Abstract
MS is an immune mediated disease of the central nervous system (CNS) characterized by demyelination, axonal damage and neurologic disability. The primary cause of this CNS disease remains elusive. Here we will address our current understanding of the role of viruses as potential environmental triggers for MS. Virus infections can act peripherally (outside the CNS) or within the CNS. The association of viral infections with demyelinating disease, in both animals and humans, will be discussed, as will the potential contributions of peripheral infection with Torque Teno virus, infection outside of and/or within the CNS with Epstein–Barr virus and infection within the CNS with Human Herpesvirus 6 to MS. An experimental animal model, Theiler’s murine encephalomyelitis virus infection of susceptible strains of mice is an example of viral infections of the CNS as a prerequisite for demyelination. Finally, the proposition that multiple virus infections are required, which first prime the immune system and then trigger the disease, as a model where infections outside of the CNS lead to inflammatory changes within the CNS, for the development of a MS-like disease is explored.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Experimental Autoimmune Encephalomyelitis
- Myelin Basic Protein
- Central Nervous System Disease
- Molecular Mimicry
- Canine Distemper Virus
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
MS is the most common inflammatory demyelinating disease of the central nervous system (CNS) in humans. Between 50 and 100 per 100,000 Caucasians (lower in other ethnic groups) are afflicted with this disease, and women are afflicted more than men at a ratio of about 2:1. Onset usually occurs between the ages of 20 and 40 years. Clinical features of MS include alterations in vision, sensory and motor disturbances and cognitive impairment. The clinical course of the disease may be progressive [primary progressive (PP) or secondary progressive (SP)] in nature or include relapses and remissions [relapsing-remitting (RR)]. RR–MS occurs more frequently (85–90%) but with time (10–15 years) can convert to SP–MS. The present general consensus is that MS is a CD4+ T helper (Th) 1-mediated autoimmune disease; however, CD8+ T cells may be involved in the pathogenesis as they are the predominant lymphocyte found in MS lesions. The cells that form myelin in the CNS (oligodendrocytes) are thought to be the main target for attack in MS, and the inflammatory demyelinating lesions characteristic of MS can occur in the optic nerve, brainstem, spinal cord and periventricular white matter. Axonal loss, another important component of MS pathology, occurs from disease onset and correlates, early in disease, with the extent of inflammation within lesions [reviewed in (Bjartmar et al. 2003; Dutta and Trapp 2007)]. The effects of axonal loss may not be apparent for years (clinically silent) due to the compensatory capacity of the CNS. With time, a threshold of axonal loss is reached which surpasses the compensatory capacity of the CNS and irreversible neurological disability develops. Once the irreversible neurological disability develops, it correlates with the degree of axonal degeneration [reviewed in (Bjartmar et al. 2003; Dutta and Trapp 2007)].
The etiology of MS remains elusive despite decades of research. The disease develops in genetically susceptible individuals, but probably, additional environmental triggers are required. A recent large-scale genomewide association study identified alleles of the interleukin (IL)-2 receptor α gene (IL2RA, CD25), alleles of the IL-7 receptor α gene (IL7RA, CD127), both of which are genes related to the regulation of the immune response, and the human leukocyte antigen (HLA)-DR locus as heritable risk factors for MS (Hafler et al. 2007). A more detailed discussion of the genetic contribution to MS is beyond the scope of this chapter and the reader is referred to recent reviews of the subject (Kantarci 2008; McElroy and Oksenberg 2008; Niino et al. 2007).
A role for environmental factors is predicted by the relatively low concordance rate (approximately 25%) for MS in identical twins (Sospedra and Martin 2005), by concordance studies, examining age of the patient at onset, calendar year at onset, presenting symptoms, disability at the time of assessment, disease course, gender and familial recurrence rate, carried out on nontwin sibling pairs (Robertson et al. 1996), as well as by the genome association study, described above, identifying genes related to the regulation of the immune response (Hafler et al. 2007). Environmental factors may include behavioral and lifestyle influences as well as infectious agents (bacterial and viral). For recent discussions of the behavioral and lifestyle influences that may play a role in MS, please see the reviews by Coo and Aronson (Coo and Aronson 2004) and Ascherio and Munger (Ascherio and Munger 2007b). A role for infectious agents is supported by epidemiological studies [(Kurtzke 1993); reviewed in (Ascherio and Munger 2007a; Fujinami 2001b; Libbey and Fujinami 2002, 2003; Oleszak et al. 2004)]. The equatorial region of the earth is a low risk area for MS and the risk increases as you move farther north or south from the equator. Infectious agents present in these areas most likely play a role in this phenomenon. Migration studies suggest that it is exposure to an agent or repeated infections before puberty that either contributes to the risk of developing MS or protects from MS. Migration studies showed that, if migration from an area of high MS risk to an area of low MS risk or vice versa occurred prior to 15 years of age, then the migrant acquired the risk of the area to which they moved; whereas, if migration occurred after 15 years of age, then the migrant maintained the risk of the area from which they moved [(Kurtzke 1993); reviewed in (Ascherio and Munger 2007a; Fujinami 2001b; Libbey and Fujinami 2002, 2003; Oleszak et al. 2004).
One proposed hypothesis for how an infectious agent could explain the epidemiology of MS is the “hygiene hypothesis” [(Leibowitz et al. 1966; Poskanzer et al. 1963a, b, 1966); reviewed in (Ascherio and Munger 2007a)]. This hypothesis proposes that exposure to multiple widespread infectious agents, which are individually relatively harmless, is protective against MS if acquired early in life, whereas exposure at an increasing age increases the risk of MS. This hypothesis could explain the latitude gradient for MS risk if the occurrence of potentially protective infectious agents is high near the equator, thus increasing the likelihood of early childhood infection and protection, and the occurrence of potentially protective infectious agents decreases with distance north and south from the equator, thus decreasing the likelihood of early childhood infection and protection and effectively increasing the likelihood of exposure later in life. This hypothesis could also explain how migration in childhood results in acquiring the risk of the area to which the migrant moves. Migration at a young age, from an area of high risk to an area of low risk, provides the opportunity for infection with potentially protective agents present in the low risk area, but lacking in the high risk area, while still in childhood. Migration at a young age, from an area of low risk to an area of high risk, would deprive the migrant of infection with potentially protective agents present in the low risk area, but lacking in the high risk area, while still in childhood, thus effectively increasing the likelihood of exposure later in life. This hypothesis could also explain how migration in late adolescence and adulthood results in maintaining the risk of the area from which the migrant moves. Adult migrants from low risk area would be protected by their plethora of childhood infections and thus would maintain their low risk, while adult migrants from high risk areas, who lack protective childhood infections, would maintain their high risk upon migration later in life to a low risk area where the occurrence of infectious agents is high. MS, according to this hypothesis, is an immune-mediated reaction triggered in response to multiple infections, such that there is no one specific etiologic agent, in susceptible individuals. It is unlikely that all infectious agents equally predispose to MS [reviewed in (Ascherio and Munger 2007a)].
Viruses have long been thought to play a role in the etiology and pathogenesis of MS. Studies with isolated populations demonstrating that populations which had no reported cases of MS experienced epidemics of MS after contact with North Americans or Europeans is one point in favor of viral involvement (Kurtzke 1993, 1997; Kurtzke and Heltberg 2001). A second point in favor of viral involvement is the finding that CD8+ T cells, which function to clear viral infections, dominate the cellular infiltrate in active MS lesions (Babbe et al. 2000). As a third point, exacerbations of MS can be correlated with viral infections (Álvarez-Lafuente et al. 2006; Andersen et al. 1993; Berti et al. 2002; Buljevac et al. 2002; Christensen 2007; Correale et al. 2006; De Keyser et al. 1998; Edwards et al. 1998; Gilden 2002; Granieri et al. 2001; Kriesel et al. 2004; Kriesel and Sibley 2005; Marrie et al. 2000; Metz et al. 1998; Panitch 1994; Sibley et al. 1985; Sospedra and Martin 2006; Wandinger et al. 2000). However, to date, no immunization or vaccination has ever been demonstrated to induce exacerbations in MS [(Rutschmann et al. 2002); reviewed in (Fujinami 2001a)]. A fourth point in favor of viral involvement is the finding that antibodies against various viruses and/or the viruses themselves have been directly isolated from MS patients. The list includes such diverse viruses as rabies virus, herpes simplex virus (types 1 and 2), parainfluenza virus (type 1), measles virus, coronavirus, human T-cell lymphotrophic virus (type 1), and human herpesvirus 6 (HHV-6) [reviewed in (Johnson 1998; Libbey and Fujinami 2003)]. It should be noted that viruses most commonly associated with MS are viruses that replicate extensively within the CNS (von Herrath et al. 2003); however, no one single virus has ever been unequivocally determined to be the causative agent of MS.
Viral infections, either within the CNS or in the periphery, could induce the autoimmune reactions that result in CNS inflammatory disease through either of the two mechanisms: molecular mimicry and/or bystander activation. The two mechanisms are not mutually exclusive. Molecular mimicry occurs when viral antigens have either sequential or structural similarities to self-antigens [reviewed in (Fujinami 1996,1998, 2000, 2001b; Fujinami et al. 2006; Libbey et al. 2007; McCoy et al. 2006; Peterson and Fujinami 2006; Sospedra and Martin 2005; von Herrath et al. 2003; Whitton and Fujinami 1999)]. Individual viruses may harbor molecular mimics to different CNS antigens and these different mimicries may be mediated through HLA class I- or class II-restricted T cells or antibodies [reviewed in (Fujinami et al. 2006; Libbey et al. 2007; McCoy et al. 2006)]. Therefore, the possibility of multiple mimics and multiple mimicry pathways could explain the inability to isolate one single causative agent of MS and could explain the phenotypic diversity of the disease, respectively. Viruses that encode molecular mimics could induce autoimmunity through either direct infection of the CNS or by peripheral infection.
Bystander activation is the nonspecific activation of autoreactive cells due to inflammatory events caused by infection [reviewed in (Fujinami et al. 2006; McCoy et al. 2006; Sospedra and Martin 2005; von Herrath et al. 2003; Whitton and Fujinami 1999)]. T cell receptor (TCR)-independent bystander activation of autoreactive T cells can occur through the production of inflammatory cytokines, the presence of superantigens or the recognition of molecular patterns by Toll-like receptors, and thus does not require direct viral infection of the CNS. TCR-dependent bystander activation of autoreactive T cells depends on the unveiling of host antigens as a result of direct viral tissue damage, followed by the presentation of host antigens by antigen-presenting cells in conjunction with an adjuvant effect of the infectious agent, which ultimately results in epitope spreading [reviewed in (Sospedra and Martin 2005; von Herrath et al. 2003)].
2 Viral Association with Demyelination
Studies using transgenic mice support the hypothesis that exposure to infectious agents (bacterial and viral) can trigger demyelination [(Goverman et al. 1993); reviewed in (Sospedra and Martin 2005)]. Transgenic mice were constructed that expressed genes encoding a rearranged TCR specific for an encephalitogenic myelin basic protein (MBP) peptide, MBP1–11, in a mouse strain that is genetically susceptible to experimental autoimmune encephalomyelitis (EAE) (Goverman et al. 1993). EAE is a nonviral, autoimmune animal model for MS in which demyelinating disease is induced by the injection of whole protein or encephalitogenic peptides from CNS antigens in adjuvant, or by the adoptive transfer of CNS antigen-sensitized lymphocytes [reviewed in (Tsunoda and Fujinami 1996)]. These mice were found to develop spontaneous demyelination in the white matter of the spinal cord when housed in nonpathogen-free conditions, but remained disease free when housed in sterile, pathogen-free conditions (Goverman et al. 1993). Thus, environmental factors such as viral or bacterial infections may initiate the autoimmune response in these mice, possibly through molecular mimicry, bystander activation or damage to the blood–brain barrier which would allow access of the CNS-specific T cells to the target organ (Goverman et al. 1993).
From studies with experimental animals, certain viral infections are known to cause demyelination [reviewed in (Libbey and Fujinami 2003)]. In some cases the virally-induced demyelination closely resembles MS lesions in humans. Canine distemper virus (CDV) causes a multifocal demyelinating disease in dogs [reviewed in (Vandevelde and Zurbriggen 2005)]. Demyelination occurs at a very high frequency upon CDV infection and the demyelinating lesions generally occur within the white matter of the cerebellum, the periventricular white matter, the optic pathways and the spinal cord; all sites commonly affected in MS. The initial acute demyelinating lesions are associated with viral replication within glial cells of the white matter with extensive infection of astrocytes and restricted infection (viral transcription without translation) of oligodendrocytes, resulting in a dramatic impairment of myelin metabolism. Progression of the chronic demyelinating lesions may be due to both the inflammatory immune reaction, in which the antiviral immune response destroys oligodendrocytes by means of a bystander mechanism, and the persistence of the virus (noncytolytic) in white matter areas outside of the lesions [reviewed in (Vandevelde and Zurbriggen 2005)]. The induction of demyelination in mice can be accomplished with viruses from such diverse viral families as Coronaviridae, Picornaviridae, Rhabdoviridae, and Togaviridae [reviewed in (Libbey and Fujinami 2003)]. Various mechanisms of demyelination, which are not mutually exclusive, include: the direct lysis of infected oligodendrocytes by the virus; direct lysis of infected oligodendrocytes by the immune response; lysis of uninfected oligodendrocytes by an autoimmune response triggered by the virus; and lysis of oligodendrocytes and other cells by a nonspecific bystander immune response in the vicinity of the viral infection. Viral-induced demyelination can vary in its presentation from small focal areas to large plaques. Some similarities between MS and these viral-induced demyelinating diseases in mice include similarities in neuropathology, similarities in disease course which can be either progressive or RR and the role that genetic susceptibility plays in the development of the disease [reviewed in (Libbey and Fujinami 2003)].
Certain viral infections of humans are also known to cause demyelinating disease [reviewed in (Asher 1991; Evans et al. 1991; Sospedra and Martin 2005; Whitley and Schlitt 1991)]. These include the human polyomavirus JC, which causes progressive multifocal leukoencephalopathy (in immunosuppressed subjects); measles virus, which causes postinfectious encephalomyelitis (in approximately 1 in 1,000 cases of acute measles virus infection) and subacute sclerosing panencephalitis (in approximately 8.5 in 1 million cases of acute measles virus infection); herpes simplex virus, which causes encephalitis; and human immunodeficiency virus (HIV), which causes HIV encephalopathy [(Fujinami 2001b); reviewed in (Asher 1991; Evans et al. 1991; Sospedra and Martin 2005; Whitley and Schlitt 1991)].
3 Torque Teno Virus and MS
Torque Teno virus (TTV) is a ubiquitous, nonenveloped, nonpathogenic, small, DNA (single-stranded antisense) virus that only encodes 4–5 gene sequences (Simmonds 2002). TTV is unique in that infection of a wide range of tissues is characterized by a persistent viremia. Bone marrow, lung and lymphoid tissue harbor the highest viral loads. TTV has also been found to have high genetic diversity, with more than 28 distinct genotypes, and multiple genotypes may infect an individual at any one time (Simmonds 2002).
In the context of MS, an early study was unable to detect the presence of TTV DNA in the cerebrospinal fluid (CSF) of MS patients although the serum was shown to be positive for the virus (Maggi et al. 2001). This indicates that the CNS does not represent a common site of TTV replication and persistence and that the virus does not easily permeate an intact blood–brain barrier (Maggi et al. 2001). However, despite this finding, TTV has been implicated in the pathogenesis of MS by another study that isolated CD4+ T cell clones, which were clonally expanded in vivo in the CSF during disease exacerbation in an RR–MS patient, that were found to be specific for the conserved arginine-rich region (74 amino acids) of TTV (Sospedra et al. 2005). This arginine-rich domain was found to be evolutionarily conserved among common viruses, prokaryotes and eukaryotes as part of DNA-binding regions, nuclear localization signals and other functional sequences. The T cell clones could have been activated in the periphery, perhaps in response to TTV, before migrating to the CSF, which would explain the findings of Maggi et al (Maggi et al. 2001). Thus, it has been suggested that repeated infections with common viruses, such as TTV, could induce the expansion of T cells specific for conserved protein domains. This cross-reactivity (molecular mimicry) between pathogens and autoantigens could ultimately lead to the initiation of autoimmune disease (MS) in genetically susceptible individuals (Sospedra et al. 2005). However, although an association between TTV infection and MS has been suggested, this study did not determine whether the initial activator of these T cells was TTV or some autoantigen; it may be that TTV does not trigger MS, but may play a role in perpetuating an already existing autoimmune reaction.
4 Epstein–Barr Virus and MS
Herpes viruses, to include Epstein–Barr virus (EBV), are ubiquitous, enveloped, large DNA (double-stranded) viruses that commonly produce latent, recurrent infections [reviewed in (Christensen 2007)]. EBV is a lymphotropic γ-herpesvirus for which reactivation of latent infections has been correlated with exacerbations of MS [(Wandinger et al. 2000); reviewed in (Christensen 2007)], though this finding remains controversial as other studies have been unable to find an association between EBV reactivation and exacerbations in RR–MS (Buljevac et al. 2005; Torkildsen et al. 2008). EBV seroprevalence is 90%; this seroprevalence increases to 100% in adults with MS [(Ascherio and Munch 2000); reviewed in (Pender and Greer 2007; Sospedra and Martin 2005)]. The EBV seroprevalence in children with MS (disease onset before age 16) approaches 100% and this is in comparison to a seroprevalence of only 72% in age-matched controls [(Pohl et al. 2006); reviewed in (Pender and Greer 2007)]. This is contradictory to the hygiene hypothesis that states that early infection is protective; in this case, seronegative individuals, at any age, have a very low risk of developing MS [reviewed in (Ascherio and Munger 2007a).
MS patients often have had infectious mononucleosis, for which EBV is the known etiologic agent. Primary infection with EBV, resulting in infectious mononucleosis, in adolescence or young adulthood has been correlated with an increased risk (more than twofold) of developing MS [(Thacker et al. 2006); reviewed in (Pender and Greer 2007)].
An increased humoral immune response to EBV has been found in MS patients. In examining the specificity of the oligoclonal immunoglobulin (Ig) bands (produced by intrathecal Ig synthesis) commonly observed in the CSF of MS patients, antibodies specific for two EBV proteins, EBV nuclear antigen (EBNA)-1 and BRRF2, were reported to be significantly higher in the CSF and serum of MS patients compared to controls, and these two proteins were specifically bound by the oligoclonal CSF IgG from MS patients [(Cepok et al. 2005); reviewed in (Pender and Greer 2007)]. In order to differentiate between the increased immune responsiveness to EBV seen in MS patients as being a cause or just an effect of MS, a large prospective study was performed to determine whether antibodies to EBV are elevated before the onset of MS (Levin et al. 2005). It was determined that there is an age-dependent relationship between EBV infection and the development of MS in that, prior to MS onset, serum levels of IgG specific for the EBNA complex, which were equivalent for subjects who developed MS and controls prior to age 20, were two- to threefold higher (statistically significant) in subjects who developed MS compared to controls at age ≥25 years [(Levin et al. 2005); reviewed in (Pender and Greer 2007)]. This age related increase in EBV-specific IgG could be due to alteration of the immune response to EBV by infection with other microorganisms, infection with a different strain of EBV or the development of the autoimmune reaction that leads to MS (Ascherio and Munger 2007a).
An increased cell-mediated immune response specific for EBV has also been demonstrated in MS patients. CD4+ memory T cells with specificity for the C-terminal domain of EBNA-1 were increased in frequency and had increased proliferative capacity and enhanced interferon (IFN)-γ production, without a concomitant increase in viral loads, when isolated from the peripheral blood mononuclear cells (PBMC) of MS patients, compared to healthy EBV carriers as controls (Lunemann et al. 2006). The increased frequency and reactivity of these T cells did not correlate with the extent of clinical disability or disease duration. In addition, the enhanced T cell response was associated with a broadened epitope recognition pattern, rather than being focused on a distinct immunodominant region, in MS patients (Lunemann et al. 2006). Thus, studies of both the humoral immune response and the cell-mediated immune response suggest that there may be a distinct role for EBNA-1-specific immune responses in MS.
In addition to the above evidence for an increased EBV-specific humoral and cell-mediated immune response in MS patients, direct evidence of EBV infection in postmortem brain specimens from MS patients has been demonstrated (Serafini et al. 2007). EBV was found to persist and reactivate in ectopic B cell follicles forming in the cerebral meninges. This abnormal accumulation of EBV-infected B cells/plasma cells in the brain was found to be a common feature of MS which was not linked to disease course, gender, age at onset, disease duration or immunosuppressive therapy. Also, this accumulation of EBV-infected B cells/plasma cells in the brain was found to be specific to MS and not just a general occurrence driven by inflammation. At sites of EBV-infected B cell/plasma cell accumulation, CD8+ T cell infiltration and activation with cytotoxicity towards EBV-infected B cells/plasma cells were found suggesting that an antiviral immune response occurs in the MS brain (Serafini et al. 2007).
EBV could act as a trigger for MS in genetically susceptible individuals through its ability to latently infect memory B cells [reviewed in (Lunemann et al. 2007; Lunemann and Munz 2007; Pender and Greer 2007)]. EBV-infected B cells, which could include CNS-reactive B cells, would not only produce pathogenic autoantibodies, but could also localize to the CNS where they could act as antigen-presenting cells (APC). These EBV-infected APC could present CNS antigens to CD4+ T cells, which have been activated by common systemic infections in the periphery, and which may be cross-reactive for CNS antigens, and which may be reactivated by the APC as they traffic through the CNS, thus promoting the survival of CNS-reactive T cells within the CNS. The surviving CNS-reactive T cells could then organize an immune attack on the CNS [reviewed in (Pender and Greer 2007)]. Additionally, reactivation of a latent EBV infection, either in the CNS or in the periphery, would activate EBV-reactive CD4+ T cells, some of which, isolated from the CSF of MS patients, have been shown to cross-react with the CNS protein, MBP (molecular mimicry) (Holmoy et al. 2004). These resultant myelin-specific CD4+ T cells could be the mediators of MS in genetically susceptible individuals.
All of the associations, between EBV infection and MS, described above, suggest that EBV may be the etiologic agent for MS. Nevertheless, infection with EBV cannot explain the decline in risk observed among subjects who migrate from an area of high MS risk to an area of low MS risk in childhood (Ascherio and Munger 2007a). In order to explain this decline in risk, either other factors contribute to determine the risk or modify the immune response to EBV infection, or EBV strains in the low risk areas are less prone to causing MS.
5 HHV-6 and MS
HHV-6 is a lymphotropic and neurotropic β-herpesvirus whose seroprevalence is > 80% by the age of 2 years, thus making it impossible to assess the risk of MS in seronegative individuals. There are two distinct subtypes of HHV-6: HHV-6A and HHV-6B [reviewed in (Christensen 2007; Fotheringham and Jacobson 2005)]. Early reports failed to distinguish between the two subtypes. A recent report distinguishing antibodies specific for HHV-6A from antibodies specific for HHV-6B has demonstrated that the seroprevalence to HHV-6A (100%) is significantly higher in MS patients compared to controls (69.2%), while no difference was found for the seroprevalence to HHV-6B (Virtanen et al. 2007).
In comparing MS brains to control brains, it was found that HHV-6 genome was present in both while HHV-6 antigen was only detected in MS brains, specifically in oligodendrocytes in MS lessions [(Challoner et al. 1995); reviewed in (Ascherio and Munger 2007a; Christensen 2007; Fotheringham and Jacobson 2005; Sospedra and Martin 2005)]. The detection of HHV-6 genome in the absence of viral antigen is suggestive of a latent infection in controls, while the presence of HHV-6 genome and viral antigen in MS brains suggests an active infection [reviewed in (Fotheringham and Jacobson 2005)].
In studies examining blood and CSF, HHV-6 viral DNA and HHV-6 specific antibodies have been detected in the serum and CSF of MS patients [reviewed in (Ascherio and Munger 2007a; Christensen 2007; Fotheringham and Jacobson 2005)]. Recently, a correlation has been made between exacerbations of RR–MS and increased levels of HHV-6 DNA in the serum and HHV-6A RNA and DNA in the PBMC [(Álvarez-Lafuente et al. 2004); reviewed in (Christensen 2007; Fotheringham and Jacobson 2005)]. In comparing RR–MS to SP–MS, it has been reported that HHV-6 DNA (in DNA extracted from PBMC and in DNA extracted from serum) and transcripts of HHV-6 genes (in mRNA extracted from PBMC) can be found significantly more often in (1) RR–MS patients than in SP–MS patients, and (2) in RR–MS patients experiencing a relapse than in SP–MS patients (Álvarez-Lafuente et al. 2007). No significant differences were found for viral load of HHV-6 in the positive samples or for the distribution of the HHV-6B subtype (in DNA extracted from PBMC), and only HHV-6A was found in the positive serum samples. These results suggest that HHV-6A may contribute to exacerbations of RR–MS, but not to the pathogenesis of SP–MS (Álvarez-Lafuente et al. 2007).
Other studies of serum and CSF have shown that levels of the soluble form of the cellular receptor for HHV-6 (both HHV-6A and HHV-6B), CD46, a complement regulatory protein, are increased in serum and CSF in MS subjects. Serum levels of soluble CD46 were significantly increased in MS patients who were shown to be positive for HHV-6 DNA in their serum [(Soldan et al. 2001); reviewed in (Christensen 2007; Fotheringham and Jacobson 2005)]. However, no correlation was found between the levels of soluble CD46 in the serum and the extent of clinical disability, disease duration or the number of gadolinium-enhancing lesions as measured by magnetic resonance imaging (Soldan et al. 2001).
Finally, oligoclonal Ig bands, common in MS CSF and indicative of intrathecal antibody production, specific for HHV-6 (subtype not specified) have been detected in 20% of MS patients [(Derfuss et al. 2005); reviewed in (Christensen 2007)]. This result has been confirmed and enhanced by the narrowing of the specificity of the intrathecal antibodies to HHV-6A (Virtanen et al. 2007).
HHV-6 could act as a trigger for MS in genetically susceptible individuals through either molecular mimicry, as demonstrated by the cross-reaction of HHV-6 reactive CD4+ T cells, isolated from the PBMC of MS patients, with MBP [(Cirone et al. 2002; Tejada-Simon et al. 2003); reviewed in (Fotheringham and Jacobson 2005; Libbey et al. 2007)], or through excessive complement activation [reviewed in (Fotheringham and Jacobson 2005)]. CD46 is a constitutively express soluble and membrane-bound protein that normally functions to inactivate C3b and C4b complement products, thus protecting healthy cells from lysis by autologous complement. CD46 has several isoforms, and activation of the CD46 isoform dominant in brain causes an increase in CD8+ T cell cytotoxicity, a decrease in CD4+ T cell proliferation and a decrease in IL-10 and IFN-γ production by CD4+ T cells [reviewed in (Fotheringham and Jacobson 2005)]. Increased levels of soluble CD46 in MS patients may be an indication of activation of the complement system (Soldan et al. 2001). Engagement of CD46 by HHV-6 may result in increased activation of the complement cascade on autologous cells through downregulation of the receptor. The resulting complement-mediated tissue destruction may play a role in triggering MS (Soldan et al. 2001).
Thus, as with EBV, an association between HHV-6 infection and MS has been suggested, however, infection with HHV-6 alone cannot explain the epidemiological aspects, including the migration data, of MS. With respect to HHV-6, and also TTV, although a virus that is ubiquitous cannot be intrinsically primarily pathogenic, it cannot be ruled out that certain subtypes/genotypes may be specifically associated with certain diseases (Simmonds 2002). Finally, there is some evidence for an increased frequency of reactivation of latent HHV-6 in subjects with MS compared to controls; however, this may just be a consequence, not a cause, of MS [reviewed in (Ascherio and Munger 2007a)].
6 Basic Animal Model: Viral Persistence Within the CNS
All three human viruses discussed above, TTV, EBV and HHV-6, persist either as an active infection (TTV) or as latent infections that can be reactivated (EBV and HHV-6). These viruses persist either within the CNS (EBV and HHV-6) or in the periphery (TTV and EBV). An animal model of MS that has the characteristic of viral persistence within the CNS is Theiler’s murine encephalomyelitis virus (TMEV) infection of mice.
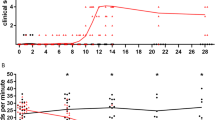
TMEV is a naturally occurring enteric pathogen of the family Picornaviridae [reviewed in (Libbey and Fujinami 2003; Oleszak et al. 2004)]. TMEV is a nonenveloped, positive sense, single-stranded RNA virus. The ability of TMEV to cause disease and the disease characteristics are dependent on the age, sex and strain of the mouse [for a review of the genetics of TMEV infection, please see (Brahic et al. 2005] and the dose and strain of the virus. TMEV has been divided into two subgroups depending on neurovirulence. The more neurovirulent of the two, the GDVII subgroup, containing the GDVII and FA strains, causes an acute fatal polioencephalomyelitis. The less neurovirulent of the two, the Theiler’s Original (TO) subgroup, containing the DA, TO, WW and BeAn strains, causes acute encephalomyelitis followed by CNS demyelination associated with viral persistence in susceptible mouse strains (SJL/J). Acute encephalomyelitis is associated with viral replication within the gray matter of the CNS. Resistant mouse strains (C57BL/6) clear the virus following the acute disease. The persistence of the virus within the CNS of susceptible strains of mice results in demyelination of the white matter of the CNS with features similar to what is observed in MS in humans [reviewed in (Oleszak et al. 2004)]. Although in the past axons were thought to be preserved or damaged secondarily to demyelination, studies by our group have shown that axonal damage can be detected as early as 1 week after infection with the DA strain of TMEV, long before demyelination is apparent (at 4 weeks after infection), the extent of axonal damage increased with time and the distribution of injured axons corresponded to regions where demyelination developed during the chronic phase (Tsunoda et al. 2003; Tsunoda and Fujinami 2002). Further studies demonstrated that induction of axonal degeneration, through injection of a toxic lectin, could target inflammatory demyelinating lesions to sites of the CNS that are normally unaffected by TMEV-induced demyelination (posterior funiculus of the spinal cord), thus suggesting that axonal damage plays a role in recruiting inflammatory cells and targeting demyelinating lesions to specific sites of the CNS (Tsunoda et al. 2007b). Clinically, the TMEV-infected mice with CNS demyelination display symptoms of extremity weakness, spasticity, incontinence and spastic paralysis that are similar to symptoms observed in MS in humans [reviewed in (Libbey and Fujinami 2003; Oleszak et al. 2004)].
In the TMEV model of MS, molecular mimicry between foreign and self epitopes (Olson et al. 2001) and epitope spreading (the end result of bystander activation) from viral to myelin antigens (Miller et al. 1997) are important for the initiation and progression, respectively, of the CD4+ T cell-mediated autoimmune demyelinating disease [reviewed in (Oleszak et al. 2004)]. Olson et al (Olson et al. 2001) were able to directly demonstrate that molecular mimicry could initiate virus-induced demyelination. This was accomplished through the insertion of native and mimic sequences of the encephalitogenic myelin proteolipid protein (PLP) epitope, PLP139–151, into a nonpathogenic, nonpersistent TMEV variant. Intracerebral infection of SJL/J mice with recombinant virus variants carrying the native and mimic sequences resulted in an early-onset demyelinating disease course characterized by the presence of CD4+ Th1 cells specific both for the immunodominant viral epitope, VP270–86, and for the immunodominant PLP epitope, PLP139–151. This held true even for the mimic sequence, derived from the protease IV protein of Haemophilus influenza, which only shared 6 out of 13 amino acids with PLP139–151. It was also demonstrated that the recombinant virus variants carrying the native and mimic sequences were able to persist in the CNS subsequent to intracerebral infection. In contrast, intravenous, subcutaneous and intraperitoneal infection of SJL/J mice with the virus variant carrying the native sequence also resulted in early-onset of the disease course, suggesting that sites distant from the CNS can be the initial sites of infection and that the mimic-encoding virus may not need to infect the target organ, the CNS in this case, in order to induce the autoimmune disease. One factor that may be important in determining whether or not a viral infection, by a virus carrying a self mimic epitope, triggers an autoimmune disease is the primary host cell type infected (Olson et al. 2001). Miller et al. (Miller et al. 1997) were able to demonstrate that epitope spreading could play a major role in the progression of virus-induced demyelination. Through kinetic and functional studies, they showed that demyelination in TMEV-infected mice is initiated by CD4+ T cells with specificity for the virus followed by de novo priming, through the secondary release of sequestered autoantigens, of self-reactive T cells specific for multiple myelin epitopes [PLP139–151, PLP56–70, PLP178–191 and myelin oligodendrocyte glycoprotein (MOG)92–106] which arise in an ordered progression starting 3–4 weeks after the onset of disease. It is important to note that persistence of the virus within the CNS is required for the development of this CNS autoimmunity (Miller et al. 1997). These two mechanisms: molecular mimicry and epitope spreading resulting from bystander activation, most likely function in concert within a TMEV-infected mouse to initiate and perpetuate virus-induced demyelination.
The viral capsid of TMEV plays a major role in persistence and persistent virus can be found in oligodendrocytes, astrocytes and microglia/macrophages [reviewed in (Oleszak et al. 2004)]. Viral persistence, though maybe not sufficient for the development of the demyelinating disease as viral persistence can be demonstrated without the development of the demyelinating disease (Oleszak et al. 1988; Patick et al. 1990), is a prerequisite to developing the chronic demyelinating disease and the extent to which the virus persists is directly proportional to the extent of demyelination and clinical disease.
7 Prime/Challenge Model: Acute Peripheral Infection
Multiple virus infections may be required for the development of MS, as proposed by the hygiene hypothesis (above). However, more specifically, multiple virus infections may interact in such a way that the initial infection may act to prime the immune response, and a subsequent challenge infection with the same or related virus or some other nonspecific immunologic stimulus may trigger the disease. Also, this prime/challenge model allows for the possibility that the initial infection could protect the host from developing disease subsequent to a challenge infection.
Early studies, including those by our group, investigating prime/challenge animal models (though they were not necessarily described as such) for autoimmune demyelinating disease were performed in the context of EAE. Two groups, using animals other than mice, demonstrated that a viral infection (prime) could enhance/allow EAE induction by injection of neuroantigens (challenge) [(Liebert et al. 1990; Massanari et al. 1979); reviewed in (Barnett and Fujinami 1992)]. The first group showed that a persistent (heat-inactivated virus did not work) measles virus infection (prime) in hamsters potentiated the development and severity of EAE induced by injection of neuroantigen (guinea pig spinal cord) in complete Freund’s adjuvant (CFA; challenge) (Massanari et al. 1979). The second group showed that a subclinical measles virus infection (prime) in Lewis rats allowed for the induction of EAE upon injection of the normally nonencephalitogenic MBP peptide, MBP69–81, in CFA (challenge), and this induction of EAE was dependent on measles virus replication in the CNS (intraperitoneal injection of virus and heat-inactivated virus did not work) (Liebert et al. 1990). One group, using mice, demonstrated that subclinical, transient infection of the CNS with Semliki Forest virus (prime) allowed for the induction of EAE in resistant C57BL/6 mice upon injection of whole MBP in CFA (challenge), or upon adoptive transfer of MBP-sensitized lymphocytes (challenge) (Mokhtarian and Swoveland 1987). Together, these studies demonstrate that a viral infection of the CNS can prime the immune system for the development of demyelinating disease upon subsequent challenge with neuroantigens in model systems where neuroantigen challenge alone induces disease rarely (guinea pig spinal cord in CFA in hamsters) or not at all (MBP69–81 in CFA in Lewis rats; whole MBP in CFA in C57BL/6 mice) (Liebert et al. 1990; Massanari et al. 1979; Mokhtarian and Swoveland 1987).
The above studies demonstrated that persistent or transient viral infection of the CNS could prime for the later induction of EAE. This priming effect could occur through several mechanisms. Viral-induced damage to the CNS could facilitate the subsequent activation and/or clonal expansion of preexisting myelin-reactive lymphocytes (Liebert et al. 1990; Mokhtarian and Swoveland 1987). Cellular components together with viral envelop proteins could be exposed on the surface of infected cells due to viral-induced alterations of the surface of infected cells (Liebert et al. 1990). Finally, changes in the integrity of the blood–brain barrier due to viral infection could facilitate antigen-specific lymphocyte infiltration of the CNS (Liebert et al. 1990).
Our group has continued to examine and develop this prime/challenge hypothesis in mice over the last several years. Our initial study demonstrated that peripheral infection, via tail scarification, of SJL/J mice with a recombinant vaccinia virus carrying the entire coding region of rat PLP did not induce CNS disease by itself, but instead primed the mice for the development of an earlier and enhanced CNS disease (EAE) upon subcutaneous injection of the PLP139–151 peptide (identical between rat and mouse) in CFA plus intravenous injection of Bordetella pertussis (challenge) (Barnett et al. 1993). The small amount of vaccinia virus used for infection/vaccination in this study resulted in localized dermal replication of the virus without infection of the CNS. Thus, prior peripheral infection, with a virus capable of coding for a self protein (molecular mimicry), can prime the host immune system for an enhanced autoimmune response triggered by a later challenge (Barnett et al. 1993).
The above study was extended by the use of other encephalitogenic PLP peptides (PLP178–191, PLP104–117) as challenge antigens in this system and by the examination of the humoral immune response in these mice (Wang and Fujinami 1997). Acute EAE induced in susceptible strains of mice by direct administration of PLP178–191 is very similar to the acute EAE induced by PLP139–151; however, EAE induced using PLP104–117 is associated with a delayed onset and slow chronic progressive disease. The enhanced CNS disease (EAE) observed in vaccinated mice upon injection of the PLP139–151 peptide in adjuvant (challenge) was also observed upon injection of the PLP104–117 peptide in adjuvant, but it was not observed upon injection of the PLP178–191 peptide in adjuvant. With respect to the humoral immune response, antibodies specific for PLP and the various PLP peptides were present in the sera of primed mice prior to the challenge, and the respective PLP peptide-specific antibodies increased subsequent to challenge with the respective peptides. Following peptide challenge, the anti PLP IgG response shifted from an IgG1 to an IgG2a (IgG2c) and 2b phenotype. Thus, this study demonstrates that a humoral immune response to encephalitogenic PLP peptides can be generated by infection with a virus capable of coding for a self CNS protein (Wang and Fujinami 1997).An interesting addition to the above study, in which we prime with vaccinia virus encoding PLP and challenge with the PLP139–151 peptide in CFA plus B. pertussis, is the demonstration that, when the B. pertussis supplementation is removed, there is still an initial early and enhanced acute attack of CNS disease (EAE) (Wang et al. 1999). However, following the initial earlier and enhanced CNS disease, the mice seldom experienced a clinical relapse, and if a relapse occurred, it was very mild and the mouse recovered very quickly. At this later time point (35–60 days post challenge), there was found to be significantly less demyelination and inflammation in the CNS of the vaccinated mice and lymphoproliferation in response to PLP peptide was significantly decreased, compared to controls. This reduced immune responsiveness suggests either unresponsiveness or regulated suppression, resulting in a permanent remission state (Wang et al. 1999).
In contrast to the above studies in which a viral infection primes the immune system for autoimmunity subsequent to a triggering challenge event, it was found that peripheral infection, via tail scarification or intraperitoneal injection, of PL/J mice with a recombinant vaccinia virus encoding the self peptide MBP1–23, which did not induce CNS disease by itself, protected the mice from developing CNS disease (EAE) upon challenge with either purified guinea pig MBP or the acetylated MBP1–20 peptide in CFA (subcutaneous injection) plus intravenous injection of B. pertussis (Barnett et al. 1996). This result is allowed for in the prime/challenge model. The observed protection was found to be both mouse strain specific, as SJL/J mice were not protected, and challenge antigen specific, as the protection did not extend to challenge with whole spinal cord homogenate. Also, this protection did not extend to the adoptive transfer of MBP1–11-specific activated T cells. Examination of the delayed-type hypersensitivity response in this system suggested an immunological basis for the protection. The inability of T cells from these vaccinated/challenged mice to, in turn, adoptively transfer disease to naïve mice suggests anergy or deletion of effector T cells in these protected mice; although CD8+ T cells do not participate in the protection as in vivo depletion of CD8+ T cells did not remove the protective effect. Thus, prior peripheral infection with a virus capable of coding for a self epitope (altered peptide ligand, the encoded self epitope is not acetylated) can protect the host from an autoimmune response that would normally be triggered by a particular challenge (Barnett et al. 1996).
The above studies demonstrate that either enhancement of or protection from disease can occur after a subsequent challenge depending on the CNS protein encoded by the vaccinia virus vaccine. In turn, the ultimate response to a challenge infection may depend on what CNS epitope a priming virus has in common with self. To explore further the idea that different epitopes present at the priming step could determine the outcome after challenge, cDNAs encoding self CNS epitopes were constructed and replaced vaccinia virus vaccination in our prime/challenge model (Theil et al. 2001; Tsunoda et al. 1998). In the initial study, cDNAs that encoded the entire PLP protein (PLPall) and the PLP peptides PLP139–151 and PLP178–191 were constructed. It was found that all three DNA constructs, injected intramuscularly, individually could induce a PLP-specific lymphoproliferative response, which was shown to be CD4+ T cell-mediated, without inducing CNS disease. All three DNA constructs, when injected as the priming step, enhanced the CNS disease (more severe disease and more frequent relapses) that developed subsequent to challenge with PLP139–151 peptide in CFA, while only priming with PLPall enhanced disease following challenge with PLP178–191 peptide in CFA. Also, the PLP-specific lymphoproliferative responses present in primed mice prior to challenge increased subsequent to challenge with the PLP peptides (Tsunoda et al. 1998). In a subsequent study, a cDNA was constructed that encoded ubiquitin fused to PLP (UPLP), leading to enhanced degradation of PLP through the proteasome pathway and the resulting PLP peptides were presented through the major histocompatibility (MHC) class I pathway (Theil et al. 2001). This method mimics infection with an intracellular virus that has molecular mimicry with CNS antigens without causing cytopathic effects in the host. Mice primed with UPLP and then challenged with phosphate-buffered saline (PBS) in CFA or with PLP139–151 in CFA developed clinical and pathological signs of CNS disease. Mice primed with UPLP and then challenged with recombinant vaccinia virus encoding β-galactosidase developed pathological signs of CNS disease without any clinical signs of the disease. In contrast, mice primed with PLPall and challenged with PBS in CFA did not develop pathological or clinical signs of the disease, thus indicating that the initial priming event may require efficient MHC class I presentation of the mimicking antigen which occurs with the ubiquitinated construct (Theil et al. 2001). An extension of this study more closely examined mice primed with UPLP and then challenged with PLP139–151 in CFA (Theil et al. 2008). It was found that these mice experienced a milder relapse phase (1 month post challenge), compared to controls. During the relapse phase, these mice had decreased clinical and pathological signs of disease, decreased in vitro lymphoproliferation to PLP139–151, reduced IFN-γ production and increased IL-4 production. In addition, CD8+ T cells were found to be activated and expanded in these mice, confirming that degradation through the proteasome pathway and presentation by the MHC class I pathway was occurring, and these CD8+ T cells could contribute to the modulation of the disease observed in these mice (Theil et al. 2008).
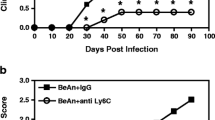
In addition to exploring the effect of the priming epitope, our group has explored various challenge events, in addition to the standard injection of PLP peptide in CFA, in our prime/challenge model (Theil et al. 2001; Tsunoda et al. 2007a). For our initial study, recombinant vaccinia viruses carrying the entire coding regions of PLP, glial fibrillary acidic protein (GFAP) and myelin associated glycoprotein (MAG) were constructed (Theil et al. 2001). Peripheral infection, via tail scarification, of SJL/J mice with any of the three vaccinia virus vaccines did not induce CNS disease. A subsequent nonspecific immunologic challenge with CFA, plus B. pertussis, resulted in the induction of pathological inflammatory CNS lesions without any clinical signs of disease. This shows that CNS proteins that are less encephalitogenic myelin antigens (MAG) and nonmyelin antigens (GFAP) can prime for disease, and that the challenge event can be a nonspecific immunologic stimulus. In comparison, priming of PL/J mice with the vaccinia viruses carrying PLP and GFAP followed by challenge with CFA, with or without B. pertussis, did not result in pathological or clinical signs of disease, thus reinforcing the importance of genetic background in the development of disease (Theil et al. 2001). In a subsequent study, the priming event was peripheral infection, via intraperitoneal injection, of SJL/J mice with a vaccinia virus vaccine encoding PLP (Tsunoda et al. 2007a). The challenge event was viral infection, via intraperitoneal injection, with several different viruses that either do not cause CNS disease on their own or cause a meningitis type of disease. Mice challenged with murine cytomegalovirus (MCMV; Smith strain) infection developed pathological signs of CNS disease, while mice challenged with lymphocytic choriomeningitis virus (LCMV; Armstrong strain) and the wild type strain of vaccinia virus (WR strain) did not develop the disease (Tsunoda et al. 2007a). One explanation of these results is that certain kinds of viral infections (MCMV) that promote IL-12 production, which contributes to the preferential development of Th1 responses (IFN-γ) over Th2 responses (IL-4), and possibly production of other members of the IL-12 family, such as IL-23 and IL-27, may be responsible for exacerbating or triggering MS through bystander activation of autoreactive T cells [(Tsunoda et al. 2007a); reviewed in (Fujinami 2001b; McCoy et al. 2006)]. Other kinds of viral infections (LCMV) that induce IFN-α/β production may suppress autoimmunity [(Tsunoda et al. 2007a); reviewed in (Fujinami 2001b; McCoy et al. 2006)]. The induction of IFN-α/β by infection may suppress autoimmunity through the downregulation of IL-12 [reviewed in (Fujinami 2001b)]. The priming with vaccinia virus encoding PLP followed by challenge with wild type vaccinia virus may not have resulted in disease due to rapid clearance of the virus (Tsunoda et al. 2007a).
8 Conclusion
This prime/challenge hypothesis easily explains why no one causative viral infection has ever been unequivocally proven to exist as the etiological agent of MS. If an initial encounter with any number of infectious agents can prime genetically susceptible individuals for CNS disease without causing overt disease, and overt disease only occurs after an encounter with any number of specific or nonspecific agents, then the likelihood of isolating one specific causative viral infection for MS is very low. The variability in the priming and challenging organisms may also contribute to the variability in the clinical course of MS observed in individual patients.
The explanation for how many different microbial infections can induce and exacerbate a single autoimmune disease has been described as the fertile-field hypothesis [(von Herrath et al. 2003); reviewed in (Fujinami et al. 2006)]. Autoreactive cells could be initially primed by both molecular mimicry and bystander activation, thus setting up a fertile-field, and then subsequent infection by a broad range of microorganisms could activate the preexisting autoreactive cells to autoagression through bystander activation. The fertile-field, induced by infection of the host and interactions between the immune response and the virus, would be transient and could change quantitatively and qualitatively over the course of infection depending on the type, anatomical location and duration of the infection. The initial priming event and the subsequent challenge event need not occur within the target organ, may be greatly separated in time, and more than one subsequent challenge event may be required for the development of overt disease [(von Herrath et al. 2003); reviewed in (Fujinami et al. 2006)]. The identification and characterization of viruses that are able to set up a fertile field within the host and then the identification and characterization of viruses that are able to trigger disease from the fertile field are challenges that remain open for future experimentation.
The identification of common inflammatory responses to otherwise distinct pathogens could lead us to the mechanism for how the prime/challenge model results in autoimmune disease (von Herrath et al. 2003). As described above, it has been found that a challenge virus (MCMV) that induces the production of IL-12 also induces the development of disease in an animal primed for autoimmune disease by exposure to a virus encoding a molecular mimic to a CNS protein (Tsunoda et al. 2007a). With this in mind, it is interesting to note that several viruses that are known to induce the production of IL-12, including herpes simplex virus, HHV-6, influenza virus and coronavirus, are viruses that have either been isolated from MS patients or associated with exacerabations of MS [reviewed in (Fujinami 2001b)]. The identification of immunomodulatory molecules that play a role in either the induction and/or exacerbation or the amelioration of CNS disease is a step towards being able to intelligently design vaccines that prevent disease through immune regulation.
References
Álvarez-Lafuente R, de Las Hervas V, Bartolome M, Picazo JJ, Arroyo R (2004) Relapsing-remitting multiple sclerosis and human herpesvirus 6 active infection. Arch Neurol 61:1523–1527
Álvarez-Lafuente R, de Las Hervas V, Garcia-Montojo M, Bartolome M, Arroyo R (2007) Human herpesvirus-6 and multiple sclerosis: relapsing-remitting versus secondary progressive. Mult Scler 13:578–583
Álvarez-Lafuente R, Garcia-Montojo M, de Las Hervas V, Bartolome M, Arroyo R (2006) Clinical parameters and HHV-6 active replication in relapsing-remitting multiple sclerosis patients. J Clin Virol 37(Suppl 1):S24–S26
Andersen O, Lygner PE, Bergstrom T, Andersson M, Vahlne A (1993) Viral infections trigger multiple sclerosis relapses: a prospective seroepidemiological study. J Neurol 240:417–422
Ascherio A, Munch M (2000) Epstein-Barr virus and multiple sclerosis. Epidemiology 11:220–224
Ascherio A, Munger KL (2007a) Environmental risk factors for multiple sclerosis. Part I: the role of infection. Ann Neurol 61:288–299
Ascherio A, Munger KL (2007b) Environmental risk factors for multiple sclerosis. Part II: noninfectious factors. Ann Neurol 61:504–513
Asher DM (1991) Slow viral infections of the human nervous system. In: Scheld WM, Whitley RJ, Durack DT (eds) Infections of the central nervous system. Raven, New York, pp 145–166
Babbe H, Roers A, Waisman A, Lassmann H, Goebels N, Hohlfeld R, Friese M, Schroder R, Deckert M, Schmidt S, Ravid R, Rajewsky K (2000) Clonal expansions of CD8+ T cells dominate the T cell infiltrate in active multiple sclerosis lesions as shown by micromanipulation and single cell polymerase chain reaction. J Exp Med 192:393–404
Barnett LA, Fujinami RS (1992) Molecular mimicry: a mechanism for autoimmune injury. FASEB J 6:840–844
Barnett LA, Whitton JL, Wada Y, Fujinami RS (1993) Enhancement of autoimmune disease using recombinant vaccinia virus encoding myelin proteolipid protein [published erratum appears in J. Neuroimmunol. 48:120, 1993]. J Neuroimmunol 44:15–25
Barnett LA, Whitton JL, Wang LY, Fujinami RS (1996) Virus encoding an encephalitogenic peptide protects mice from experimental allergic encephalomyelitis. J Neuroimmunol 64:163–173
Berti R, Brennan MB, Soldan SS, Ohayon JM, Casareto L, McFarland HF, Jacobson S (2002) Increased detection of serum HHV-6 DNA sequences during multiple sclerosis (MS) exacerbations and correlation with parameters of MS disease progression. J NeuroVirol 8:250–256
Bjartmar C, Wujek JR, Trapp BD (2003) Axonal loss in the pathology of MS: consequences for understanding the progressive phase of the disease. J Neurol Sci 206:165–171
Brahic M, Bureau JF, Michiels T (2005) The genetics of the persistent infection and demyelinating disease caused by Theiler’s virus. Annu Rev Microbiol 59:279–298
Buljevac D, Flach HZ, Hop WCJ, Hijdra D, Laman JD, Savelkoul HFJ, van der Meché FGA, Van Doorn PA, Hintzen RQ (2002) Prospective study on the relationship between infections and multiple sclerosis exacerbations. Brain 125:952–960
Buljevac D, van Doornum GJ, Flach HZ, Groen J, Osterhaus AD, Hop W, Van Doorn PA, van der Meché FGA, Hintzen RQ (2005) Epstein-Barr virus and disease activity in multiple sclerosis. J Neurol Neurosurg Psychiatr 76:1377–1381
Cepok S, Zhou D, Srivastava R, Nessler S, Stei S, Bussow K, Sommer N, Hemmer B (2005) Identification of Epstein-Barr virus proteins as putative targets of the immune response in multiple sclerosis. J Clin Invest 115:1352–1360
Challoner PB, Smith KT, Parker JD, MacLeod DL, Coulter SN, Rose TM, Schultz ER, Bennett JL, Garber RL, Chang M, Schad PA, Stewart PM, Nowinski RC, Brown JP, Burmer GC (1995) Plaque-associated expression of human herpesvirus 6 in multiple sclerosis. Proc Natl Acad Sci U S A 92:7440–7444
Christensen T (2007) Human herpesviruses in MS. Int MS J 14:41–47
Cirone M, Cuomo L, Zompetta C, Ruggieri S, Frati L, Faggioni A, Ragona G (2002) Human herpesvirus 6 and multiple sclerosis: a study of T cell cross-reactivity to viral and myelin basic protein antigens. J Med Virol 68:268–272
Coo H, Aronson KJ (2004) A systematic review of several potential non-genetic risk factors for multiple sclerosis. Neuroepidemiology 23:1–12
Correale J, Fiol M, Gilmore W (2006) The risk of relapses in multiple sclerosis during systemic infections. Neurology 67:652–659
De Keyser J, Zwanikken C, Boon M (1998) Effects of influenza vaccination and influenza illness on exacerbations in multiple sclerosis. J Neurol Sci 159:51–53
Derfuss T, Hohlfeld R, Meinl E (2005) Intrathecal antibody (IgG) production against human herpesvirus type 6 occurs in about 20% of multiple sclerosis patients and might be linked to a polyspecific B-cell response. J Neurol 252:968–971
Dutta R, Trapp BD (2007) Pathogenesis of axonal and neuronal damage in multiple sclerosis. Neurology 68:S22-S31
Edwards S, Zvartau M, Clarke H, Irving W, Blumhardt LD (1998) Clinical relapses and disease activity on magnetic resonance imaging associated with viral upper respiratory tract infections in multiple sclerosis. J Neurol Neurosurg Psychiatr 64:736–741
Evans BK, Donely DK, Whitaker JN (1991) Neurological manifestations of infection with the human immunodeficiency viruses. In: Scheld WM, Whitley RJ, Durack DT (eds) Infections of the central nervous system. Raven, New York, pp 201–232
Fotheringham J, Jacobson S (2005) Human herpesvirus 6 and multiple sclerosis: potential mechanisms for virus-induced disease. Herpes 12:4–9
Fujinami RS (1996) Molecular mimicry. In: Shoenfeld Y, Peter JB (eds) Autoantibodies. Elsevier, Amsterdam, pp 507–519
Fujinami RS (1998) Molecular Mimicry. In: Rose NR, Mackay IR (eds) The autoimmune diseases. 3rd edn. Academic Press, San Diego, CA, pp 141–149
Fujinami RS (2000) Molecular mimicry and central nervous system autoimmune disease. In: Cunningham MW, Fujinami RS (eds) Molecular mimicry, microbes and autoimmunity, ASM, Washington, D C, pp 27–38
Fujinami RS (2001a) Can virus infections trigger autoimmune disease? J Autoimmun 16:229–234
Fujinami RS (2001b) Viruses and autoimmune disease–two sides of the same coin? Trends Microbiol 9:377–381
Fujinami RS, von Herrath MG, Christen U, Whitton JL (2006) Molecular mimicry, bystander activation, or viral persistence: infections and autoimmune disease. Clin Microbiol Rev 19:80–94
Gilden DH (2002) Multiple sclerosis exacerbations and infection. Lancet Neurol 1:145
Goverman J, Woods A, Larson L, Weiner LP, Hood L, Zaller DM (1993) Transgenic mice that express a myelin basic protein-specific T cell receptor develop spontaneous autoimmunity. Cell 72:551–560
Granieri E, Casetta I, Tola MR, Ferrante P (2001) Multiple sclerosis: infectious hypothesis. Neurol Sci 22:179–185
Hafler DA, Compston A, Sawcer S, Lander ES, Daly MJ, de Jager PL, de Bakker PI, Gabriel SB, Mirel DB, Ivinson AJ, Pericak-Vance MA, Gregory SG, Rioux JD, McCauley JL, Haines JL, Barcellos LF, Cree B, Oksenberg JR, Hauser SL (2007) Risk alleles for multiple sclerosis identified by a genomewide study. N Engl J Med 357:851–862
Holmoy T, Kvale EO, Vartdal F (2004) Cerebrospinal fluid CD4+ T cells from a multiple sclerosis patient cross-recognize Epstein-Barr virus and myelin basic protein. J NeuroVirol 10:278–283
Johnson RT (1998) Viral infections of the nervous system. Lippincott-Raven, Philadelphia
Kantarci OH (2008) Genetics and natural history of multiple sclerosis. Semin Neurol 28:7–16
Kriesel JD, Sibley WA (2005) Editorial: the case for rhinoviruses in the pathogenesis of multiple sclerosis. Mult Scler 11:1–4
Kriesel JD, White A, Hayden FG, Spruance SL, Petajan J (2004) Multiple sclerosis attacks are associated with picornavirus infections. Mult Scler 10:145–148
Kurtzke JF (1993) Epidemiologic evidence for multiple sclerosis as an infection. Clin Microbiol Rev 6:382–427
Kurtzke JF (1997) The epidemiology of multiple sclerosis. In: Raine CS, McFarland HF, Tourtellotte WW (eds) Multiple sclerosis: clinical and pathogenetic basis. Chapman & Hall, London, pp 91–140
Kurtzke JF, Heltberg A (2001) Multiple sclerosis in the Faroe Islands: an epitome. J Clin Epidemiol 54:1–22
Leibowitz U, Antonovsky A, Medalie JM, Smith HA, Halpern L, Alter M (1966) Epidemiological study of multiple sclerosis in Israel. II. Multiple sclerosis and level of sanitation. J Neurol Neurosurg Psychiatr 29:60–68
Levin LI, Munger KL, Rubertone MV, Peck CA, Lennette ET, Spiegelman D, Ascherio A (2005) Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA 293:2496–2500
Libbey JE, Fujinami RS (2002) Are virus infections triggers for autoimmune disease? Clin Microbiol Newslett 24:73–76
Libbey JE, Fujinami RS (2003) Viral demyelinating disease in experimental animals. In: Herndon RM (ed) Multiple sclerosis: immunology, pathology and pathophysiology. Demos, New York, pp 125–133
Libbey JE, McCoy LL, Fujinami RS (2007) Molecular mimicry in multiple sclerosis. Int Rev Neurobiol 79:127–147
Liebert UG, Hashim GA, ter Meulen V (1990) Characterization of measles virus-induced cellular autoimmune reactions against myelin basic protein in Lewis rats. J Neuroimmunol 29:139–147
Lunemann JD, Edwards N, Muraro PA, Hayashi S, Cohen JI, Munz C, Martin R (2006) Increased frequency and broadened specificity of latent EBV nuclear antigen-1-specific T cells in multiple sclerosis. Brain 129:1493–1506
Lunemann JD, Kamradt T, Martin R, Munz C (2007) Epstein-barr virus: environmental trigger of multiple sclerosis? J Virol 81:6777–6784
Lunemann JD, Munz C (2007) Epstein-Barr virus and multiple sclerosis. Curr Neurol Neurosci Rep 7:253–258
Maggi F, Fornai C, Vatteroni ML, Siciliano G, Menichetti F, Tascini C, Specter S, Pistello M, Bendinelli M (2001) Low prevalence of TT virus in the cerebrospinal fluid of viremic patients with central nervous system disorders. J Med Virol 65:418–422
Marrie RA, Wolfson C, Sturkenboom MC, Gout O, Heinzlef O, Roullet E, Abenhaim L (2000) Multiple sclerosis and antecedent infections: a case-control study. Neurology 54:2307–2310
Massanari RM, Paterson PY, Lipton HL (1979) Potentiation of experimental allergic encephalomyelitis in hamsters with persistent encephalitis due to measles virus. J Infect Dis 139:297–303
McCoy L, Tsunoda I, Fujinami RS (2006) Multiple sclerosis and virus induced immune responses: autoimmunity can be primed by molecular mimicry and augmented by bystander activation. Autoimmunity 39:9–19
McElroy JP, Oksenberg JR (2008) Multiple sclerosis genetics. Curr Top Microbiol Immunol 318:45–72
Metz LM, McGuinness SD, Harris C (1998) Urinary tract infections may trigger relapse in multiple sclerosis. Axone 19:67–70
Miller SD, Vanderlugt CL, Begolka WS, Pao W, Yauch RL, Neville KL, Katz-Levy Y, Carrizosa A, Kim BS (1997) Persistent infection with Theiler’s virus leads to CNS autoimmunity via epitope spreading. Nat Med 3:1133–1136
Mokhtarian F, Swoveland P (1987) Predisposition to EAE induction in resistant mice by prior infection with Semliki forest virus. J Immunol 138:3264–3268
Niino M, Fukazawa T, Kikuchi S, Sasaki H (2007) Recent advances in genetic analysis of multiple sclerosis: genetic associations and therapeutic implications. Expert Rev Neurother 7:1175–1188
Oleszak EL, Chang JR, Friedman H, Katsetos CD, Platsoucas CD (2004) Theiler’s virus infection: a model for multiple sclerosis. Clin Microbiol Rev 17:174–207
Oleszak EL, Leibowitz JL, Rodriguez M (1988) Isolation and characterization of two plaque size variants of Theiler’s murine encephalomyelitis virus (DA strain). J Gen Virol 69(Pt 9):2413–2418
Olson JK, Croxford JL, Calenoff MA, Dal Canto MC, Miller SD (2001) A virus-induced molecular mimicry model of multiple sclerosis. J Clin Invest 108:311–318
Panitch HS (1994) Influence of infection on exacerbations of multiple sclerosis. Ann Neurol 36(Suppl):S25–S28
Patick AK, Oleszak EL, Leibowitz JL, Rodriguez M (1990) Persistent infection of a glioma cell line generates a Theiler’s virus variant which fails to induce demyelinating disease in SJL/J mice. J Gen Virol 71:2123–2132
Pender MP, Greer JM (2007) Immunology of multiple sclerosis. Curr Allergy Asthma Rep 7:285–292
Peterson LK, Fujinami RS (2006) Molecular mimicry. In: Shoenfeld Y, Gershwin ME, Meroni P-L (eds) Autoantibodies, 2nd edn. Elsevier, Philadelphia, pp 13–20
Pohl D, Krone B, Rostasy K, Kahler E, Brunner E, Lehnert M, Wagner HJ, Gartner J, Hanefeld F (2006) High seroprevalence of Epstein-Barr virus in children with multiple sclerosis. Neurology 67:2063–2065
Poskanzer DC, Schapira K, Miller H (1963a) Comparison of the epidemiology of multiple sclerosis and of poliomyelitis. Trans Am Neurol Assoc 88:253–255
Poskanzer DC, Schapira K, Miller H (1966) Multiple sclerosis and poliomyelitis. Acta Neurol Scand 42;Suppl 19:85–90
Poskanzer DC, Schapria K, Miller H (1963b) Multiple sclerosis and poliomyelitis. Lancet 2:917–921
Robertson NP, Clayton D, Fraser M, Deans J, Compston DA (1996) Clinical concordance in sibling pairs with multiple sclerosis. Neurology 47:347–352
Rutschmann OT, McCrory DC, Matchar DB (2002) Immunization and MS: a summary of published evidence and recommendations. Immunization Panel of the Multiple Sclerosis Council for Clinical Practice and Guidelines. Neurology 59:1837–1843
Serafini B, Rosicarelli B, Franciotta D, Magliozzi R, Reynolds R, Cinque P, Andreoni L, Trivedi P, Salvetti M, Faggioni A, Aloisi F (2007) Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. J Exp Med 204:2899–2912
Sibley WA, Bamford CR, Clark K (1985) Clinical viral infections and multiple sclerosis. Lancet 1:1313–1315
Simmonds P (2002) TT virus infection: a novel virus-host relationship. J Med Microbiol 51:455–458
Soldan SS, Fogdell-Hahn A, Brennan MB, Mittleman BB, Ballerini C, Massacesi L, Seya T, McFarland HF, Jacobson S (2001) Elevated serum and cerebrospinal fluid levels of soluble human herpesvirus type 6 cellular receptor, membrane cofactor protein, in patients with multiple sclerosis. Ann Neurol 50:486–493
Sospedra M, Martin R (2005) Immunology of multiple sclerosis. Annu Rev Immunol 23:683–747
Sospedra M, Martin R (2006) Molecular mimicry in multiple sclerosis. Autoimmunity 39:3–8
Sospedra M, Zhao Y, Zur HH, Muraro PA, Hamashin C, de Villiers E-M, Pinilla C, Martin R (2005) Recognition of conserved amino acid motifs of common viruses and its role in autoimmunity. PLoS Pathog 1:e41
Tejada-Simon MV, Zang YCQ, Hong J, Rivera VM, Zhang JZ (2003) Cross-reactivity with myelin basic protein and human herpesvirus-6 in multiple sclerosis. Ann Neurol 53:189–197
Thacker EL, Mirzaei F, Ascherio A (2006) Infectious mononucleosis and risk for multiple sclerosis: a meta-analysis. Ann Neurol 59:499–503
Theil DJ, Libbey JE, Rodriguez F, Whitton JL, Tsunoda I, Derfuss TJ, Fujinami RS. (2008) Targeting myelin proteolipid protein to the MHC class I pathway by ubiquitination modulates the course of experimental autoimmune encephalomyelitis. J Neuroimmunol 204:92-100
Theil DJ, Tsunoda I, Rodriguez F, Whitton JL, Fujinami RS (2001) Viruses can silently prime for and trigger central nervous system autoimmune disease. J NeuroVirol 7:220–227
Torkildsen O, Nyland H, Myrmel H, Myhr KM (2008) Epstein-Barr virus reactivation and multiple sclerosis. Eur J Neurol 15:106–108
Tsunoda I, Fujinami RS (1996) Two models for multiple sclerosis: experimental allergic encephalomyelitis and Theiler’s murine encephalomyelitis virus. J Neuropathol Exp Neurol 55:673–686
Tsunoda I, Fujinami RS (2002) Inside-out versus Outside-in models for virus induced demyelination: axonal damage triggering demyelination. Springer Semin Immunopathol 24:105–125
Tsunoda I, Kuang L-Q, Libbey JE, Fujinami RS (2003) Axonal injury heralds virus-induced demyelination. Am J Pathol 162:1259–1269
Tsunoda I, Kuang L-Q, Tolley ND, Whitton JL, Fujinami RS (1998) Enhancement of experimental allergic encephalomyelitis (EAE) by DNA immunization with myelin proteolipid protein (PLP) plasmid DNA. J Neuropathol Exp Neurol 57:758–767
Tsunoda I, Libbey JE, Fujinami RS (2007a) Sequential polymicrobial infections lead to CNS inflammatory disease: possible involvement of bystander activation in heterologous immunity. J Neuroimmunol 188:22–33
Tsunoda I, Tanaka T, Saijoh Y, Fujinami RS (2007b) Targeting inflammatory demyelinating lesions to sites of Wallerian degeneration. Am J Pathol 171:1563–1575
Vandevelde M, Zurbriggen A (2005) Demyelination in canine distemper virus infection: a review. Acta Neuropathol 109:56–68
Virtanen JO, Farkkila M, Multanen J, Uotila L, Jaaskelainen AJ, Vaheri A, Koskiniemi M (2007) Evidence for human herpesvirus 6 variant A antibodies in multiple sclerosis: diagnostic and therapeutic implications. J Neurovirol 13:347–352
von Herrath MG, Fujinami RS, Whitton JL (2003) Microorganisms and autoimmunity: making the barren field fertile? Nat Rev Microbiol 1:151–157
Wandinger K, Jabs W, Siekhaus A, Bubel S, Trillenberg P, Wagner H, Wessel K, Kirchner H, Hennig H (2000) Association between clinical disease activity and Epstein-Barr virus reactivation in MS. Neurology 55:178–184
Wang L-Y, Fujinami RS (1997) Enhancement of EAE and induction of autoantibodies to T-cell epitopes in mice infected with a recombinant vaccinia virus encoding myelin proteolipid protein. J Neuroimmunol 75:75–83
Wang L-Y, Theil DJ, Whitton JL, Fujinami RS (1999) Infection with a recombinant vaccinia virus encoding myelin proteolipid protein causes suppression of chronic relapsing-remitting experimental allergic encephalomyelitis. J Neuroimmunol 96:148–157
Whitley RJ, Schlitt M (1991) Encephalitis caused by herpesviruses, including B virus. In: Scheld WM, Whitley RJ, Durack DT (eds) Infections of the central nervous system. Raven, New York, pp 41–86
Whitton JL, Fujinami RS (1999) Viruses as triggers of autoimmunity: facts and fantasies. Curr Opin Microbiol 2:392–397
Acknowledgements
We are grateful to Ms. Kathleen Borick for preparation of the manuscript. This work was supported by NIH AI581501.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer Berlin Heidelberg
About this chapter
Cite this chapter
Libbey, J.E., Fujinami, R.S. (2009). Potential Triggers of MS. In: Martin, R., Lutterotti, A. (eds) Molecular Basis of Multiple Sclerosis. Results and Problems in Cell Differentiation, vol 51. Springer, Berlin, Heidelberg. https://doi.org/10.1007/400_2008_12
Download citation
DOI: https://doi.org/10.1007/400_2008_12
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-14152-2
Online ISBN: 978-3-642-14153-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)