Abstract
Molecular targeted therapies and immune checkpoint inhibitors have in recent years been transforming the care of many cancer patients. This chapter compares twenty-one appraisals of molecular targeted therapies in non-small-cell lung cancer, comprising six EGFR-TK inhibitors (gefitinib, erlotinib, afatinib, necitumumab, osimertinib and dacomitinib), five ALK inhibitors (crizotinib, ceritinib, alectinib, brigatinib and lorlatinib) and two ROS1 inhibitors (crizotinib and entrectinib), with fifteen appraisals of checkpoint inhibitors used in the treatment of non-small-cell lung cancer comprising the anti-PD-1 agents nivolumab and pembrolizumab, and the anti-PD-L1 agents atezolizumab and durvalumab. Differences with respect to economic evaluation, such as, in terms of the clinical evidence underlying the modelling of cost-effectiveness, and differences observed with respect to life-extending end-of-life status and with respect to inclusion in the Cancer Drugs Fund, are highlighted. The differences observed between the appraisal of the two types of therapy derive from the more limited clinical data and the more restricted application of the targeted medicines. This study of decision making with respect to oncology drugs is likely to be increasingly relevant to a much wider range of medicines, as differential weighting of QALYs and the use of managed access schemes are extended beyond oncology drugs.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Introduction
Two major groups of therapies have in recent years been transforming the care of many cancerpatients, namely molecular targeted therapies and immune checkpoint inhibitors. Molecular targeted therapies interfere with the molecules required for tumour growth and progression (Abramson 2018). Whereas immune checkpoint inhibitors mobilise the body’s immune system to destroy cancer cells. The success of the latter is such that they have rapidly become some of the most widely prescribed anticancer therapies (Robert 2020).
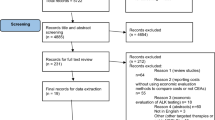
This chapter aims to discuss the cost-effectiveness of such therapies. Rather than undertaking a systematic review of economic evaluations of these therapies, I will restrict my focus to those appraised by the National Institute for Health and Care Excellence (NICE), a public body whose positive recommendations are mandatory for the National Health Service (NHS) in England. This approach has a number of advantages. Firstly, it facilitates comparison of checkpoint inhibitors with molecular targeted therapies because the evidence submission from manufacturers and its subsequent critique by an independent Evidence Review Group focuses on a Reference Case (imposing a degree of uniformity in approach) and is conducted in the context of well-established appraisal methods (NICE 2013). Secondly, all of these assessments of the cost-effectiveness of these health technologies have been undertaken for a common purpose, namely, to determine which treatments will be made available by the NHS in England. Thirdly, the level of detail regarding the clinical effectiveness evidence and the economic modelling choices (and the impact of alternative choices) is much greater than is the case for journal articles.
This chapter is based on experience with respect to the appraisal of therapies for non-small-cell lung cancer because this area offers better opportunities than any other for the comparison of molecular targeted therapies with immune checkpoint inhibitors in terms of the nature of the available data and the methods of economic evaluation employed. The twenty-one appraisals of molecular targeted therapies in non-small-cell lung cancer that have been completed to date comprise six EGFR-TK inhibitors (gefitinib, erlotinib, afatinib, necitumumab, osimertinib and dacomitinib), five ALK inhibitors (crizotinib, ceritinib, alectinib, brigatinib and lorlatinib) and two ROS1 inhibitors (crizotinib and entrectinib). The fifteen appraisals of checkpoint inhibitors used in the treatment of non-small-cell lung cancer comprise the anti-PD-1 agents nivolumab and pembrolizumab, and the anti-PD-L1 agents atezolizumab and durvalumab. As can be seen from Table 1, in the treatment of non-small-cell lung cancer, the first guidance with respect to molecular targeted therapies was issued in 2010, whereas the first guidance with respect to immune checkpoint inhibitors appeared in 2017.
The chapter compares the economic evaluation of molecular targeted therapies and of immune checkpoint inhibitors by reviewing the challenges involved in assessing the cost effectiveness of these new agents. With respect to economic evaluation, the main differences arise from the nature and extent of the available clinical evidence used to model their cost-effectiveness and the number of clinical indications for use. The chapter then goes on to consider the specific arrangements for determining access to oncology medicines, highlighting how these differences, with respect to evidence and proposed use, lead to different experience for the two groups of therapies. Although all oncology medicines in England are subject to the same decision-making arrangements, these arrangements have different implications for checkpoint inhibitors owing primarily to their having many more clinical indications than targeted therapies.
Economic Evaluation of Targeted Therapies and Checkpoint Inhibitors
In this section I review the economic evaluation of checkpoint inhibitors and targeted therapies, with an emphasis on the differences between the two technologies.
The clinical pathways for non-small-lung cancer patients are fairly numerous even when restricting attention to systemic anti-cancer therapy. This is, in part, a result of the advent of molecular targeted therapies making it important to distinguish several distinct patient groups, and because the increasing number of treatments increases the number of lines of treatment available to patients. Starting with the comparators used when estimating cost-effectiveness, there is fairly clear evolution of comparators over time with respect to molecular targeted therapies. For example, with respect to EGFR-TK inhibitors when gefitinib was originally considered as a first line treatment the comparator was platinum doublet therapy, then when erlotinib was considered, gefitinib became the comparator, and for afatinib the comparators were erlotinib and gefitinib, then when dacomitinib and osimertinib were appraised the comparators were afatinib, erlotinib and gefitinib. Similarly, in the case of first line treatment of ALK+ patients, crizotinib was compared to pemetrexed and cisplatin, then ceritinib and alectinib were compared with crizotinib, pemetrexed plus carboplatin/cisplatin, then brigatinib was compared to alectinib, ceritinib and crizotinib.
A similar evolution with respect to the comparators used is not observed in appraisals of immune checkpoint inhibitors. This is partly because sequences of checkpoint inhibitors are not an option and partly because of a peculiarity of NICE appraisal methods, namely when drugs are reviewed following inclusion in the Cancer Drugs Fund “no changes to the scope of the appraisal will be considered” (para. 6.25) (NICE 2018). Thus, when nivolumab was re-appraised for advanced squamous non-small-cell lung cancer after chemotherapy and guidance was published in October 2020 (TA655), docetaxel remained the comparator, despite immunotherapies (atezolizumab and pembrolizumab) now being available for these patients (NICE 2020a).
Most of the appraisals have followed the same general approach to modelling costs and health outcomes. Twenty out of twenty-one appraisals of targeted therapies and fourteen out of fifteen appraisals of checkpoint inhibitors have featured partitioned survival models, the exceptions being TA192 (gefitinib) and TA578 (durvalumab). Partitioned survival models, unlike Markov models which are based on transitions between health states, use survival data directly to determine the time spent in different health states. In the case of cancer appraisals, the area under the overall survival curve is partitioned into time spent progression-free and time spent with progressed disease, using the progression-free survival curve. The two exceptions featured Markov models, gefitinib by virtue of its pre-dating the widespread enthusiasm for partitioned survival modelling (NICE 2010), and durvalumab because the manufacturer’s attempts to implement partitioned survival modelling were thwarted by the extrapolated overall survival and progression-free curves crossing (NICE 2019a, b). Such crossing of curves, which is clearly impossible in practice since you need to be alive to enjoy progression-free survival, can arise when survival curves are fitted independently.
However, there were some differences in how survival was modelled. Cure rate models were never employed in the appraisal of the targeted therapies whereas, they were with checkpoint inhibitors. However, possibly surprisingly, only two of the fifteen appraisals featured formal modelling of cure rate models (atezolizumab in TA520 and durvalumab in TA578). On neither occasion was the committee persuaded by the manufacturer’s analysis. The appraisal committee noted, in the case of atezolizumab, that the model had not been sufficiently justified by the company and the cure rate was not sufficiently supported by the evidence (NICE 2018), and in the case of durvalumab that the PACIFIC trial data “were too immature for a cure model to be robust” (NICE 2019a).
More substantial differences are apparent in the clinical data upon which cost-effectiveness was assessed and, in the methods, used to estimate the relative effectiveness of treatments. The key source of data, upon which the cost-effectiveness modelling for the intervention was based came from randomised controlled trials for all of the checkpoint inhibitors, whereas six of the twenty-one appraisals of targeted therapies were based on non-randomised data (single arm trials plus one randomised dosing study). There is a tendency for the checkpoint inhibitor trials to have larger sample sizes for the intervention, with on average, 303 patients receiving the checkpoint inhibitor as compared to 208 patients receiving the targeted therapies. There being fewer head-to-head trials in the case of targeted therapies and the trials enrolling fewer subjects possibly reflects the targeted nature of the therapies.
It might be expected that these two features would lead to increased reliance on indirect comparisons to establish treatment effects in the case of the targeted therapies. This is not supported by a comparison of the proportion of appraisals featuring such analyses. The proportion of appraisals where indirect comparisons were made by the manufacturers is broadly similar for the checkpoint inhibitors (67%) and targeted therapies (62%). However, the targeted therapies give the appearance of greater use of indirect treatment comparisons than is the case with the checkpoint inhibitors. There are six appraisals involving Matching Adjusted Indirect Comparisons in the case of targeted therapies and none for checkpoint inhibitors.
Population-adjusted indirect comparisons refer to the use of individual patient data to adjust for between-trial differences in the distribution of variables which influence outcome. The merits of direct comparisons in randomised head-to-head trials are well-established. Indirect treatment comparisons generate a range of response. In the Cochrane Handbook for Systematic Reviews of Interventions we are reminded that “Indirect comparisons are not randomized comparisons and cannot be interpreted as such. They are essentially observational findings across trials, and may suffer the biases of observational studies, for example due to confounding.” (Higgins and Green 2011) Whereas Lu and Ades (2004) argue “… to ignore indirect evidence either makes the unwarranted claim that it is irrelevant or breaks the established precept of systematic review that synthesis should embrace all available evidence”, making indirect treatment comparisons required rather than optional. Differing views notwithstanding, few if any would argue for indirect over direct comparisons. Population-adjusted indirect comparisons are an attempt to mitigate some of the limitations of indirect comparisons.
There are two main methods that use individual patient data to adjust for between-trial differences in the distribution of variables that influence outcome: Matching-Adjusted Indirect Comparison (MAIC) and Simulated Treatment Comparison (STC). For no obvious reason, use of the latter approach has been restricted to appraisals of treatments for urothelial carcinoma. Whereas, Matching-Adjusted Indirect Comparisons have been used more widely and have featured in six non-small cell lung cancer appraisals (brigatinib twice, ceritinib, entrectinib, lorlatinib and osimertinib). This can be contrasted with the practice observed in the conduct of the fifteen appraisals of checkpoint inhibitors where MAICs have not featured. The proximate explanation for this marked difference is that all of the checkpoint inhibitor appraisals drew their data primarily from randomised controlled trials, in contrast to the greater reliance placed on non-randomised studies in the appraisals of molecular targeted therapies. In addition, the population for targeted therapies is smaller and trials are also smaller which may make differences in baseline characteristics more substantial than in the case of checkpoint inhibitors.
Matching Adjusted Indirect Comparisons are a relatively new area of activity. They are particularly relevant when a manufacturer has individual patient data from a trial of its own drug but only has access to aggregate data for a drug to which it wishes to compare. They involve reweighting the population in a study where individual patient-level data are available to match more closely the aggregate data from another study. The central idea is that MAIC can allow comparison of trials where there are differences in the baseline characteristics of patients. We can distinguish “anchored” and “unanchored” indirect comparisons. Unanchored indirect comparisons are used where there is a disconnected treatment network or single arm studies. An unanchored MAIC assumes that all effect multipliers and prognostic factors are accounted for. Suppose you have individual data for a trial of A and aggregate data for another trial of B. The MAIC tries to generate the AB effect that would be observed in an A vs. B trial.
For example, in the appraisal of brigatinib for treating ALK-positive advanced non-small cell lung cancer after crizotinib, there was no clinical trial directly comparing brigatinib with the relevant comparator, ceritinib. The manufacturer estimated progression-free survival and overall survival using a hazard ratio from a meta-analysis of two MAICs. In the first, ceritinib data from the single arm ASCEND-2 were matched to the brigatinib arm of ALTA. In the second, the ceritinib arm of ASCEND-5 were also matched to the brigatinib arm of ALTA. The factors adjusted for in the MAICs comprised ECOG performance status, presence of brain metastases, age, crizotinib as last treatment before next TK inhibitor, gender, receipt of any prior chemotherapy, number of prior anti-cancer regimens and smoking history status.
All of the appraisals of checkpoint inhibitors have based their health state utility values on EQ-5D (Rabin and de Charro 2001) data collected in clinical trials. Whereas targeted therapies, while mainly relying on EQ-5D data collected in clinical trials, have also made use of mapping algorithms from QLQ-C30 (Aaronson et al. 1993) to EQ-5D on five occasions, and cancer-specific health state values on three occasions. This probably, in part, reflects changes in the conduct of economic evaluations over time and that several of the targeted appraisals predate consideration of the checkpoint inhibitors.
Arrangements Specific to Decision Making Involving Oncology Medicines
The appraisal by NICE of oncological treatments has differed significantly from the appraisal of non-oncological treatments. Since 2016, NICE has routinely appraised all oncology medicines, whereas this practice has only recently been extended to all medicines. The 2019 Voluntary Scheme for Branded Medicines Pricing and Access agreed that NICE would appraise all new active substances in their first indication (and usually any significant new therapeutic indication). This agreement, between the UK government, NHS England, the Association of the British Pharmaceutical Industry and individual manufacturers, also confirmed that appraisal timelines for non-oncology treatments would in future match those for oncology treatments, reflecting the longer lag in the past between the date of the marketing authorisation and any NICE guidance to the NHS.
There are two other important ways in which decision-making involving oncology therapies is clearly different from that for other medicines. Since January 2009, appraisal committees have been required to value the health benefits accruing to life-extending end-of life treatments more highly than those produced by treatments not qualifying for this status. The two criteria which currently must be met to be a life-extending end-of-life treatment are that, in the absence of the new treatment the patient group would have a short life expectancy, normally less than twenty-four months, and there is sufficient evidence to indicate that the treatment offers an extension to life, normally of at least three months. Note that there is no requirement that the treatment in question be a cancer therapy. However, to date a treatment has been determined to be a life-extending end-of-life treatment on 110 occasions, only one of which was not for advanced cancer. The single exception being nusinersen, a treatment for spinal muscular atrophy. The higher valuation of the health benefits in these cases has been implemented by using a cost-effectiveness threshold of £50,000 per QALY gained, instead of the cost-effectiveness threshold range of £20,000 to £30,000 used explicitly by NICE since 2004.
England has had a Cancer Drugs Fund since 2010 but it has had two distinct incarnations. The original Cancer Drugs Fund was introduced in 2010 as fulfilment of an election promise, that any cancer patient should be allowed any drug licensed in the previous five years, if sought by their doctor, even if NICE had determined that it did not represent good value for money for the NHS. The Cancer Drugs Fund was established by the new coalition government (with interim funding of £60 million, and from 1 April 2011, £200 million per annum) as an additional funding source for cancerdrugs not routinely available through routine commissioning. Its operational management moved to NHS England in 2013. Concern over its financial sustainability led first to more rigorous assessment of candidate medicines, and then to proposals for an entirely new fund. This further instance of special treatment being extended to cancer therapies, offered poor value for the increasing proportion of NHS budget that it absorbed (Aggarwal et al. 2017).
The new Cancer Drugs Fund, launched in England on 1 July 2016, provides a mechanism by which access to some new therapies can be increased by offering appraisal committees an alternative to rejection, when there is an insufficiently compelling case for recommending that they are provided as part of routine clinical practice. If a committee, following its review of the evidence on clinical effectiveness and cost-effectiveness, does not recommend routine commissioning by NHS England, it can consider whether to recommend inclusion in the Cancer Drugs Fund. In making its decision the committee considers the following questions:
-
Is the model structurally robust for decision making?
-
Is there plausible potential to be cost-effective at the offered price?
-
Could further data collection reduce uncertainty?
-
Will ongoing studies provide useful data?
-
Is Cancer Drugs Fund data collection via the Systemic Anti-Cancer Therapy relevant and feasible?
As well as tying inclusion in the Cancer Drugs Fund to the NICE appraisal of the medicine, the 2016 Cancer Drugs Fund addressed the budget sustainability issues of its precursor. First, as highlighted in the questions listed above, a selective approach to entry to the Cancer Drugs Fund is now practiced. Second, while in the fund the drug must be provided at a cost-effective price (a price informed by the committee’s appraisal). Third, there is a budget cap supported by a provision that the Cancer Drugs Fund spend is shared across entrants when the cap is reached.
The first medicine to be made available through the new fund, in October 2016, was osimertinib for treating metastatic EGFR and T790M mutation-positive non-small-cell lung cancer (NICE 2016). The appraisal committee believed the ICER to be between £60,663 and £70,776 per QALY gained. Although, it met the criteria to be regarded as a life-extending end-of-life treatment, these ICERs were too high to recommend that it be routinely commissioned. The greatest area of uncertainty concerned the extrapolation of the overall survival data for patients treated with osimertinib. It was anticipated that this would be reduced over the next two years with follow-up of the AURA-3 trial. The other main uncertainty concerned the generalisability of the AURA-3 trial to English clinical practice. It was anticipated that data collected over the next two years would document treatment patterns and baseline patient characteristics, and in particular, provide more accurate estimates of the duration of treatment. The appraisal committee subsequently met in February 2020, and following review of the additional data, recommended routine commissioning of osimertinib for this indication (NICE 2020b).
There are some clear differences between the non-small-cell lung cancer appraisals of immune checkpoint inhibitors and of molecular targeted therapies with respect to life-extending end-of-life status and entry to the 2016 Cancer Drugs Fund.
If we compare the proportion of the two groups considered to meet the criteria to be assessed as life-extending end-of-life treatments, we find that in thirteen out of fifteen non-small-cell lung cancer appraisals (87 per cent), the checkpoint inhibitor was deemed to meet the criteria to be considered an end-of-life life-extending treatment with respect to at least one comparator. Whereas molecular targeted therapies were similarly considered to be life-extending end-of life treatments in ten out of twenty-one appraisals (48 per cent). There are two potential explanations for this marked difference, one is that checkpoint inhibitors are typically extending life more substantially than the molecular targeted therapies (making it more likely that the extension to life criterion is met). Another potential explanation is that the targeted therapies are being used earlier in the treatment pathway than the checkpoint inhibitors when life expectancy under current treatment is greater (making it less likely that they meet the life expectancy criterion).
Fifty-seven per cent of non-small cell lung cancer appraisals of checkpoint inhibitors, where inclusion in the 2016 Cancer Drugs Fund was an option, were subsequently included in the fund. Whereas only fourteen per cent of appraisals of molecular targeted therapies for non-small cell lung cancer have led to provision within the fund. There are a number of potential explanations for this differential recourse to the 2016 Cancer Drugs Fund. It may be that there is a higher likelihood that uncertainties regarding clinical effectiveness, and ultimately cost-effectiveness, can be satisfactorily reduced by inclusion in the fund in the case of checkpoint inhibitors, as compared to molecular targeted therapies. This might arise because the impact of checkpoint inhibitors, on some patients’ health, is much more long-lived and the uncertainties are consequently greater but amenable to longer follow-up of trial participants.
There may also be an explanation in terms of drug pricing. The health benefits that the average patient can expect from a particular treatment are likely to vary by indication. With uniform pricing across indications there can be some indications where use of the medicine does not offer a favourable balance between the expected costs of treatment and the expected benefits, and others where use of the medicine provides satisfactory value for money. Indication-specific pricing offers the opportunity to provide patients with particular indications access to medicines that they might be denied under uniform pricing. Described thus indication-specific pricing appears something of a boon. It can also be described as price discrimination which transfers surplus from those paying for health care to the firms selling the medicines (Chandra and Garthwaite 2017). NHS England has been reluctant to engage in indication-specific pricing as part of routine commissioning, but the door is not firmly closed. The 2019 Voluntary Scheme on Branded Medicines recognises uniform pricing as the norm but concedes “In cases where uniform pricing would lead to a reduction in total revenue for a medicine overall from the introduction of additional indications, other forms of commercial flexibility may be considered for medicines with a strong value proposition. In these cases, commercial flexibility would only be considered where the level of clinical effectiveness is highly differentiated, but substantial in all indications under consideration” (DHSC 2018, para. 3.36).
The potential relevance of uniform pricing is that the non-small-cell lung cancer molecular targeted therapies are characterised by a lower number of NICE-recommended indications (usually one or two, occasionally three) as compared to checkpoint inhibitors. NICE has issued guidance, for example, on sixteen occasions in the case of pembrolizumab and fifteen times for nivolumab, and many further appraisals are in development. Moreover, pembrolizumab has been appraised in seven clinical areas: colorectal cancer, head and neck cancer, Hodgkin lymphoma, melanoma, non-small-cell lung cancer, renal cell carcinoma and urothelial carcinoma, and nivolumab has been appraised in these seven clinical areas plus oesophageal cancer. This is in marked contrast to the twelve targeted therapies which, with a single exception, only have non-small-cell lung cancer indications. The sole exception, entrectinib, also has an indication for NTRK fusion-positive solid tumours. The potential foregone revenue to the manufacturer from setting a single uniform price would thus be expected to be less in the case of the targeted therapies. While a drug included in the Cancer Drugs Fund will need to be offered at a potentially cost-effective price, since it is not part of routine commissioning the scope for price to vary across indications is much greater. Consequently, manufacturers might have a stronger incentive to seek inclusion of their checkpoint inhibitors in the 2016 Cancer Drugs Fund.
The multiple therapeutic indications for some new drugs were noted in NICE’s 2021 consultation on changes to its appraisal processes, in which they specifically highlighted pembrolizumab, nivolumab, and atezolizumab. They posed the question whether “the current approach to conduct a full technology appraisal for every new indication is proportionate or if an alternative simpler approach to evaluation … may be more appropriate for technologies that are evaluated multiple times” and sought views concerning different approaches (NICE 2021). Thus, NICE’s interest in considering alternative approaches stems primarily from constraints on the organisation’s evaluative capacity, however, as we have seen, multiple indications also raise at least as important issues with respect to the pricing of these therapies.
Conclusions
While this review is based on experience in non-small-cell lung cancer it offers insights regarding the evaluation of targeted therapies and checkpoint inhibitors across oncology. The differences with respect to economic evaluation, such as, in terms of the clinical evidence underlying the modelling of cost-effectiveness, and the differences observed with respect to life-extending end-of-life status and with respect to inclusion in the Cancer Drugs Fund, are not anticipated to be specific to non-small-cell lung cancer but arise from differences between immune checkpoint inhibitors and molecular targeted therapies.
Although it appears that some of the differences between oncology treatments and non-oncology treatments are beginning to reduce, this looks like being achieved by moving appraisal and decision-making with respect to non-oncology drugs closer to that of oncology drugs. An increasing proportion of non-oncology treatments will be subject to appraisal by NICE. Also, the general election at the end of 2019 brought forward a proposal to extend the Cancer Drugs Fund to create a new Innovative Medicines Fund. Additionally, NICE have recently consulted on changes to their methods of appraisal, expressing a clear desire to replace the life-extending end-of-life criteria with a severity criterion (NICE 2020c). While many oncology medicines are still likely to qualify for a more favourable treatment of their health benefits, it is anticipated that they will be joined by a number of non-oncology medicines. Just how many non-oncology medicines and the new severity criteria are yet to be revealed. Thus, the study of the recent past of decision making with respect to oncology drugs is likely to be increasingly relevant to a much wider range of medicines, as differential weighting of QALYs and the use of managed access schemes are extended beyond oncology drugs.
This chapter describes where we are rather than how we got here. There is clearly a suggestion that the differences observed between the appraisal of molecular targeted therapies and that of immune checkpoint inhibitors derives from the more limited clinical data and the more restricted application of the targeted medicines. However, clinical studies are not designed, and indications are neither sought nor granted without human agency.
References
Aaronson, N.K., S. Ahmedzai, B. Bergman, et al. 1993. The European Organisation for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute 85: 365–376.
Abramson R. (2018). Overview of targeted therapies for cancer. My Cancer Genome. https://www.mycancergenome.org/content/molecular-medicine/overview-of-targeted-therapies-for-cancer/.
Aggarwal, A., T. Fojo, C. Chamberlain, C. Davis, and R. Sullivan. 2017. Do patient access schemes for high-cost cancer drugs deliver value to society? Lessons from the NHS Cancer Drugs Fund. Annals of Oncology 28 (8): 1738–1750.
Chandra, A., and C. Garthwaite. 2017. The economics of indication-based drug pricing. New England Journal of Medicine 377 (2): 103–106.
Department of Health & Social Care and Association of the British Pharmaceutical Industry. 2018. The 2019 voluntary scheme for branded medicines pricing and access. https://www.gov.uk/government/publications/voluntary-scheme-for-branded-medicines-pricing-and-access.
Higgins J.P.T., and S. Green (eds.). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Lu, G., and A.E. Ades. 2004. Combination of direct and indirect evidence in mixed treatment comparisons. Statistics in Medicine 23 (20): 3105–3124.
NICE. 2010. Gefitinib for the first-line treatment of locally advanced or metastatic non-small-cell lung cancer (TA192). https://www.nice.org.uk/guidance/ta192.
———. 2013. Guide to the methods of technology appraisal 2013. https://www.nice.org.uk/process/pmg9.
———. 2016. Osimertinib for treating locally advanced or metastatic EGFR T790M mutation-positive non-small-cell lung cancer (TA416).
———. 2018. Guide to the processes of technology appraisal. https://www.nice.org.uk/process/pmg19.
———. 2019a. Durvalumab for treating locally advanced unresectable non-small-cell lung cancer after platinum-based chemoradiation (TA578). https://www.nice.org.uk/guidance/ta578.
———. 2019b. Position statement: consideration of products recommended for use in the Cancer Drugs Fund as comparators, or in a treatment sequence, in the appraisal of a new cancer product. January 2019.
———. 2020a. Nivolumab for advanced squamous non-small-cell lung cancer after chemotherapy (TA655). https://www.nice.org.uk/guidance/ta655.
———. 2020b. Osimertinib for treating EGFR T790M mutation-positive advanced non-small-cell lung cancer (TA653). https://www.nice.org.uk/guidance/ta653.
———. 2020c. The NICE methods of health technology evaluation: the case for change. Published 6 November 2020. https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-technology-appraisal-guidance/changes-to-health-technology-evaluation.
———. 2021. Review of the health technology evaluation processes. Published 4 February 2021.
Rabin, R., and F. de Charro. 2001. EQ-5D: A measure of health status from the EuroQol Group. Annals of Medicine 33 (5): 337–343.
Robert, C. 2020. A decade of immune-checkpoint inhibitors in cancer therapy. Nature Communications 11: 3801. https://doi.org/10.1038/s41467-020-17670-y.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2022 The Author(s)
About this chapter
Cite this chapter
Cairns, J.A. (2022). Assessing the Cost-Effectiveness of Molecular Targeted Therapies and Immune Checkpoint Inhibitors. In: Bremer, A., Strand, R. (eds) Precision Oncology and Cancer Biomarkers. Human Perspectives in Health Sciences and Technology, vol 5. Springer, Cham. https://doi.org/10.1007/978-3-030-92612-0_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-92612-0_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-92611-3
Online ISBN: 978-3-030-92612-0
eBook Packages: Religion and PhilosophyPhilosophy and Religion (R0)