Abstract
The short and long-term effects of post-operative total parenteral nutrition (TPN) on body composition were studied in a randomised series of patients undergoing major colorectal surgery. Ninety-two patients (colorectal cancer: 50, ulcerative colitis or Crohn's disease: 42) were grouped according to diagnosis and clinical inflammatory activity. TPN was given for 9.7±1.1 days. The complication rate was not changed by the TPN. Nitrogen balance was studied during the first week. Body weight, total body potassium, triceps skinfold, serum albumin and body water were measured before and at intervals up to 24 weeks after the operation. Cumulative nitrogen balance in control patients at 7 days after surgery was −47.3 g. Patients given TPN balanced nitrogen intake and output (cancer patients and patients with quiescent inflammatory bowel disease, IBD) or were in positive balance (patients with active IBD). Weight loss at 1 week after surgery was less in TPN patients compared to controls and this difference remained statistically significant up to 6 months after termination of the nutritional treatment. A similar, although not statistically significant, difference was noted in total body potassium and triceps skinfold. Patients with active IBD regained pre-operative body composition earlier than cancer patients and patients with quiescent IBD. It is concluded that TPN after major colorectal surgery reduces postoperative weight loss and that this effect lasts after termination of the nutritional treatment. In the absence of increased body potassium and increased body water, we conclude that the long-term effect of TPN on body weight is most likely due to preservation of fat. Preservation of cell mass was only demonstrable at one week after surgery. The results show that weight loss continues after discharge from hospital irrespective of nutritional treatment. Patients with ongoing inflammatory activity showed a less profound catabolic response and regained pre-operative body composition earlier than patients with quiescent IBD. The normal neuro-endocrine response to major abdominal surgery includes a period of weight loss. This weight reduction is derived from loss of cell mass, fat and water [1]. The magnitude of the weight loss depends on the operative trauma, the individual patient's nutritional state and the nutritional therapy in the perioperative period [2]. It has been shown that postoperative total parenteral nutrition (TPN) prevents loss of body weight and negative nitrogen balance in the first postoperative week [3–6]. It is unclear, however, whether this short-term effect on body weight and nitrogen balance lasts beyond the immediate postoperative period.
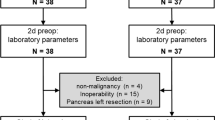
The purpose of this investigation was therefore to study, prospectively and under controlled conditions, the effects of a limited course of postoperative TPN on body composition. A comparison was made between patients operated on for colo-rectal carcinoma and those operated upon for ulcerative colitis (UC) or Crohn's disease (CD). It was also considered of interest to assess whether postoperative TPN alters the metabolic response to surgery differentially in patients with varying degrees of inflammatory activity.
Similar content being viewed by others
References
Kinney JM, Duke JH, Long CL, Gump FE (1979) Tissue fuel and weight loss after injury. J Clin Pathol 23:65–72
Richards JR (1977) Metabolic responses to injury, infection and starvation: an overview. In: Nutritional aspects of care in the critically ill. Churchill Livingstone, Edinburgh London New York, pp 273–302
Elwyn DH, Bryan-Brown CW, Shoemaker WC (1975) Nutritional aspects of body water dislocations in postoperative and depleted patients. Ann Surg 182:76–85
Elwyn DH, Gump FE, Iles M, Long CL, Kinney JM (1978) Protein and energy sparing of glucose added in hypocaloric amounts to peripheral infusions of amino acids. Metabolism 27:325–331
Macfie J, Smith RC, Hill GL (1981) Glucose or fat as a nonprotein energy source? Gastroenterology 80:103–107
Rush BF, Richardson JD, Griffen WO (1970) Positive nitrogen balance immediately after abdominal operations. Am J Surg 119:70–76
Talstad J, Gjone E (1976) The disease activity of ulcerative colitis and Crohn's disease. Scand Gastroenterol 11:403–408
Fasth S, Hultén L, Magnusson O, Nordgren S, Warnold I (1987) Postoperative complications in colorectal surgery in relation to preoperative clinical and nutritional state and postoperative nutritional treatment. Int J Colorect Dis 2:87–92
Hill GL, Church J (1984) Energy and protein requirements of general surgical patients requiring intravenous nutrition. Br J Surg 71:1–9
Guess CW, Werth R, Pollard M, Wood CD (1984) An assessment of nutritional depletion following major colonic surgery. Dis Colon Rectum 27:669–671
O'Keefe SJD, Sender PM, James WPT (1974) “Catabolic” loss of body nitrogen in response to surgery. Lancet 2:1035–1038
Young GA, Hill GL (1980) A controlled study of protein-sparing therapy after excision of the rectum. Ann Surg 192: 183–191
Gazzaniga AB, Day AT, Bartlett RH, Wilson AF (1976) Endogenous caloric sources and nitrogen balance. Arch Surg 111:1357–1361
Van Way III CW, Meng HC, Sandstead HH (1975) Nitrogen balance in postoperative patients receiving parenteral nutrition. Arch Surg 110:272–276
Jarnum S (1961) Plasma protein exudation in the peritoneal cavity during laparotomy. Gastroenterology 41:106–118
Mouridsen HT (1967) Turnover of human serum albumin before and after operations. Clin Sci 33:345–354
McNeill KG, Phil D, Harrison JE, Mernagh JR, Stewart S, Jeejeebhoy KN (1982) Changes in body protein, body potassium, and lean body mass during total parenteral nutrition. J Parenter Enter Nutr 6:106–108
Shizgal HM (1978) Symposium on nutritional requirements of the surgical patient. Can J Surg 21:483–506
Moore PJ, Magnall D, Clare RG (1982) The significance of hypoalbuminemia. In: Wesdorp R, Soeters PB (eds) Clinical nutrition 81. Churchill Livingstone, Edinburgh London New York pp 227–232
Beddoe AH, Hill GL (1985) Clinical measurement of body composition using in vivo neutron activation analysis. J Parenter Enter Nutr 9:504–520
Schiller WR, Long CL, Blakemore WS (1979) Creatinine and nitrogen excretion in seriously ill and injured patients. Surg Gynecol Obstet 149:561–566
Chettle DR, Fletcher JG, Downey SPMJ, Scott MC, James HM, Higgens CS (1982) Measurement of nitrogen in vivo by neutron activation analysis: further developments and applications. J Radioanal Chem 71:533–564
Filipsson S, Lindstedt G, Rehnberg O, Hultén L (1978) The metabolic consequences of surgery in Crohn's disease. Scand J Gastroenterol 13:471–479
Wood CD, Goumas W, Pollard M, Brinker JE (1984) Tissue nitrogen and potassium variation in trauma, starvation, and realimentation. J Parent Enter Nutr 8:665–667
Hessov I, Wara P (1978) Energi- og proteinindtagelse hos tarmresecerede patienter under hospitalsindlaeggelsen. Ugeskr Laeger 140:1469–1473
Christensen T, Kehlet H (1984) Postoperative fatigue and changes in nutritional status. Br J Surg 71:473–476
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fasth, S., Hultén, L., Magnusson, O. et al. The immediate and long-term effects of postoperative total parenteral nutrition on body composition. Int J Colorect Dis 2, 139–145 (1987). https://doi.org/10.1007/BF01647995
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01647995