Key summary points
To assess the impact of combining lower-extremity muscle power training with regular cardiac rehabilitation on the muscle strength, balance function, and walking ability of older adults with heart failure
AbstractSection FindingsLower-extremity muscle power training was safely performed on older adults with heart failure. Dynamic balance and walking ability improved after regular cardiac rehabilitation, with added benefits observed when combined with lower-extremity muscle power training
AbstractSection MessageCombining lower-extremity muscle power training with regular cardiac rehabilitation further improves dynamic balance and walking ability in older adults with heart failure
Abstract
Purpose
This study investigated the combined effect of lower-extremity muscle power training and regular cardiac rehabilitation on muscle strength, balance function, and walking ability of older adults with heart failure.
Methods
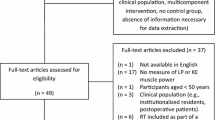
Thirty-one patients, comprising 17 males and 14 females, aged between 66 and 89 years and diagnosed with non-severe heart failure, were randomly assigned to either the intervention group (n = 15) or control group (n = 16). Both groups participated in a 12-week regular rehabilitation program, with the intervention group receiving additional lower-extremity muscle power training. Various outcome measures, including muscle strength (the five-times-sit-to-stand test and knee extensor peak torque), balance function (Berg balance scale and functional reach test), and walking ability (4-m walk and Timed Up-and-Go tests) were assessed at baseline and 12 weeks after the intervention.
Results
Of the 31 participants, 27 completed the study protocol. The intervention group demonstrated significantly greater improvement in the five-times-sit-to-stand test time, indicating enhanced lower-extremity muscle power compared to the control group. Both groups showed significant differences in the Berg balance scale, functional reach test, 4-m walk test, and Timed Up-and-Go test between baseline and 12 weeks. However, the effect sizes for the changes during the study period were larger in the intervention group (d = 0.74–1.19) than the control group (d = 0.57–0.96).
Conclusion
Combining lower-extremity muscle power training with regular cardiac rehabilitation may lead to additional improvements in muscle function for older adults with heart failure, resulting in enhanced dynamic balance and walking ability.
Trial registration number/date of registration
UMIN000032087/April 4, 2018.


Similar content being viewed by others
Data availability
All data used and analyzed to support the findings of this study are available from the corresponding author upon reasonable request.
References
Okura Y, Ramadan MM, Ohno Y, Mitsuma W, Tanaka K, Ito M et al (2008) Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J 72:489–491. https://doi.org/10.1253/circj.72.489
Marengoni A, Zucchelli A, Vetrano DL, Aloisi G, Brandi V, Ciutan M et al (2020) Heart failure, frailty, and pre-frailty: a systematic review and meta-analysis of observational studies. Int J Cardiol 316:161–171. https://doi.org/10.1016/j.ijcard.2020.04.043
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:146–156. https://doi.org/10.1093/gerona/56.3.m146
Matsue Y, Kamiya K, Saito H, Saito K, Ogasahara Y, Maekawa E et al (2020) Prevalence and prognostic impact of the coexistence of multiple frailty domains in elderly patients with heart failure: the FRAGILE-HF cohort study. Eur J Heart Fail 22:2112–2119. https://doi.org/10.1002/ejhf.1926
Vitale C, Jankowska E, Hill L, Piepoli M, Doehner W, Anker SD et al (2019) Heart Failure Association/European Society of Cardiology position paper on frailty in patients with heart failure. Eur J Heart Fail 21:1299–1305. https://doi.org/10.1002/ejhf.1611
Tschopp M, Sattelmayer MK, Hilfiker R (2011) Is power training or conventional resistance training better for function in elderly persons? A meta-analysis. Age Ageing 40:549–556. https://doi.org/10.1093/ageing/afr005
Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H et al (2021) International Exercise Recommendations in Older Adults (ICFSR): expert consensus guidelines. J Nutr Health Aging 25:824–853. https://doi.org/10.1007/s12603-021-1665-8
Häkkinen K, Kraemer WJ, Newton RU, Alen M (2001) Changes in electromyographic activity, muscle fibre and force production characteristics during heavy resistance/power strength training in middle-aged and older men and women. Acta Physiol Scand 171:51–62. https://doi.org/10.1046/j.1365-201X.2001.00781.x
Beijersbergen CMI, Granacher U, Gäbler M, Devita P, Hortobágyi T (2017) Power training-induced increases in muscle activation during gait in old adults. Med Sci Sports Exerc 49:2198–2025. https://doi.org/10.1249/MSS.0000000000001345
Lim FY, Yap J, Gao F, Teo LL, Lam CSP, Yeo KK (2018) Correlation of the New York Heart Association classification and the cardiopulmonary exercise test: a systematic review. Int J Cardiol 263:88–93. https://doi.org/10.1016/j.ijcard
Park J, Cho K, Lee W (2012) Effect of jumping exercise on muscle strength and balance of elderly people: a randomized controlled trial. J Phys Ther Sci 24:1345–1348. https://doi.org/10.1589/jpts.24.1345
Karvonen J, Vuorimaa T (1988) Heart rate and exercise intensity during sports activities. Practical application. Sports Med 5:303–311. https://doi.org/10.2165/00007256-198805050-00002
Goldberg A, Chavis M, Watkins J, Wilson T (2012) The five-times-sit-to-stand test: validity, reliability and detectable change in older females. Aging Clin Exp Res 24:339–44. https://doi.org/10.1007/BF03325265
Drouin JM, Valovich-mcLeod TC, Shultz SJ, Gansneder BM, Perrin DH (2004) Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol 91:22–29. https://doi.org/10.1007/s00421-003-0933-0
Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A (2002) Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci 57:M539-543. https://doi.org/10.1093/gerona/57.8.m539
Downs S (2015) The Berg Balance Scale. J Physiother 61:46. https://doi.org/10.1016/j.jphys.2014.10.002
Downs S, Marquez J, Chiarelli P (2013) The Berg Balance Scale has high intra- and inter-rater reliability but absolute reliability varies across the scale: a systematic review. J Physiother 59:93–99. https://doi.org/10.1016/S1836-9553(13)70161-9
Lajoie Y, Gallagher SP (2004) Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg balance scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr 38:11–26. https://doi.org/10.1016/s0167-4943(03)00082-7
Duncan PW, Weiner DK, Chandler J, Studenski S (1990) Functional reach: a new clinical measure of balance. J Gerontal 45:M 192-7. https://doi.org/10.1093/geronj/45.6.m192
Omana H, Bezaire K, Brady K, Davies J, Louwagie N, Power S et al (2021) Functional reach test, single-leg stance test, and tinetti performance-oriented mobility assessment for the prediction of falls in older adults: a systematic review. Phys Ther 101:173. https://doi.org/10.1093/ptj/pzab173
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG et al (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85-94. https://doi.org/10.1093/geronj/49.2.m85
Scott V, Votova K, Scanlan A, Close J (2007) Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing 36:130–139. https://doi.org/10.1093/ageing/afl165
Lee J, Geller AI, Strasser DC (2013) Analytical review: focus on fall screening assessments. PM R 5:609–621. https://doi.org/10.1016/j.pmrj
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Bonnefoy M, Kostka T, Arsac LM, Berthouze SE, Lacour JR (1998) Peak anaerobic power in elderly men. Eur J Appl Physiol Occup Physiol 77:182–188. https://doi.org/10.1007/s004210050318
Porter MM, Vandervoort AA, Lexell J (1995) Aging of human muscle: structure, function and adaptability. Scand J Med Sci Sports 5:129–142. https://doi.org/10.1111/j.1600-0838.1995.tb00026.x
Mc Dermott EJ, Balshaw TG, Brooke-Wavell K, Maden-Wilkinson TM, Folland JP (2022) Fast and ballistic contractions involve greater neuromuscular power production in older adults during resistance exercise. Eur J Appl Physiol 122:1639–1655. https://doi.org/10.1007/s00421-022-04947-x
Orr R, de Vos NJ, Singh NA, Ross DA, Stavrinos TM, Fiatarone-Singh MA (2006) Power training improves balance in healthy older adults. J Gerontol A Biol Sci Med Sci 61:78–85. https://doi.org/10.1093/gerona/61.1.78
Horak FB, Nashner LM (1986) Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol 55:1369–1381. https://doi.org/10.1152/jn.1986.55.6.1369
Pijnappels M, van der Burg PJ, Reeves ND, van Dieën JH (2008) Identification of elderly fallers by muscle strength measures. Eur J Appl Physiol 102:585–592. https://doi.org/10.1007/s00421-007-0613-6
Lopez P, Rech A, Petropoulou M, Newton RU, Taaffe DR, Galvão DA et al (2023) Does high-velocity resistance exercise elicit greater physical function benefits than traditional resistance exercise in older adults? A systematic review and network meta-analysis of 79 trials. J Gerontol A Biol Sci Med Sci 78:1471–1482. https://doi.org/10.1093/gerona/glac230
Katsura Y, Takeda N, Hara T, Takahashi S, Nosaka K (2019) Comparison between eccentric and concentric resistance exercise training without equipment for changes in muscle strength and functional fitness of older adults. Eur J Appl Physiol 119:1581–1590. https://doi.org/10.1007/s00421-019-04147-0
Lee HC, Lee ML, Kim SR (2015) Effect of exercise performance by elderly women on balance ability and muscle function. J Phys Ther Sci 27:989–992. https://doi.org/10.1589/jpts.27.989
Krebs DE, Scarborough DM, McGibbon CA (2007) Functional vs. strength training in disabled elderly outpatients. Am J Phys Med Rehabil 86:93–103. https://doi.org/10.1097/PHM.0b013e31802ede64
Brodie MA, Coppens MJ, Ejupi A, Gschwind YJ, Annegarn J, Schoene D et al (2017) Comparison between clinical gait and daily-life gait assessments of fall risk in older people. Geriatr Gerontol Int 17:2274–2282. https://doi.org/10.1111/ggi.12979
Mulasso A, Roppolo M, Gobbens RJ, Rabaglietti E (2017) Mobility, balance and frailty in community-dwelling older adults: what is the best 1-year predictor of falls? Geriatr Gerontol Int 17:1463–1469. https://doi.org/10.1111/ggi.12893
Yoshiko A, Kaji T, Sugiyama H, Koike T, Oshida Y, Akima H (2017) Effect of 12-month resistance and endurance training on quality, quantity, and function of skeletal muscle in older adults requiring long-term care. Exp Gerontol 98:230–237. https://doi.org/10.1016/j.exger.2017.08.036
Borowicz A, Zasadzka E, Gaczkowska A, Gawłowska O, Pawlaczyk M (2016) Assessing gait and balance impairment in elderly residents of nursing homes. J Phys Ther Sci 28:2486–2490. https://doi.org/10.1589/jpts.28.2486
Beck Jepsen D, Robinson K, Ogliari G, Montero-Odasso M, Kamkar N, Ryg J et al (2022) Predicting falls in older adults: an umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatr 22:615. https://doi.org/10.1186/s12877-022-03271-5
Papa EV, Dong X, Hassan M (2017) Resistance training for activity limitations in older adults with skeletal muscle function deficits: a systematic review. Clin Interv Aging 12:955–961. https://doi.org/10.2147/CIA.S104674
Schoenfeld BJ, Ogborn D, Krieger JW (2016) Effects of resistance training frequency on measures of muscle hypertrophy: a systematic review and meta-analysis. Sports Med 46:1689–1697. https://doi.org/10.1007/s40279-016-0543-8
Farris DJ, Sawicki GS (2012) Human medial gastrocnemius force-velocity behavior shifts with locomotion speed and gait. Proc Natl Acad Sci USA 109:977–82. https://doi.org/10.1073/pnas.1107972109
Espejo-Antúnez L, Pérez-Mármol JM, Cardero-Durán MLÁ, Toledo-Marhuenda JV, Albornoz-Cabello M (2020) The effect of proprioceptive exercises on balance and physical function in institutionalized older adults: a randomized controlled trial. Arch Phys Med Rehabil 101:1780–1788. https://doi.org/10.1016/j.apmr.2020.06.010
Oh DS, Choi JD (2021) Effects of motor imagery training on balance and gait in older adults: a randomized controlled pilot study. Int J Environ Res Public Health 18:650. https://doi.org/10.3390/ijerph18020
Acknowledgements
We would like to express our gratitude to the study participants. We would also like to thank Kamijo Y, Uenishi H, and all staff members at Sumiya Rehabilitation Hospital for their kind support.
Funding
The authors received no financial support for the research.
Author information
Authors and Affiliations
Contributions
MS conceived the study design, data collection, statistical analysis, and interpretation and drafted the manuscript. NM contributed to statistical analysis, interpretation, drafting, and final revision of the manuscript. HK contributed to data collection and interpretation. MA contributed to the conception and design of the study, drafting, and final revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
This study was conducted in accordance with the principles of the Declaration of Helsinki. Approval was granted by the ethics board of Wakayama Medical University (approval no. 2295).
Informed consent
All participants signed an informed consent form after the objectives of the study and experimental procedures were explained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakaguchi, M., Miyai, N., Kobayashi, H. et al. Effect of lower-extremity muscle power training on muscle strength, balance function and walking ability in older adults with heart failure: a randomized controlled trial. Eur Geriatr Med 15, 361–370 (2024). https://doi.org/10.1007/s41999-023-00905-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-023-00905-8