Abstract
Background
Financial toxicity (FT) refers to the adverse impact of cancer treatment costs on patients’ experiences, potentially leading to poor adherence to treatment and outcomes. However, the prevalence of FT among patients undergoing major upper gastrointestinal cancer operations, as well as factors associated with FT, remain unclear.
Methods
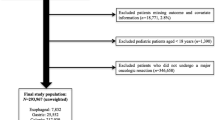
We conducted a cross-sectional study by sending the Comprehensive Score for financial Toxicity (COST) survey and Surgery-Q (a survey specifically developed for this study) to patients who underwent gastrectomy or pancreatectomy for malignant disease at our institution in 2019–2021.
Results
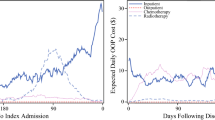
We sent the surveys to 627 patients and received responses from 101 (16%) patients. The FT prevalence (COST score <26) was 48 (48%). Patients likely to experience FT were younger than 50 years of age, of non-White race, earned an annual income <$75,000, and had credit scores <740 (all p < 0.05). Additionally, longer hospital stay (p = 0.041), extended time off work for surgery (p = 0.011), and extended time off work for caregivers (p = 0.005) were associated with FT. Procedure type was not associated with FT; however, patients who underwent minimally invasive surgery (MIS) had a lower FT probability (p = 0.042). In a multivariable analysis, age <50 years (p = 0.031) and credit score <740 (p < 0.001) were associated with high FT risk, while MIS was associated with low FT risk (p = 0.024).
Conclusions
Patients with upper gastrointestinal cancer have a major risk of FT. In addition to predicting the FT risk before surgery, facilitating quicker functional recovery with the appropriate use of MIS is considered important to reducing the FT risk.


Similar content being viewed by others
References
Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103(2):117–28.
Verma V, Sprave T, Haque W, et al. A systematic review of the cost and cost-effectiveness studies of immune checkpoint inhibitors. J Immunother Cancer. 2018;6(1):128.
Narang AK, Nicholas LH. Out-of-pocket spending and financial burden among medicare beneficiaries with cancer. JAMA Oncol. 2017;3(6):757–65.
Gilligan AM, Alberts DS, Roe DJ, Skrepnek GH. Death or debt? National estimates of financial toxicity in persons with newly-diagnosed cancer. Am J Med. 2018;131(10):1187-1199.e5.
Ghazal LV, Abrahamse P, Ward KC, Morris AM, Hawley ST, Veenstra CM. Financial toxicity and its association with health-related quality of life among partners of colorectal cancer survivors. JAMA Netw Open. 2023;6(4):e235897.
Zafar SY, Peppercorn JM, Schrag D, et al. The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist. 2013;18(4):381–90.
Ramsey S, Blough D, Kirchhoff A, et al. Washington state cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood). 2013;32(6):1143–52.
Tran G, Zafar SY. Financial toxicity and implications for cancer care in the era of molecular and immune therapies. Ann Transl Med. 2018;6(9):166.
Greenup RA, Rushing C, Fish L, et al. Financial costs and burden related to decisions for breast cancer surgery. J Oncol Pract. 2019;15(8):e666–76.
de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: the COST measure. Cancer. 2014;120(20):3245–53.
de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the comprehensive score for financial toxicity (COST). Cancer. 2017;123(3):476–84.
Jagsi R, Ward KC, Abrahamse PH, et al. Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer. 2018;124(18):3668–76.
Bullock AJ, Hofstatter EW, Yushak ML, Buss MK. Understanding patients’ attitudes toward communication about the cost of cancer care. J Oncol Pract. 2012;8(4):e50-58.
Huntington SF, Weiss BM, Vogl DT, et al. Financial toxicity in insured patients with multiple myeloma: a cross-sectional pilot study. The Lancet Haematology. 2015;2(10):e408–16.
Coroneos CJ, Lin YL, Sidey-Gibbons C, et al. Correlation between financial toxicity, quality of life, and patient satisfaction in an insured population of breast cancer surgical patients: a single-institution retrospective study. J Am Coll Surg. 2021;232(3):253–63.
Offodile AC 2nd, Asaad M, Boukovalas S, et al. Financial toxicity following surgical treatment for breast cancer: a cross-sectional pilot study. Ann Surg Oncol. 2021;28(5):2451–62.
Souza JAD, Wroblewski K, Proussaloglou E, Nicholson L, Hantel A, Wang Y. Validation of a financial toxicity (FT) grading system. J Clin Oncol. 2017;35(15 Suppl):6615–6615.
Farooq A, Merath K, Hyer JM, et al. Financial toxicity risk among adult patients undergoing cancer surgery in the United States: an analysis of the National Inpatient Sample. J Surg Oncol. 2019;120(3):397–406.
Deboever N, Eisenberg M, Hofstetter WL, et al. Financial toxicity in patients with resected lung cancer. Ann Surg. 2023;278(6):1038–44.
Ozman O, Tillier CN, van Muilekom E, van de Poll-Franse LV, van der Poel HG. Financial toxicity after robot-assisted radical prostatectomy and its relation with oncologic. Functional Outcomes J Urol. 2022;208(5):978–86.
Sharp L, O’Leary E, O’Ceilleachair A, Skally M, Hanly P. Financial impact of colorectal cancer and its consequences: associations between cancer-related financial stress and strain and health-related quality of life. Dis Colon Rectum. 2018;61(1):27–35.
Allen CJ, Yakoub D, Macedo FI, et al. Long-term quality of life and gastrointestinal functional outcomes after pancreaticoduodenectomy. Ann Surg. 2018;268(4):657–64.
McCall MD, Graham PJ, Bathe OF. Quality of life: a critical outcome for all surgical treatments of gastric cancer. World J Gastroenterol. 2016;22(3):1101–13.
Hirata Y, Chiang Y-J, Mansfield P, Badgwell BD, Ikoma N. Trends of oncological quality of robotic gastrectomy for gastric cancer in the United States. World Journal of Oncology. 2023;14(5):371–81.
Witt RG, Hirata Y, Prakash LR, et al. Comparative analysis of opioid use between robotic and open pancreatoduodenectomy. J Hepatobiliary Pancreat Sci. 2023;30(4):523–31.
Hirata Y, Witt RG, Prakash LR, et al. Analysis of opioid use in patients undergoing open versus robotic gastrectomy. Ann Surg Oncol. 2022;29(9):5861–70.
Hirata Y, Agnes A, Arvide EM, et al. Short-term and textbook surgical outcomes during the implementation of a robotic gastrectomy program. J Gastrointest Surg. 2023;27(6):1089–97.
Lee HJ, Hyung WJ, Yang HK, et al. Short-term outcomes of a multicenter randomized controlled trial comparing laparoscopic distal gastrectomy with D2 lymphadenectomy to open distal gastrectomy for locally advanced gastric cancer (KLASS-02-RCT). Ann Surg. 2019;270(6):983–91.
Hirata Y, Noorani A, Song S, Wang L, Ajani JA. Early stage gastric adenocarcinoma: clinical and molecular landscapes. Nat Rev Clin Oncol. 2023;20(7):453–69.
Kim HI, Han SU, Yang HK, et al. Multicenter prospective comparative study of robotic versus laparoscopic gastrectomy for gastric adenocarcinoma. Ann Surg. 2016;263(1):103–9.
Uyama I, Suda K, Nakauchi M, et al. Clinical advantages of robotic gastrectomy for clinical stage I/II gastric cancer: a multi-institutional prospective single-arm study. Gastric Cancer. 2019;22(2):377–85.
Acknowledgments
The authors thank Ann Sutton, Scientific Editor in the Research Medical Library at The University of Texas MD Anderson Cancer Center, for editing this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Yuki Hirata, Connie To, Heather Lyu, Grace L. Smith, Joyce P. Samuel, Hop S. Tran Cao, Brian D. Badgwell, Matthew H. G. Katz, and Naruhiko Ikoma have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hirata, Y., To, C., Lyu, H. et al. Prevalence of and Factors Associated with Financial Toxicity After Pancreatectomy and Gastrectomy. Ann Surg Oncol (2024). https://doi.org/10.1245/s10434-024-15236-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1245/s10434-024-15236-6