temporary circulatory support with a pneumatic, axisymmetric, paracorporeal ventricular assist device (VAD) has been undertaken in 22 postcardiotomy patients. During VAD function, 9 patients demonstrated hemodynamic improvement (group I), and eventually, 8 of these stabilized sufficiently to permit device removal. Three remain alive and well up to 5 years postoperatively. The clinical course of 13 others (group II) was complicated by severe postoperative bleeding and abnormalities in renal function, leading to lack of hemodynamic improvement and death. In group I, the duration of cardiopulmonary bypass (CPB) ranged from 4.3 to 9.0 hr (mean 6.0 hr), and in group II, from 3.7 to 10.0 hr (mean 5.9 hr). The duration of VAD function was 125 hr (mean) in group I, and 25 hr (mean) in group II. Major hematologic abnormalities (secondary to prolonged CPB) included thrombocytopenia, abnormal platelet function studies, severe hypofibrinogenemia, and low levels of fibrinogen/fibrin degradation products. Efforts to develop a permanent, electrically powered ventricular assist system (VAS) for patients with irreversible cardiomyopathy and end-stage coronary artery disease are also progressing. In a recent series of animal experiments, 2 components of the VAS, an electromechanical energy converter and pusher-plate blood pump (stroke volume 85 ml) were evaluated (9 calves, 30–149 days). The bloodcontacting surfaces of the device consisted of textured fibrils to attract a fibrin coagulum. Conversion of this layer to a collagenous membrane was achieved by preliminary seeding of the pump with cultured, bovine fetal fibroblasts (5 calves). These were compared with 4 non-cell-seeded devices (controls), and functioned for longer periods without thromboembolic complications.
Résumé
Une assistance circulatoire temporaire a été mise en place chez 22 malades après chirurgie cardiaque en utilisant une pompe d'assistance ventriculaire paracorporelle pneumatique. Pendant le fonctionnement de cette assistance ventriculaire, 9 malades ont eu une amélioration hémodynamique (groupe I) dont 8 ont eu une stabilisation hémodynamique suffisante pour permettre d'arrêter l'assistance; 3 ont survécu et vont bien plus de 5 ans après l'intervention. L'évolution clinique de 13 autres malades (groupe II) a été compliquée par des hémorragies postopératoires abondantes, et des altérations de la fonction rénale entrainant une détérioration de l'hémodynamique et le décès. Pour les malades du groupe I, la durée de circulation extra-corporelle (en heure) allait de 4.3 à 9.0 (moyenne 6) et pour les malades du groupe II, de 3.7 à 10.0 (moyenne 5.9). La durée de l'assistance ventriculaire a été de 125 heures en moyenne pour le groupe I et de 25 heures en moyenne pour le groupe II. Les complications hématologiques (les plus graves dûes à une circulation extra-corporelle prolongée) furent des thrombocytopénies, des fonctions plaquettaires anormales, une diminution marquée du taux de fibrinogène et des produits de dégradation du fibrinogène. Des efforts pour développer un système d'assistance ventriculaire permanente, à energie électrique, pour les malades ayant des cardiomyopathies irreversibles et des coronaropathies au stade terminal, ont été tentés. Dans une série récente d'expérimentation animale, deux composantes de l'assistance ventriculaire: convertisseur d'energie electromécanique et pompe pulsée (de volume d'éjection 85 ml/s) ont été étudiées chez 9 veaux (30 à 149 jours). Les éléments en contact avec le sang de la pompe d'assistance furent recouverts d'un textile fibrillaire pour faciliter un dépôt de fibrine et la transformation de cette paroi en une membrane collagène fut réalisée par mise en culture sur la paroi de fibroblastes foetaux d'origine bovine (5 veaux). Ces pompes qui ont été comparées avec 4 pompes sans mise en place de culture cellulaire sur la paroi (à type de témoin) ont fonctionné pendant des durées plus importantes sans complication thrombo-embolique.
Resumen
El soporte circulatorio temporal ha sido emprendido en 22 pacientes post-cardiotomía mediante un sistema de asistencia mecánica ventricular (AMV) paracorpórea de tipo neumático interpuesto entre el apex del ventrículo izquierdo y la aorta. Durante la AMV, 9 pacientes demostraron mejoría hemodinámica (grupo I) y eventualmente 8 de estos lograron suficiente estabilidad para permitir la remoción del sistema. Tres continuaron vivos y en buenas condiciones hasta 5 años después de la operación. La evaluación clínica de los otros 13 (grupo II) resultó complicada por hemorragia postoperatoria severa y alteraciones en la función renal, lo cual, al impedir mejoría hemodinámica, resultó en defunción. En el grupo I la duración de la perfusión cardiopulmonar extracorpórea osciló entre 4.3 y 9.0 (promedio 6.0) horas, y en el grupo II entre 3.7 y 10.0 (promedio 5.9) horas. La duración de la AMV fué de 125 horas (promedio) en el grupo I, y de 25 horas (promedio) en el grupo II. Las alteraciones hematológicas mayores (secundarias a perfusión cardiopulmonar prolongada) incluyeron trombocitopenia, función plaquetaria anormal, hipofibrinogenia severa y bajos niveles de productos de degradación de fibrinógeno/fibrina. Los esfuerzos para desarrollar sistemas de asistencia ventricular (SAV) accionados eléctricamente para uso en pacientes con cardiomiopatía irreversible y con enfermedad coronaria terminal también están progresando. En una reciente serie de experimentos en animales, dos componentes de los SAV, un convertidor electromecánico de energía y una bomba de pistón de disco (volumen de eyección de 85 ml) fueron evaluados (9 terneros, 30–149 días). Las superficies de contacto sanguíneo del sistema son de fibrilla tejida para atraer un coágulo de fibrina. La conversión de esta capa a una membrana colagenosa fué lograda mediante la siembra preliminar de la bomba con fibroblastos bovinos fetales cultivados (5 terneros). Estos fueron comparados con 4 sistemas no sembrados con células (controles) y se encontró que funcionaron por períodos más prolongados y libres de complicaciones tromboembólicas.
Similar content being viewed by others
References
Filler, R.M., Bernhard, W.F., Robinson, T., Bankole, M.A., LaFarge, C.G.: An implantable left ventricular-aortic assist device. J. Thorac. Cardiovasc. Surg.54:795, 1967
Bernhard, W.F., Poirier, V., LaFarge, C.G., Carr, J.G.: A new method for temporary left ventricular bypass: Preclinical appraisal. J. Thorac. Cardiovasc. Surg.70:880, 1975
Bernhard, W.F., Stetz, J., Carr, J.G., Colo, N., McCormick, J., Fishbein, M.C.: Temporary left ventricular bypass: Factors affecting patient survival. Circulation60[Suppl. I]:I-131, 1979
Bernhard, W.F., Poirier, V.L., Carr, J.G.: A paracorporeal left ventricular assist device. Encyclopedia of Thoracic Surgery—Modern Techniques in Surgery, Cardio-Thoracic Surgery28:1, 1980
Bernhard, W.F., Clay, W., Schoen, F.J., Gernes, D., Sherman, C., Carr, J.G., Melaragno, A.J., Burke, D., Poirier, V.L., Valeri, C.R.: Clinical and laboratory investigations related to temporary and permanent ventricular bypass. Heart Transplant.3:16, 1983
Bernhard, W.F., LaFarge, C.G., Liss, R.H., Szycher, M., Berger, R.L., Poirier, V.L.: An appraisal of blood trauma and the prosthetic interface during left ventricular bypass in the calf and humans. Ann. Thorac. Surg.26:427, 1978
Bernhard, W.F., Poirier, V.L., LaFarge, C.G.: Relief of congenital obstruction to left ventricular outflow with a ventricular-aortic prosthesis. J. Thorac. Cardiovasc. Surg.69:223, 1975
Kean, J.F., Fellows, K.E., LaFarge, C.G., Nadas, A.S., Bernhard, W.F.: The surgical management of discrete and diffuse supravalvar aortic stenosis. Circulation54:112, 1976
Bernhard, W.F.: Clinical experience with the use of a valve-bearing conduit to construct a second left ventricular outflow tract in cases of unresectable intraventricular obstruction. Circulation54:323, 1976
Pierce, W.F., Parr, G.V.S., Myers, J.L., Pae, W.E., Bull, A.P., Waldhausen, J.A.: Ventricular-assist pumping in patients with cardiogenic shock after cardiac operations. N. Engl. J. Med.305:1606, 1981
Portner, P.M., Jassawalla, J.S., Chen, H., Conley, M.G., Lee, J.: Development of left heart assist blood pump. Devices and Technology Branch Contractors Program, 3, 1980
Schoen, F.J., Bernhard, W.F., Khuri, S.F., Koster, J.K., Van Devanter, S.J., Weintraub, R.M.: Pathologic findings in postcardiotomy patients managed with a temporary left ventricular assist pump. Am. J. Surg.143:508, 1982
Tennant, R., Wiggers, C.J.: The effect of coronary occlusion on myocardial contraction. Am. J. Physiol.112:351, 1935
Katz, A.M.: Effects of ischemia on the contractile processes of heart muscle. Am. J. Cardiol.32:456, 1973
Grossman, W., Barry, W.H.: Diastolic pressurevolume relations in the diseased heart. Fed. Proc.39:148, 1980
Leaf, A.: Cell swelling. A factor in ischemic tissue injury. Circulation48:455, 1973
Powers, E.R., DiBona, D.R., Powell, W.J.: The development of a perfusion deficit and myocardial cell swelling during low flow ischemia. Circulation58[Suppl. II]:II-175, 1978
Whalen, D.A., Jr., Hamilton, D.G., Ganote, C.E., Jennings, R.B.: Effects of a transient period of ischemia on myocardial cells. I. Effects on cell volume regulation. Am. J. Pathol.74:381, 1974
Schaper, J., Schwarz, F., Kittstein, H., Stämmler, G., Winkler, B., Scheid, H., Hehrlein, F.: The effects of global ischemia and reperfusion on human myocardium: Quantitative evaluation by electron microscopic morphometry. Ann. Thorac. Surg.33:116, 1982
Bethencourt, D.M., Laks, H.: Importance of edema and compliance changes during 24 hours of perservation of the dog heart. J. Thorac. Cardiovasc. Surg.81:440, 1981
Dennis, C., Hall, D.P., Moreno, J.R., Senning, Å.: Reduction of the oxygen utilization of the heart by left heart bypass. Circ. Res.10:298, 1962
Hughes, D.A., Igo, S.R., Daly, B.D., Migliore, J.J., Norman, J.C.: Effects of an abdominal left ventricular assist device on myocardial oxygen supply/demand ratios in normally perfused and ischemic bovine myocardium. Ann. Thorac. Surg.19:301, 1975
Pennock, J.L., Pae, W.E., Pierce, W.S., Waldhausen, J.A.: Reduction of myocardial infarct size: Comparison between left atrial and left ventricular bypass. Circulation59:275, 1979
Jennings, R.B., Reimer, K.A.: Factors involved in salvaging ischemic myocardium: Effect of reperfusion of arterial blood. Circulation68[Suppl. I]:I-25, 1983
Braunwald, E., Kloner, R.A.: Stunned myocardium prolonged post-ischemic ventricular dysfunction. Circulation66:1146, 1982
Bernhard, W.F., Gernes, D.G., Clay, W.C., Schoen, F.J., Burgeson, R., Valeri, R.C., Melaragno, A.J., Poirier, V.L.: Investigations with an implantable electrically-actuated ventricular assist device. J. Thorac. Cardiovasc. Surg.88:11, 1984
Rosenberg, G., Snyder, A., Weiss, W., Landis, D.L., Geselowitz, D.B., Pierce, W.S.: A cam-type electric motor-driven left ventricular assist device. J. Biomech. Eng.104:214, 1982
Whalen, R.L., Snow, J.L., Harasaki, H., Nose, Y.: Volume compensation for pulsatile blood pumps. Trans. Am. Soc. Artif. Intern. Organs27:110, 1981
Lee, S., Rosenberg, G., Donachy, J.H., Wisman, C.B., Pierce, W.S.: The compliance problem: A major obstacle in the development of implantable blood pumps. Artif. Organs8:82, 1984
Bernhard, W.F., Colo, N.A., Wesolowski, J.S., Szycher, M., Fishbein, M.C., Parkman, R., Franzblau, C., Haudenschild, C.C.: Development of collagenous linings on impermeable prosthetic surfaces. J. Thorac. Cardiovasc. Surg.79:552, 1980
Bernhard, W.F., Colo, N.A., Szycher, M., Wesolowski, J., Haudenschild, C.C., Franzblau, C.C., Parkman, R., Liss, R.: Development of a nonthrombogenic collagenous blood-prosthetic interface. Ann. Surg.192:369, 1980
Leung, D., Glagov, S., Mathews, M.: Cyclic stretching stimulates synthesis of matrix components by arterial smooth muscle in vitro. Science191:475, 1976
Hauscha, P., Lian, J.B., Gallop, P.M.: Direct identification of the calcium binding amino-acid, gammacarboxyglutamate in mineralized tissue. Proc. Natl. Acad. Sci. U.S.A.72:3925, 1975
Lian, J.B., Skinner, M., Gallop, P.M.: The presence of gamma-carboxyglutamic acid in the proteins associated with ectopic calcification. Biochem. Biophys. Res. Commun.71:349, 1976
Author information
Authors and Affiliations
Additional information
Supported in part by contracts NO1-HV-02914 and NO1-HV-12908, Devices and Technology Branch, NHLBI, NIH, Bethesda, Maryland.
Rights and permissions
About this article
Cite this article
Bernhard, W.F., Clay, W., Gernes, D. et al. Temporary and permanent left ventricular bypass: Laboratory and clinical observations. World J. Surg. 9, 54–64 (1985). https://doi.org/10.1007/BF01656256
Issue Date:
DOI: https://doi.org/10.1007/BF01656256