Abstract
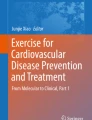
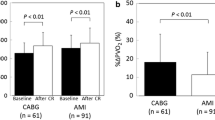
Cardiac rehabilitation (CR) plays an important role in cardiovascular disease prevention. Understanding the key component of CR such as training intensity and biomarkers reflecting cardiopulmonary functions may help to better target the rehabilitation program. Thirty-four consecutive patients with coronary artery disease after percutaneous coronary intervention participated in the CR program. The difference between intervention group and control group was mainly the training intensity. Cardiopulmonary exercise testing (CPET) and blood biomarker measurements were performed before and after CR. The results demonstrated that it was safe and feasible to perform CR, while sufficient training intensity was required to significantly ameliorate CPET parameters. Among numerous biomarkers tested, vasopressin surrogate marker copeptin (CPP) improved significantly after CR. Moreover, improved CPP was correlated with exercise intensity and peak oxygen uptake, two most important indicators of cardiopulmonary exercise capacities. Therefore, CR may have a novel role in maintaining plasma osmolality and cardiovascular homeostasis.

Cardiac rehabilitation training improves cardiopulmonary exercise parameters El and PVO2 which are correlated with reduced CPP level. CPP, copeptin; El, exercise intensity; POV2, peak oxygen uptake.




Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CAD:
-
Coronary artery disease
- CPET:
-
Cardiopulmonary exercise testing
- CPP:
-
Copeptin
- CR:
-
Cardiac rehabilitation
- EI:
-
Exercise intensity
- ELISA:
-
Enzyme-linked immunosorbent assay
- HRR:
-
Heart rate reserve
- IFN-γ:
-
Interferon gamma
- IL:
-
Interleukin
- MET:
-
Metabolic equivalent of task
- MHR:
-
Maximum heart rate
- O2 pulse:
-
Oxygen pulse
- PCI:
-
Percutaneous coronary intervention
- PTX3:
-
Pentraxin 3
- PVO2 :
-
Peak oxygen uptake
- RDBP:
-
Resting diastolic blood pressure
- RHR:
-
Resting heart rate
- RSBP:
-
Resting systolic blood pressure
- TNF-α:
-
Tumor necrosis factor alpha
- VAT:
-
Ventilatory anaerobic threshold
- VE/CO2 :
-
Ventilation/carbon dioxide output ratio
- VEGF:
-
Vascular endothelial growth factor
- WC:
-
Waist circumference
References
Naghavi, M., Wang, H., Lozano, R., et al. (2015). Global, regional, and national age sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet, 385, 117–171.
Liu, S., Li, Y., Zeng, X., Wang, H., Yin, P., Wang, L., et al. (2019). Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 Global Burden of Disease Study. JAMA Cardiology, 4(4), 342–352.
Chen, W. W., Gao, R. L., Liu, L. S., Zhu, M. L., Wang, W., Wang, Y. J., et al. (2017). China cardiovascular diseases report 2015: a summary. Journal of Geriatric Cardiology, 14, 1–10.
Wu, Y., Benjamin, E. J., & Macmahon, S. (2016). Prevention and control of cardiovascular disease in the rapidly changing economy of China. Circulation, 133, 2545.
Batacan Jr., R. B., Duncan, M. J., Dalbo, V. J., Buitrago, G. L., & Fenning, A. S. (2018). Effect of different intensities of physical activity on cardiometabolic markers and vascular and cardiac function in adult rats fed with a high-fat high-carbohydrate diet. Journal of Sport and Health Science, 7(1), 109–119.
van Halewijn, G., Deckers, J., Tay, H. Y., van Domburg, R., Kotseva, K., & Wood, D. (2017). Lessons from contemporary trials of cardiovascular prevention and rehabilitation: a systematic review and meta-analysis. International Journal of Cardiology, 232, 294–303.
Shepherd, C. W., & While, A. E. (2012). Cardiac rehabilitation and quality of life: a systematic review. International Journal of Nursing Studies, 49(6), 755–771.
Keteyian, S. J., Brawner, C. A., Savage, P. D., Ehrman, J. K., Schairer, J., Divine, G., Aldred, H., Ophaug, K., & Ades, P. A. (2008). Peak aerobic capacity predicts prognosis in patients with coronary heart disease. American Heart Journal, 156(2), 292–300.
Solbraa, A. K., Anderssen, S. A., Holme, I. M., et al. (2018). The built environment correlates of objectively measured physical activity in Norwegian adults: a cross-sectional study. Journal of Sport and Health Science, 7(1), 19–26.
Wisløff, U., Støylen, A., Loennechen, J. P., Bruvold, M., Rognmo, Ø., Haram, P. M., et al. (2007). Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation, 115(24), 3086–3094.
Elliott, A. D., Rajopadhyaya, K., Bentley, D. J., Beltrame, J. F., & Aromataris, E. C. (2015). Interval training versus continuous exercise in patients with coronary artery disease: a meta-analysis. Heart, Lung & Circulation, 24, 149–157.
Strimbu, K., & Tavel, J. (2010). What are biomarkers? Current Opinion in HIV and AIDS, 5(6), 463–466.
Min, X., Lu, M., Tu, S., et al. (2017). Serum cytokine profile in relation to the severity of coronary artery disease. BioMed Research International, 2017, 4013685.
Bolignano, D., Cabassi, A., Fiaccadori, E., et al. (2014). Copeptin (CTproAVP), a new tool for understanding the role of vasopressin in pathophysiology. Clinical Chemistry and Laboratory Medicine, 52(10), 1447–1456.
Choi, H. J., Kim, M. C., Sim, D. S., Hong, Y. J., Kim, J. H., Jeong, M. H., et al. (2018). Serum copeptin levels predict clinical outcomes after successful percutaneous coronary intervention in patients with acute myocardial infarction. Annals of Laboratory Medicine, 38, 538–544.
Rolph, M. S., Zimmer, S., Bottazzi, B., Garlanda, C., Mantovani, A., & Hansson, G. K. (2002). Production of the long pentraxin PTX3 in advanced atherosclerotic plaques. Arteriosclerosis, Thrombosis, and Vascular Biology, 22(5), 10–14.
Ristagno, G., Fumagalli, F., Bottazzi, B., et al. (2019). Pentraxin 3 in cardiovascular disease. Frontiers in Immunology, 10, 823.
Felmeden, D. C., Spencer, C. G., Belgore, F. M., et al. (2003). Endothelial damage and angiogenesis in hypertensive patients: relationship to cardiovascular risk factors and risk factor management. American Journal of Hypertension, 16(1), 11–20.
Cao, R. Y., Zheng, H., Mi, Q., Li, Q., Yuan, W., Ding, Y., et al. (2018). Aerobic exercise-based cardiac rehabilitation in Chinese patients with coronary heart disease: study protocol for a pilot randomized controlled trial. Trials, 19, 363.
Gensini, G. G. (1983). A more meaningful scoring system for determining the severity of coronary heart disease. American Journal of Cardiology, 51, 606.
Andrikoula, M., & McDowell, I. F. W. (2008). The contribution of ApoB and ApoA1 measurements to cardiovascular risk assessment. Diabetes, Obesity & Metabolism, 10, 271–278.
Koch, B., Schaper, C., Ittermann, T., Spielhagen, T., Dorr, M., Volzke, H., et al. (2009). Reference values for cardiopulmonary exercise testing in healthy volunteers: the SHIP study. The European Respiratory Journal, 33, 389–397.
Tan, S. J. J., Allen, J. C., & Tan, S. Y. (2017). Determination of ideal target exercise heart rate for cardiac patients suitable for rehabilitation. Clinical Cardiology, 40, 1008–1012.
Sperling, M. P. R., Simoes, R. P., Caruso, F. C. R., et al. (2016). Is heart rate variability a feasible method to determine anaerobic threshold in progressive resistance exercise in coronary artery disease? Brazilian Journal of Physical Theraphy, 20, 289–297.
Jette, M., Sidney, K., & Blumchen, G. (1990). Metabolic equivalents (METS) in exercise testing, exercise prescription, and evaluation of functional capacity. Clinical Cardiology, 13, 555–565.
Thomas, R. J., King, M., Lui, K., et al. (2010). AACVPR/ACCF/AHA 2010 update: performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services endorsed by the American College of Chest Physicians, the American College of Sports Medicine, the American Physical Therapy Association, the Canadian Association of Cardiac Rehabilitation, the Clinical Exercise Physiology Association, the European Association for Cardiovascular Prevention and Rehabilitation, the Inter-American Heart Foundation, the National Association of Clinical Nurse Specialists, the Preventive Cardiovascular Nurses Association, and the Society of Thoracic Surgeons. Journal of the American College of Cardiology, 56, 1159–1167.
Piepoli, M. F., Corrà, U., Adamopoulos, S., et al. (2014). Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. European Journal of Preventive Cardiology, 21, 664–681.
Albouaini, K., Egred, M., Alahmar, A., & Wright, D. J. (2007). Cardiopulmonary exercise testing and its application. Heart, 93(10), 1285–1292.
Dyrstad, S. M., Edvardsen, E., Hansen, B. H., & Anderssen, S. A. (2019). Waist circumference thresholds and cardiorespiratory fitness. Journal of Sport and Health Science, 8(1), 17–22.
Conraads, V. M., Pattyn, N., Maeyer, C. D., et al. (2015). Aerobic interval training and continuous training equally improve aerobic exercise capacity in patients with coronary artery disease: the SAINTEX-CAD study. International Journal of Cardiology, 179, 203–210.
Amedro P, Gavotto A, Guillaumont S, et al. (2017). Cardiopulmonary fitness in children with congenital heart diseases versus healthy children. Heart, 0:1–11.
Goldhammer, E., Tanchilevitch, A., Maor, I., et al. (2005). Exercise training modulates cytokines activity in coronary heart disease patients. International Journal of Cardiology, 100(1), 93–99.
Kim, Y. J., Shin, Y. O., Bae, J. S., et al. (2008). Beneficial effects of cardiac rehabilitation and exercise after percutaneous coronary intervention on hsCRP and inflammatory cytokines in CAD patients. Pflügers Archiv, 455(6), 1081–1088.
Windsor, M. T., Bailey, T. G., Perissiou, M., et al. (2018). Cytokine responses to acute exercise in healthy older adults: the effect of cardiorespiratory fitness. Frontiers in Physiology, 9, 203.
Sandor, B., Nagy, A., Toth, A., et al. (2014). Effects of moderate aerobic exercise training on hemorheological and laboratory parameters in ischemic heart disease patients. PLoS One, 9(10), e110751.
Ferratini, M., Ripamonti, V., Masson, S., et al. (2012). Pentraxin-3 predicts functional recovery and 1-year major adverse cardiovascular events after rehabilitation of cardiac surgery patients. Journal of Cardiopulmonary Rehabilitation and Prevention, 32(1), 17–24.
Lee, B. C., Hsu, H. C., Tseng, W. Y., et al. (2009). Effect of cardiac rehabilitation on angiogenic cytokines in postinfarction patients. Heart, 95(12), 1012–1018.
Tu, W. J., Ma, G. Z., Ni, Y., et al. (2017). Copeptin and NT-proBNP for prediction of all-cause and cardiovascular death in ischemic stroke. Neurology, 88(20), 1899–1905.
Acknowledgments
The authors would like to express their gratitude to Dr. Qun Zhao from Shanghai Xuhui Central Hospital for his help with statistical analysis, Drs. Lingling Jiang and Wanqun Sun from Shanghai Xuhui Central Hospital, and Wenqin Gu from Shanghai Xuhui Fengling Community Healthcare Service Center for their generous contributions to the revision.
Funding
This work was supported by National Natural Science Foundation of China (grant number 81672260 for RYC); Shanghai Municipal Health Commission (grant numbers ZK2018A11 for HZ, ZK2018A10 and 201640194 for JY); and a hospital internal grant for JY.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human Subjects/Informed Consent Statement
Ethical approval was acquired from the Ethics Committee of Shanghai Xuhui Central Hospital (approval no. 2016-10) and registered on Chinese Clinical Trial Registry (ChiCTR-IPR-17010556). All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the World Medical Association (Declaration of Helsinki of 1975). Informed consent was obtained from each patient in the study.
Additional information
Editor-in-Chief Enrique Lara-Pezzi oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cao, R.Y., Zheng, H., Hong, Y. et al. Cardiac Rehabilitation with Targeted Intensity Improves Cardiopulmonary Functions Accompanying with Reduced Copeptin Level in Patients with Coronary Artery Disease. J. of Cardiovasc. Trans. Res. 14, 317–326 (2021). https://doi.org/10.1007/s12265-020-10055-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-10055-y