Abstract
Background
The anaplastic lymphoma kinase (ALK) inhibitor treatment landscape is rapidly evolving, providing patients with ALK-positive (+) non-small cell lung cancer (NSCLC) with multiple therapy options, multiple lines of treatments, and prolonged survival. However, these recent treatment advances have resulted in additional increases in treatment costs. The objective of this article is to review the economic evidence of ALK inhibitors in patients with ALK+ NSCLC.
Methods
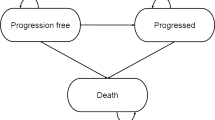
The systematic review was conducted in accordance with the Joanna Briggs Institute (JBI) systematic reviews of economic evaluation. The population included adult patients with locally advanced (stage IIIb/c) or metastatic (stage IV) NSCLC cancer with confirmed ALK fusions. The interventions included the ALK inhibitors alectinib, brigatinib, ceritinib, crizotinib, ensartinib, or lorlatinib. The comparators included the listed ALK inhibitors, chemotherapy, or best supportive care. The review considered cost-effectiveness analysis studies (CEAs) that reported incremental cost-effectiveness ratio in quality-adjusted life years and/or in life years gained. Published literature was searched in Medline (via Ovid) by 4 January 2023, in Embase (via Ovid) by 4 January 2023, in International Pharmaceutical Abstracts (via Ovid) by 4 January 2023, and in Cochrane library (via Wiley) by 11 January 2023. Preliminary screening of titles and abstracts was conducted against the inclusion criteria by two independent researchers followed by a full text of selected citations. Search results are presented in a Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram. Critical appraisal was conducted using the validated Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS) tool as well as the Phillips et al. 2004 appraisal tool to assess the reporting and quality of the economic evaluations. Data were extracted from the final set of articles and presented in a table of characteristics of included studies, an overview of study methods of included studies, and a summarization of outcomes of included studies.
Results
A total of 19 studies met all inclusion criteria. The majority of the studies were in the first-line treatment setting (n = 15). Included CEAs varied in the interventions and comparators being evaluated and were conducted from different country perspectives, limiting their comparability. Outcomes from the included CEAs showed that ALK inhibitors may be considered a cost-effective treatment option for patients with ALK+ NSCLC in the first-line and subsequent lines of treatment setting. However, the probability of cost effectiveness of ALK inhibitors ranged from 46 to 100% and were mostly achieved at willingness-to-pay thresholds of $100,000 USD or higher (> $30,000 or higher in China) in the first-line treatment setting and at thresholds of $50,000 USD or higher in subsequent lines of treatment setting. The number of published full-text CEAs is low and the studies represent a handful of country perspectives. The source of survival data was dependent on data from randomized controlled trials (RCTs). Where RCT data were not available, indirect treatment comparisons or matched adjusted indirect comparisons were performed using efficacy data from different clinical studies. Real world evidence was rarely used for efficacy and costing data inputs.
Conclusion
The findings summarized available evidence on cost effectiveness of ALK inhibitors for the treatment of patients with locally advanced or metastatic ALK+ NSCLC across lines of treatment settings and generated a valuable overview of analytical approaches utilized to support future economic analyses. To help further inform treatment and policy decisions, this review emphasizes the need for comparative cost effectiveness of multiple ALK inhibitors simultaneously using real-world data sources with broad representation of settings.

Similar content being viewed by others
References
Blackadar CB. Historical review of the causes of cancer. World J Clin Oncol. 2016;7(1):54–86. https://doi.org/10.5306/wjco.v7.i1.54.
Sadikovic B, Al-Romaih K, Squire JA, Zielenska M. Cause and consequences of genetic and epigenetic alterations in human cancer. Curr Genom. 2008;9(6):394–408. https://doi.org/10.2174/138920208785699580.
Minamoto T, Mai M, Ronai Z. Environmental factors as regulators and effectors of multistep carcinogenesis. Carcinogenesis. 1999;20(4):519–27. https://doi.org/10.1093/carcin/20.4.519.
Schwaederle M, Kurzrock R. Actionability and precision oncology. Oncoscience. 2015;2(10):779–80.
Cancer.Net. Lung cancer—non-small cell—statistics. June 25, 2012. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/statistics.
Zhu QG, Zhang SM, Ding XX, He B, Zhang HQ. Driver genes in non-small cell lung cancer: characteristics, detection methods, and targeted therapies. Oncotarget. 2017;8(34):57680–92. https://doi.org/10.18632/oncotarget.17016.
Griesinger F, Roeper J, Pöttgen C, Willborn KC, Eberhardt WEE. Brain metastases in alk-positive nsclc—time to adjust current treatment algorithms. Oncotarget. 2018;9(80):35181–94. https://doi.org/10.18632/oncotarget.26073.
Melosky B. Rapidly changing treatment algorithms for metastatic nonsquamous non-small-cell lung cancer. Curr Oncol. 2018;25(Suppl 1):S68-76. https://doi.org/10.3747/co.25.3839.
Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, Liu M, Yuan Y. ALK inhibitors in the treatment of ALK positive NSCLC. Front Oncol. 2019;8:557. https://doi.org/10.3389/fonc.2018.00557.
Barrows SM, Wright K, Copley-Merriman C, Kaye JA, Chioda M, Wiltshire R, Torgersen KM, Masters ET. Systematic review of sequencing of ALK inhibitors in ALK-positive non-small-cell lung cancer. Lung Cancer Targ Ther. 2019;10:11–20. https://doi.org/10.2147/LCTT.S179349.
Migliorino MR, Santo A, Romano G, Cortinovis D, Galetta D, Alabiso O, Cartenì G, et al. Economic burden of patients affected by non-small cell lung cancer (nsclc): the life study. J Cancer Res Clin Oncol. 2017;143(5):783–91. https://doi.org/10.1007/s00432-016-2326-x.
Evans WK, Will BP, Berthelot J-M, Wolfson MC. The economics of lung cancer management in Canada. Lung Cancer. 1996;14(1):19–29. https://doi.org/10.1016/0169-5002(95)00510-2.
Elliott J, Bai Z, Hsieh S-C, Kelly SE, Chen L, Skidmore B, Yousef S, Zheng C, Stewart DJ, Wells GA. ALK inhibitors for non-small cell lung cancer: a systematic review and network meta-analysis. PLoS ONE. 2020;15(2): e0229179. https://doi.org/10.1371/journal.pone.0229179.
Horn L, Wang Z, Wu G, Poddubskaya E, Mok T, Reck M, Wakelee H, et al. Ensartinib vs crizotinib for patients with anaplastic lymphoma kinase-positive non-small cell lung cancer: a randomized clinical trial. JAMA Oncol. 2021;7(11):1617–25. https://doi.org/10.1001/jamaoncol.2021.3523.
NMPA (China) approves ensartinib to treat first line ALK positive NSCLC. https://www.medthority.com/news/2022/3/nmpachina-approves-ensartinib-to-treat-first-line-alk-positive-nsclc.--xcovery-holdings--betta-pharma-/. Accessed 27 Apr 2023.
NCCN. Guidelines detail. https://www.nccn.org/guidelines/guidelines-detail. Accessed 2 Nov 2022.
IASLC. The rising cost of lung cancer therapies: what are the global implications? https://www.iaslc.org/iaslc-news/ilcn/rising-cost-lung-cancer-therapies-what-are-global-implications. Accessed 19 July 2021.
Cancer Care Ontario. “Crizotinib.” https://www.cancercareontario.ca/en/drugformulary/drugs/crizotinib. Accessed 24 Oct 2021.
Cancer Care Ontario. “Ceritinib”. https://www.cancercareontario.ca/en/drugformulary/drugs/ceritinib. Accessed 24 Oct 2021.
Cancer Care Ontario. “Alectinib.” https://www.cancercareontario.ca/en/drugformulary/drugs/alectinib. Accessed 24 Oct 2021.
Aromataris E, Munn Z, Editors. JBI Manual for evidence synthesis. JBI, 2020. https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-01. Accessed 19 July 2021.
Gomersall JS, Jadotte YT, Xue Y, Lockwood S, Riddle D, Preda A. Conducting systematic reviews of economic evaluations. JBI Evid Implement. 2015;13(3):170–8. https://doi.org/10.1097/XEB.0000000000000063.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) explanation and elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25(1):10–31.
Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess. 2004;8(36). https://doi.org/10.3310/hta8360.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 Statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Djalalov S, Beca J, Hoch JS, Krahn M, Tsao M-S, Cutz J-C, Leighl NB. Cost effectiveness of EML4-ALK fusion testing and first-line crizotinib treatment for patients with advanced ALK-positive non-small-cell lung cancer. J Clin Oncol. 2014;32(10):1012–9. https://doi.org/10.1200/JCO.2013.53.1186.
Hurry M, Zhou Z-Y, Zhang J, Zhang C, Fan L, Rebeira M, Xie J. Cost-effectiveness of ceritinib in patients previously treated with crizotinib in anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer in Canada. J Med Econ. 2016;19(10):936–44. https://doi.org/10.1080/13696998.2016.1187151.
Liu M, Zhang L, Huang Q, Li Na, Zheng B, Cai H. Cost-effectiveness analysis of ceritinib and alectinib versus crizotinib in the treatment of anaplastic lymphoma kinase-positive advanced non-small cell lung cancer. Cancer Manag Res. 2019;11(101512700):9195–202. https://doi.org/10.2147/CMAR.S223441.
Carlson JJ, Canestaro W, Ravelo A, Wong W. The cost-effectiveness of alectinib in anaplastic lymphoma kinase-positive (ALK+) advanced NSCLC previously treated with crizotinib. J Med Econ. 2017;20(7):671–7. https://doi.org/10.1080/13696998.2017.1302453.
Zhou Z-Y, Mutebi A, Han S, Bensimon AG, Ricculli ML, Xie J, Dalal A, Culver K. Cost-effectiveness of ceritinib in previously untreated anaplastic lymphoma kinase-positive metastatic non-small cell lung cancer in the United States. J Med Econ. 2018;21(6):577–86. https://doi.org/10.1080/13696998.2018.1443111.
Carlson JJ, Suh K, Orfanos P, Wong W. Cost effectiveness of alectinib vs crizotinib in first-line anaplastic lymphoma kinase-positive advanced non-small-cell lung cancer. Pharmacoeconomics. 2018;36(4):495–504. https://doi.org/10.1007/s40273-018-0625-6.
Lu S, Yu Y, Fu S, Ren H. Cost-effectiveness of ALK testing and first-line crizotinib therapy for non-small-cell lung cancer in China. PLoS ONE. 2018;13(10): e0205827. https://doi.org/10.1371/journal.pone.0205827.
Guan H, Sheng Y, Guo W, Han S, Shi L. Cost-effectiveness of alectinib for patients with untreated ALK-positive non-small cell lung cancer in China. Adv Ther. 2019;36(5):1114–25. https://doi.org/10.1007/s12325-019-00908-7.
Peng Ye, Ma F, Tan C, Wan X, Yi L, Peng L, Zeng X. Model-based economic evaluation of ceritinib and platinum-based chemotherapy as first-line treatments for advanced non-small cell lung cancer in China. Adv Ther. 2019;36(11):3047–58. https://doi.org/10.1007/s12325-019-01103-4.
Li H, Lai L, Bin Wu. Cost effectiveness of ceritinib and alectinib versus crizotinib in first-line anaplastic lymphoma kinase-positive advanced non-small-cell lung cancer. Clin Drug Investig. 2020;40(2):183–9. https://doi.org/10.1007/s40261-019-00880-8.
Savignon M, Monnier R, Tehard B, Roze S. Cost-effectiveness of alectinib compared to crizotinib for the treatment of first-line ALK+ advanced non-small-cell lung cancer in France. PLoS ONE. 2020;15(1): e0226196. https://doi.org/10.1371/journal.pone.0226196.
Huang M, Tian Y, He M, Liu J, Ren L, Gong Y, Peng F, et al. Crizotinib versus chemotherapy: a real-world cost-effectiveness study in China. J Compar Effect Res. 2020;9(2):93–102. https://doi.org/10.2217/cer-2019-0075.
Nilsson FOL, Asanin ST, Masters ET, Iadeluca L, Almond C, Cooper M, Smith S. The cost-effectiveness of lorlatinib versus chemotherapy as a second- or third-line treatment in anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer in Sweden. Pharmacoeconomics. 2021;39(8):941–52. https://doi.org/10.1007/s40273-021-01015-8.
Loong HH, Wong CKH, Leung LKS, Chan CPK, Chang A, Zhou Z-Y, Xie J, Gibbs M. Cost-effectiveness analysis of ceritinib vs. crizotinib in previously untreated anaplastic lymphoma kinase (ALK)-positive non-small cell lung cancer (NSCLC) in Hong Kong. Cost Effect Resour Alloc C/E. 2020;18(1):50. https://doi.org/10.1186/s12962-020-00244-6.
Li S, Li JH, Peng LB, Li YM, Wan XM. Cost-effectiveness of lorlatinib as a first-line therapy for untreated advanced anaplastic lymphoma kinase-positive non-small cell lung cancer. Front Oncol. 2021;11(101568867): 684073. https://doi.org/10.3389/fonc.2021.684073.
Cranmer H, Kearns I, Young M, Humphries MJ, Trueman D. The cost-effectiveness of brigatinib in adult patients with ALK inhibitor-naive ALK-positive non-small cell lung cancer from a US perspective. J Manag Care Spec Pharm. 2022;28(9):970–9. https://doi.org/10.18553/jmcp.2022.28.9.970.
Gourzoulidis G, Zisimopoulou O, Boubouchairopoulou N, Michailidi C, Lowry C, Tzanetakos C, Kourlaba G. Cost-effectiveness analysis of lorlatinib in patients previously treated with anaplastic lymphoma kinase inhibitors for non-small cell lung cancer in Greece. J Health Econ Outcomes Res. 2022;9(1):50–7. https://doi.org/10.36469/jheor.2022.32983.
Luo X, Zhou Z, Zeng X, Peng L, Liu Q. Cost-effectiveness of ensartinib, crizotinib, ceritinib, alectinib, brigatinib and lorlatinib in patients with anaplastic lymphoma kinase-positive non-small cell lung cancer in China. Front Public Health. 2022;10: 985834. https://doi.org/10.3389/fpubh.2022.985834.
Zhang X, Fang P, Guangquan Su, Gui S, Shen A. Cost-effectiveness of ensartinib for patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer in China. J Compar Effect Res. 2022;11(12):871–8. https://doi.org/10.2217/cer-2022-0066.
Roche HL. Randomized, Multicenter, Phase III, Open-label study of alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive advanced non-small cell lung cancer. Clinical trial registration. clinicaltrials.gov, March 1, 2023. https://clinicaltrials.gov/ct2/show/NCT02075840.
Camidge DR, Dziadziuszko R, Peters S, Mok T, Noe J, Nowicka M, Gadgeel SM, et al. Updated efficacy and safety data and impact of the eml4-alk fusion variant on the efficacy of alectinib in untreated ALK-positive advanced non–small cell lung cancer in the global phase III ALEX study. J Thorac Oncol. 2019;14(7):1233–43. https://doi.org/10.1016/j.jtho.2019.03.007.
Roche H-L. Randomized, multicenter, phase III, open-label study of alectinib versus crizotinib in Asian patients with treatment-naive anaplastic lymphoma kinase-positive advanced non-small cell lung cancer. Clinical trial registration. clinicaltrials.gov, September 6, 2019. https://clinicaltrials.gov/ct2/show/NCT02838420.
Zhou C, Kim S-W, Reungwetwattana T, Zhou J, Zhang Y, He J, Yang J-J, et al. Alectinib versus crizotinib in untreated Asian patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer (ALESIA): a randomised phase 3 study. Lancet Respir Med. 2019;7(5):437–46. https://doi.org/10.1016/S2213-2600(19)30053-0.
Roche H-L. Randomized, Multicenter, Phase III, Open-label study of alectinib versus pemetrexed or docetaxel in anaplastic lymphoma kinase-positive advanced non small cell lung cancer patients previously treated with platinum-based chemotherapy and crizotinib. Clinical trial registration. clinicaltrials.gov, October 7, 2019. https://clinicaltrials.gov/ct2/show/NCT02604342.
Signorovitch JE, Sikirica V, Erder MH, Xie J, Lu M, Hodgkins PS, et al. Matching-adjusted indirect comparisons: a new tool for timely comparative effectiveness research. Value Health. 2012;15(6):940–7.
Ariad Pharmaceuticals. “A phase 3 multicenter open-label study of brigatinib (AP26113) versus crizotinib in patients with ALK-positive advanced lung cancer.” Clinical trial registration. Clinicaltrials.gov, July 27, 2021. https://clinicaltrials.gov/ct2/show/NCT02737501.
Camidge, D. Ross, Hye Ryun Kim, Myung-Ju Ahn, James C.H. Yang, Ji-Youn Han, Maximilian J. Hochmair, Ki Hyeong Lee, et al. “Brigatinib versus crizotinib in ALK inhibitor–naive advanced ALK-positive NSCLC: final results of phase 3 ALTA-1L trial.” Journal of Thoracic Oncology 16, no. 12 (December 2021): 2091–2108. https://doi.org/10.1016/j.jtho.2021.07.035.
Novartis Pharmaceuticals. “A phase I, multi-center, open label dose escalation study of LDK378, administered orally in adult patients with tumors characterized by genetic abnormalities in anaplastic lymphoma kinase (ALK).” Clinical trial registration. Clinicaltrials.gov, November 28, 2018. https://clinicaltrials.gov/ct2/show/NCT01283516.
Kim, Dong-Wan, Ranee Mehra, Daniel S W Tan, Enriqueta Felip, Laura Q M Chow, D Ross Camidge, Johan Vansteenkiste, et al. “Intracranial and whole-body response of ceritinib in ALK inhibitor-naïve and previously ALK inhibitor-treated patients with ALK-rearranged non-small-cell lung cancer (NSCLC): updated results from the phase 1, multicentre, open-label ASCEND-1 trial.” The Lancet. Oncology 17, no. 4 (April 2016): 452–63. https://doi.org/10.1016/S1470-2045(15)00614-2.
Novartis Pharmaceuticals. “A phase II, multicenter, single-arm study of oral LDK378 in adult patients with ALK-activated non-small cell lung cancer previously treated with chemotherapy and crizotinib.” Clinical trial registration. Clinicaltrials.gov, May 25, 2017. https://clinicaltrials.gov/ct2/show/NCT01685060.
“Multicenter phase II study of whole-body and intracranial activity with ceritinib in patients with ALK-rearranged non–small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2.” Journal of Clinical Oncology. Accessed November 5, 2021. http://ascopubs.org/doi/pdf/https://doi.org/10.1200/JCO.2015.65.5936.
Novartis Pharmaceuticals. “A Phase III Multicenter, Randomized Study of Oral LDK378 Versus Standard Chemotherapy in Previously Untreated Adult Patients With ALK Rearranged (ALK-Positive), Stage IIIB or IV, Non-Squamous Non-Small Cell Lung Cancer.” Clinical trial registration. clinicaltrials.gov, March 30, 2023. https://clinicaltrials.gov/ct2/show/NCT01828099.
Soria, Jean-Charles, Daniel S W Tan, Rita Chiari, Yi-Long Wu, Luis Paz-Ares, Juergen Wolf, Sarayut L Geater, et al. “First-line ceritinib versus platinum-based chemotherapy in advanced ALK -rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study.” The Lancet 389, no. 10072 (March 2017): 917–29. https://doi.org/10.1016/S0140-6736(17)30123-X.
Novartis Pharmaceuticals. A phase III, multicenter, randomized, open-label study of oral LDK378 versus standard chemotherapy in adult patients with ALK-rearranged (ALK-positive) advanced non-small cell lung cancer who have been treated previously with chemotherapy (platinum doublet) and crizotinib. Clinical trial registration. Clinicaltrials.gov, March 30, 2023. https://clinicaltrials.gov/ct2/show/NCT01828112.
Smith S, Albuquerque de Almeida F, Ines M, Iadeluca L, Cooper M. Matching-adjusted indirect treatment comparisons of the efect of lorlatinib versus chemotherapy on overall survival and progression-free survival for patients with second-line or later anaplastic lymphoma kinase-positive non-small-cell lung cancer. Presented at the International Society for Pharmacoeconomics and Outcomes Research—23rd Annual European Congress. 16–19 November 2020.
Pfizer. Phase 1 safety, pharmacokinetic and pharmacodynamic study of PF-02341066, a MET/HGFR selective tyrosine kinase inhibitor, administered orally to patients with advanced cancer. Clinical trial registration. Clinicaltrials.gov, January 10, 2023. https://clinicaltrials.gov/ct2/show/NCT00585195.
Drilon AE, Camidge DR, Ou S-HI, Clark JW, Socinski MA, Weiss J, Riely GJ, et al. Efficacy and safety of crizotinib in patients (pts) with advanced met exon 14-altered non-small cell lung cancer (NSCLC). J Clin Oncol. 2016;34(15):108–108. https://doi.org/10.1200/JCO.2016.34.15_suppl.108.
Pfizer. Phase 3, randomized, open-label study of the efficacy and safety of crizotinib versus pemetrexed/cisplatin or pemetrexed/carboplatin in previously untreated patients with non-squamous carcinoma of the lung harboring a translocation or inversion event involving the anaplastic lymphoma kinase (Alk) gene locus. Clinical trial registration. Clinicaltrials.gov, September 29, 2017. https://clinicaltrials.gov/ct2/show/NCT01154140.
Solomon, Benjamin J., Tony Mok, Dong-Wan Kim, Yi-Long Wu, Kazuhiko Nakagawa, Tarek Mekhail, Enriqueta Felip, et al. “First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer.” New England Journal of Medicine 371, no. 23 (December 4, 2014): 2167–77. https://doi.org/10.1056/NEJMoa1408440.
Pfizer. Phase 3, randomized, open-label study of the efficacy and safety of crizotinib versus pemetrexed/cisplatin or pemetrexed/carboplatin in previously untreated east Asian patients with non-squamous carcinoma of the lung harboring a translocation or inversion event involving the anaplastic lymphoma kinase (ALK) gene locus. Clinical trial registration. Clinicaltrials.gov, November 16, 2020. https://clinicaltrials.gov/ct2/show/NCT01639001.
Wu Y-L, Lu S, Lu Y, Zhou J, Y-k Shi V, Sriuranpong JCMH, et al. Results of PROFILE 1029, a phase III comparison of first-line crizotinib versus chemotherapy in East Asian patients with ALK-positive advanced non-small cell lung cancer. J Thorac Oncol. 2018;13(10):1539–48. https://doi.org/10.1016/j.jtho.2018.06.012.
Xcovery Holding Company, LLC. Phase 3 randomized study comparing X-396 (ensartinib) to crizotinib in anaplastic lymphoma kinase (ALK) positive non-small cell lung cancer (NSCLC) patients. Clinical trial registration. Clinicaltrials.gov, February 7, 2023. https://clinicaltrials.gov/ct2/show/NCT02767804.
Pfizer. A phase 3, randomized, open-label study of lorlatinib (PF-06463922) monotherapy versus crizotinib monotherapy in the first-line treatment of patients with advanced ALK-positive non-small cell lung cancer. Clinical trial registration. clinicaltrials.gov, May 27, 2022. https://clinicaltrials.gov/ct2/show/NCT03052608.
Shaw AT, Bauer TM, de Marinis F, Felip E, Goto Y, Liu G, Mazieres J, et al. First-line lorlatinib or crizotinib in advanced ALK -positive lung cancer. N Engl J Med. 2020;383(21):2018–29. https://doi.org/10.1056/NEJMoa2027187.
Ma H-c, Liu Y-h, Ding K-l, Liu Y-f, Zhao W-j, Zhu Y-j, Chang X-s, et al. Comparative efficacy and safety of first-line treatments for advanced non-small cell lung cancer with ALK-rearranged: a meta-analysis of clinical trials. BMC Cancer. 2021;21:1278. https://doi.org/10.1186/s12885-021-08977-0.
Roche H-L. An open-label, non-randomized, multicenter phase I/II trial of RO5424802 given orally to non-small cell lung cancer patients who have ALK mutation and who have failed crizotinib treatment. Clinical trial registration. Clinicaltrials.gov, October 31, 2018. https://clinicaltrials.gov/ct2/show/NCT01801111.
Shaw AT, Gandhi L, Gadgeel S, Riely GJ, Cetnar J, West H, RossCamidge D, et al. Phase 2 prospective analysis of alectinib in ALK-positive, crizotinib-resistant non-small-cell lung cancer. Lancet Oncol. 2016;17(2):234–42. https://doi.org/10.1016/S1470-2045(15)00488-X.
Roche H-L. A phase I/II study of the ALK inhibitor CH5424802/RO5424802 in patients with ALK-rearranged non-small cell lung cancer previously treated with crizotinib. Clinical trial registration. Clinicaltrials.gov, July 23, 2018. https://clinicaltrials.gov/ct2/show/NCT01871805.
Sacher AG, Le LW, Lau A, Earle CC, Leighl NB. Real-world chemotherapy treatment patterns in metastatic non–small cell lung cancer: are patients undertreated? Cancer. 2015;121(15):2562–9. https://doi.org/10.1002/cncr.29386.
Chemotherapy in addition to supportive care improves survival in advanced non–small-cell lung cancer: a systematic review and meta-analysis of individual patient data from 16 randomized controlled trials. J Clin Oncol. 2008;26(28):4617–25. https://doi.org/10.1200/JCO.2008.17.7162.
Yu A, Huang E, Abe M, An K, Park S-K, Park C. Cost-effectiveness analyses of targeted therapy and immunotherapy for advanced non-small cell lung cancer in the United States: a systematic review. Expert Rev Pharmacoecon Outcomes Res. 2021;21(3):381–93. https://doi.org/10.1080/14737167.2021.1886928.
Haslam A, Lythgoe MP, Greenstreet Akman E, Prasad V. Characteristics of cost-effectiveness studies for oncology drugs approved in the United States from 2015–2020. JAMA Netw Open. 2021;4(11): e2135123. https://doi.org/10.1001/jamanetworkopen.2021.35123.
Roberts M, Russell LB, Paltiel AD, Chambers M, McEwan P, Krahn M. Conceptualizing a model: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-2. Value Health. 2012;15(62012):804–11. https://doi.org/10.1016/j.jval.2012.06.016.
Novartis Pharmaceuticals. A multi-center, randomized open label study to assess the systemic exposure, efficacy, and safety of 450 mg ceritinib taken with a low-fat meal and 600 mg ceritinib taken with a low-fat meal as compared with that of 750 mg ceritinib taken in the fasted state in adult patients with ALK rearranged (ALK-positive) metastatic non-small cell lung cancer (NSCLC). Clinical trial registration. clinicaltrials.gov, February 7, 2022. https://clinicaltrials.gov/ct2/show/NCT02299505.
Kiefer C, Sturtz S, Bender R. Indirect comparisons and network meta-analyses. Dtsch Arztebl Int. 2015;112(47):803–8. https://doi.org/10.3238/arztebl.2015.0803.
Xie F, Zhou T. Industry sponsorship bias in cost effectiveness analysis: registry based analysis. BMJ. 2022;377: e069573. https://doi.org/10.1136/bmj-2021-069573.
Solomon, Benjamin J., Benjamin Besse, Todd M. Bauer, Enriqueta Felip, Ross A. Soo, D. Ross Camidge, Rita Chiari, et al. “Lorlatinib in Patients with ALK-Positive Non-Small-Cell Lung Cancer: Results from a Global Phase 2 Study.” The Lancet. Oncology 19, no. 12 (December 2018): 1654–67. https://doi.org/10.1016/S1470-2045(18)30649-1https://doi.org/10.1016/S1470-2045(18)30649-1.
Acknowledgements
The authors would like to thank the liaison and education librarian Ms. Glyneva Bradley-Ridout at the University of Toronto for her help and contribution to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
LC is an employee of Hoffmann La-Roche, a pharmaceutical and diagnostics company. This systematic review is being conducted independent of LC’s place of employment. MT received consulting fees from CADTH and Green Shield Canada. NBL has received institutional grant funding from Amgen, Array, AstraZeneca, Bayer, BMS, Eli Lilly, EMD Serono, Guardant Health, Inivata, MSD, Novartis, Pfizer, Roche, and Takeda as well as honoraria for independent CME lectures from Amgen, BMS, EMD Serono, MSD, Novartis, Sanofi Genzyme, and Takeda.
Author contributions
Author 1: Lara Chayab: Conceived and designed the systematic review protocol (objective, research question, PICO, inclusion/exclusion criteria, and methodology); Conducted the systematic review including the search strategy, study selection, assessment of methodological quality, data extraction, analysis, synthesis, and presentation; Drafted the manuscript and revised manuscript on the basis of editor and reviewer comments; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 2: Natalia Konstantelos: Provided substantial intellectual contribution to the systematic review methodology design and conduct; Conducted the systematic review alongside author 1 in the capacity of independent reviewer, including study selection, assessment of methodological quality, and data extraction; Provided critical revisions to the results section of the manuscript including data analysis and presentation as well as to the full manuscript, ensuring overall accuracy, consistency, and rigor; Assisted in addressing reviewer comments and helped revise manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 3: Natasha B. Leighl: Provided substantial intellectual contribution to the conception and design of the systematic review objective, research question, PICO, and inclusion/exclusion criteria from a clinical (medical oncologist) expert perspective; Provided critical revisions to the background, result interpretation, discussion, and relevance/conclusion of the manuscript; Assisted in addressing reviewer comments and provided input to revised manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 4: Mina Tadrous: Provided substantial intellectual contribution to the conception and design of the systematic review protocol (objective, research question, PICO, inclusion/exclusion criteria, and methodology) from a health services and outcomes research expert perspective; Provided critical revisions to the results’ presentation and interpretation, to the discussion, and to the conclusion sections of the manuscript, as well as to the full manuscript, ensuring overall accuracy, consistency, and rigor; Assisted in addressing reviewer comments and provided input to revised manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 5: In supervision, William W.L. Wong: Provided co-leadership (and oversight to) the conception and design of the systematic review protocol and study conduct together with author 1; Conducted the systematic review alongside author 1 and author 2 in the capacity of third reviewer, which required oversight of the study selection, assessment of methodological quality, and data extraction processes; Provided critical and intellectual revisions to the full manuscript, ensuring relevance, rigor, and integrity throughout with special focus on the abstract, methodology description, the results’ analysis, presentation, and interpretation, and the key points for decision makers; Assisted in addressing reviewer comments and helped revise manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting.
Funding
The team received no external funding for this study.
Data availability
The systematic review protocol is available in the International Prospective Register of systematic review, PROSPERO, under registration code CRD42022308680; https://www.crd.york.ac.uk/prospero/. Results of the search strategy are included in this published article (and its supplementary information files).
Code availability
Not applicable.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chayab, L., Konstantelos, N., Leighl, N.B. et al. A Systematic Review of the Cost-Effectiveness Analyses of Anaplastic Lymphoma Kinase (ALK) Inhibitors in Patients with Locally Advanced or Metastatic Non-small Cell Lung Cancer (NSCLC). PharmacoEconomics 41, 945–980 (2023). https://doi.org/10.1007/s40273-023-01279-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01279-2