Abstract
Cardiac output measurement is still regarded as one of the key hemodynamic variables in the assessment of cardiac function and as an essential measure for guiding the therapy of critically ill patients. In order to achieve adequate oxygen delivery (DO2), hemodynamic monitoring is necessary in order to provide appropriate cardiovascular support [1]. Although measurements of regional perfusion and oxygenation are gaining increasing attention, cardiac output measurement is still regarded as the key hemodynamic variable in the assessment of cardiac function and to guide therapy. Flow, as gauged by cardiac output, is the key measure of how well the circulation is delivering oxygen and nutrients to the vital organs and is the focus of all resuscitation efforts. Traditionally a pulmonary artery catheter (PAC) has been used for measuring pulmonary arterial pressures and cardiac output by thermodilution techniques in order to guide fluid therapy and hemodynamic manipulation. There have been serious concerns about the risk-benefit ratio of using pulmonary artery occlusion pressure (PAOP) as a measure of cardiac preload and recent studies have suggested a lack of benefit in some patient groups using the PAC [2]72-[4]. Recently, in a cohort of patients undergoing major non-cardiac surgery, it was demonstrated that the use of the PAC provides no benefit [5]. Among patients with severe sepsis, PAC placement was not associated with a change in mortality rate or resource use, although small non-significant trends towards a lower resource use were present in the PAC group [6]. In a consensus statement of the National Heart, Lung, and Blood Institute (NHLBI) and the Food and Drug Administration (FDA) PAC use was not recommended for elective major surgery [7].
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Preview
Unable to display preview. Download preview PDF.
Similar content being viewed by others
References
Pinsky MR (2003) Hemodynamic monitoring in the intensive care unit. Clin Chest Med 24:549–560
Connors AF Jr, Speroff T, Dawson NV, et al (1996) The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA 276:889–897
Weil MH (1998) The assault on the Swan-Ganz catheter: a case history of constrained technology, constrained bedside clinicians, and constrained monetary expenditures. Chest 113:1379–1386
Harvey S, Harrison DA, Singer M, et al (2005) Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet 366:472–477
Polanczyk CA, Rohde LE, Goldman L, et al (2001) Right heart catheterization and cardiac complications in patients undergoing noncardiac surgery: an observational study. Jama 286: 309–314
Yu DT, Platt R, Lanken PN, et al (2003) Relationship of pulmonary artery catheter use to mortality and resource utilization in patients with severe sepsis. Crit Care Med 31:2734–2741
Bernard GR, Sopko G, Cerra F, et al (2000) Pulmonary artery catheterization and clinical outcomes: National Heart, Lung, and Blood Institute and Food and Drug Administration Workshop Report. Consensus Statement. Jama 283:2568–2572
Sandham JD, Hull RD, Brant RF, et al (2003) A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med 348:5–14
Wesseling KH, de Wit B, Weber J, Smith N (1983) A simple device for the continuous measurement of cardiac output. Adv Cardiovasc Physiol 5:16–52
Goedje O, Hoeke K, Lichtwarck-Aschoff M, et al (1999) Continuous cardiac output by femoral arterial thermodilution calibrated pulse contour analysis: comparison with pulmonary arterial thermodilution. Crit Care Med 27:2407–2412
Hofer CK, Ganter MT, Zollinger A (2007) What technique should I use to measure cardiac output? Curr Opin Crit Care 13:308–317
Hoeft A, Schorn B, Weyland A, et al (1994) Bedside assessment of intravascular volume status in patients undergoing coronary bypass surgery. Anesthesiology 81:76–86
Godje O, Hoke K, Goetz AE, et al (2002) Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med 30:52–58
Felbinger TW, Goepfert MS, Goresch T, et al (2005) Accuracy of pulse contour cardiac index measurements during changes of preload and aortic impedance. Anaesthesist 54:755–762
Bein B, Worthmann F, Tonner PH, et al (2004) Comparison of esophageal Doppler, pulse contour analysis, and real-time pulmonary artery thermodilution for the continuous measurement of cardiac output. J Cardiothorac Vasc Anesth 18:185–189
Marx G, Schuerholz T, Sumpelmann R, et al (2005) Comparison of cardiac output measurements by arterial trans-cardiopulmonary and pulmonary arterial thermodilution with direct Fick in septic shock. Eur J Anaesthesiol 22:129–134
Schuerholz T, Meyer MC, Friedrich L, et al (2006) Reliability of continuous cardiac output determination by pulse-contour analysis in porcine septic shock. Acta Anaesthesiol Scand 50:407–413
Spohr F, Hettrich P, Bauer H, et al (2007) Comparison of two methods for enhanced continuous circulatory monitoring in patients with septic shock. Intensive Care Med 33:1805–1810
Halvorsen PS, Espinoza A, Lundblad R, et al (2006) Agreement between PiCCO pulse-contour analysis, pulmonal artery thermodilution and transthoracic thermodilution during off-pump coronary artery by-pass surgery. Acta Anaesthesiol Scand 50:1050–1057
Yamashita K, Nishiyama T, Yokoyama T, et al (2005) Cardiac output by PulseCO is not interchangeable with thermodilution in patients undergoing OPCAB. Can J Anaesth 52:530–534
Sander M, von Heymann C, Foer A, et al (2005) Pulse contour analysis after normothermic cardiopulmonary bypass in cardiac surgery patients. Crit Care 9:R729–734
Button D, Weibel L, Reuthebuch O, et al (2007) Clinical evaluation of the FloTrac/Vigileo system and two established continuous cardiac output monitoring devices in patients undergoing cardiac surgery. Br J Anaesth 99:329–336
Uchino S, Bellomo R, Morimatsu H, et al (2006) Pulmonary artery catheter versus pulse contour analysis: a prospective epidemiological study. Crit Care 10:R174
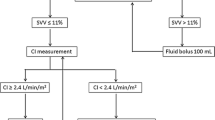
Berkenstadt H, Margalit N, Hadani M, et al (2001) Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg 92:984–989
Reuter DA, Felbinger TW, Schmidt C, et al (2002) Stroke volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med 28:392–398
Marx G, Cope T, McCrossan L, et al (2004) Assessing fluid responsiveness by stroke volume variation in mechanically ventilated patients with severe sepsis. Eur J Anaesthesiol 21:132–138
Wiesenack C, Prasser C, Keyl C, Rodig G (2001) Assessment of intrathoracic blood volume as an indicator of cardiac preload: single transpulmonary thermodilution technique versus assessment of pressure preload parameters derived from a pulmonary artery catheter. J Cardiothorac Vasc Anesth 15:584–588
Fernandez-Mondejar E, Rivera-Fernandez R, Garcia-Delgado M, et al (2005) Small increases in extravascular lung water are accurately detected by transpulmonary thermodilution. J Trauma 59:1420–1423
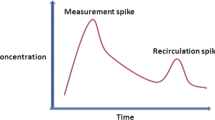
Band DM, Linton RA, O’Brien TK, et al (1997) The shape of indicator dilution curves used for cardiac output measurement in man. J Physiol 498 ( Pt 1):225–229
Pearse RM, Ikram K, Barry J (2004) Equipment review: an appraisal of the LiDCO plus method of measuring cardiac output. Crit Care 8:190–195
Linton R, Band D, O’Brien T, et al (1997) Lithium dilution cardiac output measurement: a comparison with thermodilution. Crit Care Med 25:1796–1800
Linton RA, Jonas MM, Tibby SM, et al (2000) Cardiac output measured by lithium dilution and transpulmonary thermodilution in patients in a paediatric intensive care unit. Intensive Care Med 26:1507–1511
Kurita T, Morita K, Kato S, et al (1997) Comparison of the accuracy of the lithium dilution technique with the thermodilution technique for measurement of cardiac output. Br J Anaesth 79:770–775
Hamilton TT, Huber LM, Jessen ME (2002) PulseCO: a less-invasive method to monitor cardiac output from arterial pressure after cardiac surgery. Ann Thorac Surg 74:S1408–1412
Pittman J, Bar-Yosef S, SumPing J, et al (2005) Continuous cardiac output monitoring with pulse contour analysis: a comparison with lithium indicator dilution cardiac output measurement. Crit Care Med 33:2015–2021
Pearse R, Dawson D, Fawcett J, et al (2005) Early goal-directed therapy after major surgery reduces complications and duration of hospital stay. A randomised, controlled trial [ISRCTN38797445]. Crit Care 9:R687–693
Manecke GR, Jr., Auger WR (2007) Cardiac output determination from the arterial pressure wave: clinical testing of a novel algorithm that does not require calibration. J Cardiothorac Vasc Anesth 21:3–7
Wesseling KH, Weber H, de Wit B (1973) Estimated five component viscoelastic model parameters for human arterial walls. J Biomech 6:13–24
Langewouters GJ, Wesseling KH, Goedhard WJ (1985) The pressure dependent dynamic elasticity of 35 thoracic and 16 abdominal human aortas in vitro described by a five component model. J Biomech 18:613–620
de Waal EE, Kalkman CJ, Rex S, Buhre WF (2007) Validation of a new arterial pulse contourbased cardiac output device. Crit Care Med 35:1904–1909
Sander M, Spies CD, Grubitzsch H, et al (2006) Comparison of uncalibrated arterial waveform analysis in cardiac surgery patients with thermodilution cardiac output measurements. Crit Care 10:R164
Mayer J, Boldt J, Schollhorn T, et al (2007) Semi-invasive monitoring of cardiac output by a new device using arterial pressure waveform analysis: a comparison with intermittent pulmonary artery thermodilution in patients undergoing cardiac surgery. Br J Anaesth 98: 176–182
Sakka SG, Kozieras J, Thuemer O, van Hout N (2007) Measurement of cardiac output: a comparison between transpulmonary thermodilution and uncalibrated pulse contour analysis. Br J Anaesth 99:337–342
Mayer J, Boldt J, Wolf M, Suttner S (2007) Second generation arterial waveform analysis for less Invasive determination of the cardiac output. Anesthesiology 107:A1531
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15:85–91
Breukers R, Sepehrkhouy S, Spiegelenberg S, Groneveld J (2007) Cardiac output measured by a new arterial pressure waveform analysis method without calibration compared with thermodilution after cardiac surgery. J Cardiothorac Vasc Anesth 21:632–635
Prasser C, Trabold B, Schwab A, et al (2007) Evaluation of an improved algorithm for arterial pressure-based cardiac output assessment without external calibration. Intensive Care Med 33:2223–2225
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2008 Springer-Verlag Berlin Heidelberg
About this paper
Cite this paper
Marx, G., Schuerholz, T. (2008). Minimally Invasive Cardiac Output Monitoring: Toy Or Tool?. In: Yearbook of Intensive Care and Emergency Medicine. Yearbook of Intensive Care and Emergency Medicine, vol 2008. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-77290-3_57
Download citation
DOI: https://doi.org/10.1007/978-3-540-77290-3_57
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-77289-7
Online ISBN: 978-3-540-77290-3
eBook Packages: MedicineMedicine (R0)