Abstract
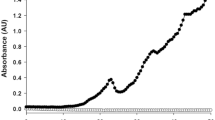
Total cellular creatine content is an important bioenergetic parameter in skeletal muscle. To understand its regulation we investigated creatine transport and accumulation in the G8 cultured skeletal myoblast line. Like other cell types, these contain a creatine transporter, whose activity, measured using a radiolabelling technique, was saturable (Km = 110 ± 25 μM) and largely dependent on extracellular [Na+]. To study sustained influences on steady state creatine concentration we measured total cellular creatine content using a fluorimetric method in 48 h incubations. We found that the total cellular creatine content was relatively independent of extracellular creatine concentration, consistent with high affinity sodium-dependent uptake balanced by slow passive efflux. Accordingly, in creatine-free incubations net creatine efflux was slow ( 5 ± 1 % of basal creatine content per day over 6 days), while creatine content in 48 h incubations was reduced by 28 ± 13% of control by the Na+,K+-ATPase inhibitor ouabain. Creatine accumulation after 48 h was stimulated by treatment with the mixed α- and β-adrenergic agonist noradrenaline, the β-adrenergic agonist isoproterenol, the β2-agonist clenbuterol and the cAMP analogue N6,2′-O-dibutyryladenosine 3′,5′-cyclic monophosphate, but was unaffected by the α1 adrenergic agonist methoxamine. The noradrenaline enhancement of creatine accumulation at 48 h was inhibited by the mixed α- and β-antagonist labetalol and by the β-antagonist propranolol, but was unaffected by the α2 antagonist phentolamine; greater inhibition was caused by the β2 antagonist butoxamine than the β1 antagonist atenolol. Creatine accumulation at 48 h was increased to 230 ± 6% of control by insulin and by 140 ± 13% by IGF-I (both at 3 nM). Creatine accumulation at 48 h was also increased to 280 ± 40% of control by 3,3′,5-triiodothyronine (at 70 μM) and to 220 ± 35% of control by amylin (60 nM). As 3,3′,5-triiodothyronine, amylin and isoproterenol all stimulate the Na+,K+-ATPase, we suggest that they stimulate Na+-creatine cotransport indirectly by increasing the transmembrane [Na+] concentration gradient and membrane potential.
Similar content being viewed by others
Abbreviations
- IGF-I:
-
insulin-like growth factor I
- IGF-II:
-
insulin-like growth factor II
- T3 :
-
3,3′,5-triiodothyronine
- CGRP:
-
calcitonin gene-related peptide
References
Walliman T, Wyss M, Brdiczka D, Nicolay K, Eppenberger HM: Intracellular compartmentation, structure and function of creatine kinase isoenzymes in tissues with high and fluctuating energy demands: the ‘phosphocreatine circuit’ for cellular energy homeostasis. Biochem J 281:21–40, 1992
Meyer RA: Linear dependence of muscle phosphocreatine kinetics on total creatine content. Am J Physiol 257: C1149-C1157, 1989
Loike JD, Somes M, Silverstein SC: Creatine uptake, metabolism and efflux in human monocytes and macrophages. Am J Physiol 251: C128–135, 1986
Loike JD, Zalutsky DL, Kaback E, Miranda AF, Silverstein SC: Extracellular creatine transport in rat and human muscle cells. Proc Natl Acad Sci USA 85: 807–811, 1988
Ku C-P, Passow H: Creatine and creatine transport in old and young human red blood cells. Biochim Biophys Acta 600: 212–227, 1980
Bennett SE, Bevington A, Walls J: Regulation of intracellular creatine in erythrocytes and myoblasts: influence of uraemia and inhibition of Na,K-ATPase. Cell Biochem Funct 12: 99–106, 1994
Guimbal C, Kilimann MW: A Na+-dependent creatine transporter in rabbit brain, muscle heart and kidney. J Biol Chem 268: 8418–8421, 1993
Schloss P, Mayser W, Betz H: The putative rat choline transporter CHOT 1 transports creatine and is highly expressed in neural and muscle-rich tissues. Biochem Biophys Res Commun 198: 637–645, 1994
Greenhaff PL, Casey A, Short AH, Harris R, Söderlund K, Hultman E: Influence of oral creatine supplementation on muscle torque during repeated bouts of maximal voluntary exercise in man. Clin Sci 84: 567–571, 1993
Harris RC, Söderlund K, Hultman E: Elevation of creatine in resting and exercised muscle of normal subjects by creatine supplementation. Clin Sci 83: 367–374, 1992
Gordon A, Hultman E, Kaijser L, Kristjansson S, Rolf CJ, Nyquist O, Sylven C: Creatine supplementation in chronic heart failure increases skeletal muscle creatine phosphate and muscle performance. Cardiovasc Res 30: 413–418, 1995
Sipila I, Rapola J, Simell O, Vaunas O: Supplementary creatine as a treatment for gyrate atrophy of the choroid and retina. N Engl J Med 304:867–870, 1981
Bessman SP, Mohan C: In: P. DeDeyn, B. Marescau, V. Stalon, I. Quesli (eds). Guanidino compounds in biology and medicine. John Libbey, London, 1992, pp 181–187
Ingwall JS, Kramer MF, Fifer MA, Lorell BH, Shemin R, Grossman W, Allen PD: The creatine kinase system in normal and diseased myocardium. New Eng J Med 313: 1050–1054, 1985
Kemp G, Bevington A: The regulation of intracellular orthophosphate concentration. J Theor Biol 161: 77–94, 1993
Andersen SLV, Clausen T, Calcitonin gene-related peptide stimulates active Na+-K+ transport in rat soleus muscle. Am J Physiol 264: C419-C429, 1993
Zhu G, Dudley TD, Saltiel AR: Amylin increases cyclic AMP formation in L6 myocytes through calcitonin gene-related peptide receptors. Biochem Biophys Res Commun 177: 771–775, 1991
Seppet EK, Adoyaan AJ, Kallikorm AP, Chemousova GB, Lyulina NV, Sharov VG, Severin VV, Popovich MI, Saks VA: Hormone regulation of cardiac energy metabolism. Biochem Med 34: 267–279, 1985
Otten JV, Fitch CD, Wheatley JB, Fischer VW: Thyrotoxic myopathy in mice: accentuation by a creatine transport inhibitor. Metabolism 35:481–484, 1986
Polgreen KE, Kemp GJ, Leighton B, Radda GK: Modulation of Pi transport in skeletal muscle by insulin and IGF-1. Biochim Biophys Acta 1223: 279–284, 1994
Marette A, Krischer J, Lavoie L, Ackerley C, Carpentier J-L, Klip A: Insulin increases the Na+-K+-ATPase α2-subunit in the surface of rat skeletal muscle: morphological evidence. Am J Physiol 265: C716-C1722, 1993
Brodie C, Sampson SR: Characterisation of thyroid hormone effects on Na-K pump and membrane potential of cultured rat skeletal muscle. Endocrinology 123: 891–897, 1988
Clausen T, Flatman JA: β2- adrenoceptors mediate the stimulating effect of adrenaline on active electrogenic Na-K transport in rat soleus muscle. Br J Pharmacol 68: 749–755, 1980
Clausen T, Flatman JA: The effect of catecholamines on Na-K transport and membrane potential in rat soleus membrane. J Physiol (Lond) 270:383–414, 1977
Odoom JE, Kemp GJ, Radda GK: Control of intracellular creatine condentration in a mouse myoblast cell line. Biochem Soc Trans 21: 441S, 1993
Radda GK, Odoom J, Kemp GJ, Taylor DJ, Thompson CH, Styles P: Assessment of mitochondrial function and control in normal and diseased states. Biochim Biophys Acta 1271: 15–19, 1995
Conn RB: Fluorimetric determination of creatine. Clin Chem 6: 537–548, 1960
Lowry OH, Roseborough NJ, Farr AL, Randall RJ: Protein measurement with the Folin reagent. J Biol Chem 193: 265–275, 1951
Kemp GJ: The susceptibility of calibration methods to errors in the analytical signal. Anal Chim Acta 176: 229–247, 1985
Cornish-Bowden A: Analysis of enzyme-kinetic data. OUP, Oxford, 1995
Marescau B, DeDeyn P, Wiechert P, vanGorp L, Lowenthal A: Comparative study of guanidino compounds in serum and brain of mouse, rat, rabbit and man. J Neurochem 46: 717–720, 1986
Walker JB: Creatine: biosynthesis, regulation and function. Adv Enzymol 50: 177–242, 1979
Syllm-Rapoport I, Daniel A, Rapoport S: Creatine transport into red blood cells. Acta Biol Med Germ 39: 771–779, 1980
Syllm-Rapoport I, Daniel A, Starck H, Goetze W, Hartwig A, Gross J, Rapoport S: Creatine in red cells: transport and erythropoeitic dynamics. Acta Biol Med Germ 40: 653–659, 1981
Möller A, Hamprecht B: Creatine transport in cultured cells of rat and mouse brain. J Neurochem 52: 544–550, 1989
Masson S, Quistorff B: Kinetics of creatine uptake in the perfused mouse liver: a 31P-n.m.r. study of transgenic mice expressing creatine kinase (CKBB) in the liver. Biochem J 303: 531–538, 1994
Bloch K, Schoenheimer R, Rittenberg D: Rate of formation and disappearance of body creatine in normal animals. J Biol Chem 138: 155–165, 1941
Hansch CH, Leo A: Substituent constants for correlation analysis in chemistry and biology. Wiley-Interscience, New York, 1979, pp
Odoom JE, Campbell ID, Ellory JC, King GF: Characterisation of peptide fluxes into human erythrocytes. Biochem J 267: 141–147, 1990
Perez-Llamas F, Lopez JA, Zamora S: The digestive and metabolic utilization of the dietary protein: effect of clenbuterol and protein level. Arch Int Physiol Biochim Biophys 100: 27–31, 1992
Choo JJ, Horan MA, Little RA, Rothwell NJ: Anabolic effects of clenbuterol on skeletal muscle are mediated by beta 2-adrenoceptor activation. Am J Physiol 263: E50-E56, 1992
Sillence MN, Matthews ML, Spiers WG, Lindsay DB: Effects of clenbuterol, ICI 118551 and sotalol on the growth of cardiac and skeletal muscle and on beta 2-adrenoceptor density in female rats. Naunyn Schmiedeberg Arch Pharmacol 344: 449–453, 1991
Humbel R: Insulin-like growth factors I and II. Eur J Biochem 190: 445–462, 1990
Seraydarian MW, Artaza L: Regulation of energy metabolism by creatine in cardiac and skeletal muscle cells in culture. J Mol Cell Cardiol 8:669–678, 1976
Kemp G, Polgreen K, Radda G: Skeletal muscle Pi transport and cellular [Pi] studied in L6 myoblasts and rabbit muscle-membrane vesicles. Bioch Biophys Acta 1137: 10–18, 1992
Leighton B, Cooper GJS: Pancreatic amylin and calcitonin gene-related peptide cause resistance to insulin in skeletal muscle in vivo. Nature 335: 632–635, 1988
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Odoom, J.E., Kemp, G.J. & Radda, G.K. The regulation of total creatine content in a myoblast cell line. Mol Cell Biochem 158, 179–188 (1996). https://doi.org/10.1007/BF00225844
Issue Date:
DOI: https://doi.org/10.1007/BF00225844