Summary
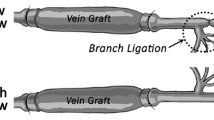
The development of a thickened (hyperplastic) fibro-cellular neo-intima is a significant event in the adaptation of a vein grafted into an artery. The histogenesis of tissues in vein grafts was explored in a rat model where the source of endothelial and smooth muscle cells was from the adjacent artery. Cell proliferation was assessed by the incorporation of tritiated thymidine and autoradiography, up to 18 months after grafting. Cell migration was detected by prelabelling in the first 5 days after grafting and sampling at later times. The proliferation of cells in the arterial media adjacent to the graft was elevated above control levels as early as 2 days after grafting; it was maximal at 3 days and returned to low levels by day 21. During the first week, prelabelled smooth muscle cells in the tunica media of the adjacent artery migrated to the subendothelial space, where they continued to proliferate to produce arterial intimal hyperplasia. The migration of endothelial and smooth muscle cells proceeded across the anastomosis to populate the vein graft neo-intima, where smooth muscle cells continued to proliferate until 28 days after grafting. Cell migration and proliferation were significant factors in the histogenesis of vein graft neo-intimal hyperplasia in this model. These processes were controlled, perhaps by local regulatory factors, to form a vein graft, the wall of which was similar in thickness and structure to that of the host artery.
Similar content being viewed by others
References
Baumgartner HR, Studer A (1978) Smooth muscle cell proliferation and migration after removal of arterial endothelium in rabbits. In: Schettler G (ed) Atherosclerosis is it reversible? Springer, Berlin pp 1–39
Brody WR, Angel WW, Kosek JC (1972) Histologic fate of the venous coronary artery bypass in dogs. Am J Pathol 66:111–119
Bush HL, Jakubowski JA, Curl GR, Deykin D, Nabsetch DC (1986) The natural history of endothelial structure and function in arterialized vein grafts. J Vasc Surg 3:204–215
Campbell GR, Campbell JH (1985) Smooth muscle cell phenotypic changes in arterial wall homoeostasis: implications for the pathogenesis of atherosclerosis. Exp Mol Pathol 42:139–162
Campbell GR, Campbell JH, Manderson JA, Horrigan S, Rennick RE (1988) Arterial smooth muscle. A multifunctional mesenchymal cell. Arch Pathol Lab Med 112:977–986
Campbell PC, McGeachie JK, Prendergast FJ (1981) Vein grafts for arterial repair: Their success and reasons for failure. Ann Roy Coll Surg Engl 63:257–260
Castellot JJ, Addonizzio ML, Rosenberg R, Karnovsky MJ (1981) Cultured endothelial cells produce a heparin like inhibitor of smooth muscle cell growth. J Cell Biol 90:372–379
Chang LO, Looney WB (1965) A biochemical and autoradiographic study of the in vitro utilization of tritiated thymidine in regenerating liver. Cancer Res 25:1817–1827
Cleaver JE (1967) Thymidine metabolism and cell kinetics. North Holland, Amsterdam
Clowes AW, Clowes MM (1985) Kinetics of cellular proliferation after arterial injury. II. Inhibition of smooth muscle growth by heparin. Lab Invest 52:611–616
Clowes AW, Clowes MM (1986) Kinetics of cell proliferation after arterial injury. IV Heparin inhibits rat smooth muscle mitogenesis and migration. Circ Res 58:839–845
Clowes AW, Schwartz SM (1985) Significance of quiescent smooth muscle cell migration in the injured rat carotid artery. Circ Res 56:139–145
Clowes AW, Reidy MA, Clowes MM (1983) Kinetics of cellular proliferation after arterial injury. I. Smooth muscle cell grown in the absence of endothelium. Lab Invest 49:327–333
Clowes AW, Gown AM, Hanson SR, Reidy MA (1985) Mechanisms of arterial graft failure. I. Role of cellular proliferation in early healing of PTFE prostheses. Am J Pathol 118:43–54
Diderholm H, Fichthelius KE, Linder O (1962) Availability time of 3H-label after administration of 3H-thymidine in vivo. Exp Cell Res 27:431–435
Dilley RJ, McGeachie JK (1983) Block staining with p-phenylenediamine for light microscope autoradiography. J Histochem Cytochem 31:1015–1018
Dilley RJ, McGeachie JK, Prendergast FJ (1986) A morphometric study of vein graft intimal hyperplasia. Plast Recon Surg 77:451–454
Dilley RJ, McGeachie JK, Prendergast FJ (1988) A review of the histologic changes in vein-to-artery grafts, with particular reference to intimal hyperplasia. Arch Surg 123:691–696.
Dobrin PB, Littooy FN, Golan J, Blackeman B, Fareed J (1988) Mechanical and histological changes in canine vein grafts. J Surg Res 44:259–265
Drysji M, Mikat E, Bjornsson TD (1988) Inhibition of intimal hyperplasia after arterial injury by heparins and heparinoid. J Vasc Surg 8:623–633
Fritze LMS, Reilly CF, Rosenberg RD (1985) An antiproliferative heparan sulfate species produced by post-confluent smooth muscle cells. J Cell Biol 100:1014–1019
Fuchs JCA, Mitchener JS, Hagen PO (1978) Post-operative changes in autologous vein grafts. Ann Surg 188:1–15
Liu WM, Roubin GS, King SB (1989) Restenosis after coronary angioplasty. Circulation 79:1374–1387
Luscher TF (1989) Endothelium-dependant relaxing and contracting factors: potential role in coronary artery disease. Eur Heart J 10:847–857
Majack RA, Clowes AW (1984) Inhibition of vascular smooth muscle cell migration by heparin-like glycosaminoglycans. J Cell Physiol 118:253–256
McGeachie JK (1975) Smooth muscle regeneration. Monogr Dev Biol 9:1–99
McGeachie JK, Campbell PA, Prendergast FJ (1981) Vein to artery grafts. A quantitative study of the revascularisation by vasa vasorum and its relationship to intimal hyperplasia. Ann Surg 194:100–107
McGeachie JK, Meagher S, Prendergast FJ (1989) Vein-to-artery grafts: The long-term development of neo-intimal hyperplasia and its relationship to vasa vasorum and sympathetic innervation. Aust NZJ Surg 59:59–65
McMillan GC, Stary HC (1968) Preliminary experience with mitotic activity of cellular elements in the atherosclerotic plaques of cholesterol-fed rabbits studied by labelling with tritiated thymidine. Ann NY Acad Sci 149:699–709
Nakao J, Ooyama T, Chang W-C, Murota S, Orimo H (1982) Platelets stimulate aortic smooth muscle cell migration in vitro. Involvement of 12-L-hydrozy-5,8,10,14-eicosatetraenoic acid. Atherosclerosis 43:143–150
Nilsson J, Sjolund M, Palmberg L, Thyberg J, Heldin CH (1985) Arterial smooth muscle cells in primary culture produce PDGF-like protein. Proc Natl Acad Sci USA 82:4418–4422
Prendergast FJ, McGeachie JK, Fabre JW, Winearls CG Morris PJ (1979) Vein allografts for arterial replacement in rats: an immunological and histological study. Transplantation 27:49–54
Schwartz SM, Campbell GR, Campbell JH (1986) Replication of smooth muscle cells in vascular disease. Circ Res 58:427–444
Seppa H, Grotendorst G, Seppa S, Schiffmann E, Martin GR (1982) Platelet-derived growth factor is chemotactic for fibroblasts. J Cell Biol 92:584–588
Sjolund M, Sejersen T, Heldin CH, Thymberg J (1988) Arterial smooth muscle cells express platelet-derived growth factor (PDGF) A chain mRNA, secrete a PDGF-like mitogen, and binds exogenous PDGF in a phenotype- and growth state-dependant manner. J Cell Biol 106:403–413
Spaet TH, Stemerman MB, Veith J, Lejnieks I (1975) Intimal injury and regrowth in the rabbit aorta. Medial smooth muscle cells as a source of neointima. Circ Res 36:58–69
Spraragen SC, Bond VP, Dahl LK (1962) Role of hyperplasia in vascular lesions of cholesterol-fed rabbits studied with thymidine-H3 autoradiography. Circ Res 11:329–336
Szilagyi DE, Elliot JP, Hageman JH, Smith RF, Dall'olmo CA (1973) Biologic fate of autogenous vein implants as arterial substitutes. Ann Surg 178:232–246
Tennant M, McGeachie JK (1990) Blood vessel structure and function: a brief update on recent advances. Aust N Z J Surg 60:747–753
Tennant M, McGeachie JK, Dilley RJ, Prendergast FJ (1990) Histogenesis of arterial intimal hyperplasia and atherosclerosis. Aust N Z J Surg 60:79–85
Vanhoutte PM (1988) Platlets, endothelium and the blood vessel wall. Experimentia 44:105–108
Webster WS, Bishop SP, Geer JC (1974) Experimental aortic intimal thickening. I. Morphology and source of intimal cells. Am J Pathol 76:245–259
Wilcox JN, Smith KM, Schwartz SM, Gordon D (1988) Platelet derived growth factor mRNA detection in human atherosclerotic plaques by in-situ hybridisation. J Clin Invest 82:1134–1143
Winkles JA, Friesel R, Burgess WH (1987) Human vascular smooth muscle cells both express and respond to heparin-binding growth factor I (endothelial cell growth factor). Proc Natl Acad Sci USA 84:7124–7128
Zwolach RM, Adams MC, Clowes AW (1987) Kinetics of vein graft hyperplasia: Association with tangential stress. J Vasc Surg 5:126–136
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Dilley, R.J., McGeachie, J.K. & Tennant, M. The role of cell proliferation and migration in the development of a neo-intimal layer in veins grafted into arteries, in rats. Cell Tissue Res 269, 281–287 (1992). https://doi.org/10.1007/BF00319619
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00319619