Abstract
Purpose
Patients with hereditary hypophosphatemic rickets are short and disproportionate and very little information is available on segmental growth, but the body disproportion at adulthood leads us to think that the growth velocity of legs is slower.
Methods
A total of 96 children were included and molecular testing was carried out in 42. Children who reached adult height were classified into two groups according to their compliance to conventional treatment (phosphate supplement and calcitriol). Individual growth records of height and sitting height/height were plotted using Argentine reference data in 96 children and growth curves were estimated by fitting Preece-Baines Model 1 in 19 of the children.
Results
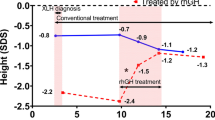
Molecular testing revealed sequence deleterious alterations or large deletions in 36/42 patients. During childhood, 76% of children grew below − 1.88 standard deviation score (SDS) and 97% had body disproportion. During adolescence, the mean peak height velocity for the good and poor compliance to treatment groups was 7.8 (0.6) and 5.4 (0.4) cm/year in boys and 7.0 (0.7) and 5.2 (0.8) cm/year in girls, respectively. At adulthood, the median sitting height/height ratio was 2.32 and 6.21 SDS for the good and poor compliance to treatment groups, respectively. The mean pubertal growth spurt of the trunk was –0.8 (1.4) SDS, with a short pubertal growth spurt of − 1.8 (0.4) SDS for limbs in the good compliance group. Median adult height in 13/29 males and 30/67 females was –4.56 and –3.16 SDS, respectively.
Conclusion
For all patients the growth spurt was slower, secondary to a short growth spurt of limbs, reaching a short adult height with body disproportion that was more prominent in the poor compliance group.



Similar content being viewed by others
Data availability statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
KaleidaGraph 4.5.3 for Microsoft Windows. Copyright by Sinergy software. Serial no. 9009089.
References
Capelli S, Donghi V, Maruca K, Vezzoli G, Corbetta S, Brandi ML, Mora S, Weber G (2015) Clinical and molecular heterogeneity in a large series of patients with hypophosphatemic rickets. Bone 79(143–149):12. https://doi.org/10.1016/j.bone.2015.05.040
Razali NN, Hwu TT, Thilakavathy K (2015) Phosphate homeostasis and genetic mutations of familial hypophosphatemic rickets. J Pediatr Endocrinol Metab JPEM 28(9–10):1009–1017. https://doi.org/10.1515/jpem-2014-0366
Bastepe M, Jüppner H (2008) Inherited hypophosphatemic disorders in children and the evolving mechanisms of phosphate regulation. Rev Endocr Metab Disord 9(2):171–180. https://doi.org/10.1007/s11154-008-9075-3
Glorieux FH, Pettifor JM, Jüppner H (2012) Pediatric Bone. Biology and diseases. Academic Press, USA
Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL (2011) A clinician’s guide to X-linked hypophosphatemia. J Bone Min Res Off J Am Soc Bone Min Res 26(7):1381–1388. https://doi.org/10.1002/jbmr.340
Linglart A, Biosse-Duplan M, Briot K, Chaussain C, Esterle L, Guillaume-Czitrom S, Kamenicky P, Nevoux J, Prié D, Rothenbuhler A, Wicart P, Harvengt P (2014) Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr Connect 3(1):R13–R30. https://doi.org/10.1530/EC-13-0103
Imel EA, Carpenter TO (2015) A practical clinical approach to paediatric phosphate disorders. Endocr Dev 28:134–161. https://doi.org/10.1159/000381036
Rafaelsen S, Johansson S, Ræder H, Bjerknes R (2016) Hereditary hypophosphatemia in Norway: a retrospective population-based study of genotypes, phenotypes, and treatment complications. Eur J Endocrinol 174(2):125–136. https://doi.org/10.1530/EJE-15-0515
Courbebaisse M, Lanske B (2018) Biology of fibroblast growth factor 23: from physiology to pathology. Cold Spring Harb Perspect Med 8(5):a031260. https://doi.org/10.1101/cshperspect.a031260
- Arenas, Maria; Jaimovich, Sebastian; Perez Garrido, Natalia; del Pino, Mariana; Viterbo, Gisela; Marino, Roxana;and Fano, Virginia; Hereditary Hypophosphatemic Rickets and Craniosynostosis https://doi.org/10.1515/jpem-2021-0042
Carpenter TO, Whyte MP, Imel EA, Boot AM, Högler W, Linglart A, Padidela R, Van’t Hoff W, Mao M, Chen CY, Skrinar A, Kakkis E, San Martin J, Portale AA (2018) Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med 378(21):1987–1998. https://doi.org/10.1056/NEJMoa1714641
Imel EA, Glorieux FH, Whyte MP et al (2019) Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet (London, England) 393(10189):2416–2427. https://doi.org/10.1016/S0140-6736(19)30654-3
Mao M, Carpenter TO, Whyte MP, Skrinar A, Chen CY, San Martin J, Rogol AD (2020) Growth curves for children with X-linked hypophosphatemia. J Clin Endocrinol Metab 105(10):495. https://doi.org/10.1210/clinem/dgaa495
Fano V, del Pino M, Caletti MG, Delgado A, Turconi A, Mendilaharzu H, Lejarraga H (2008) Crecimiento a largo plazo de pacientes con raquitismo hipofosfatémico familiar (RHF). Med Infantil XV:243–247
Santos F, Fuente R, Mejia N, Mantecon L, Gil-Peña H, Ordoñez FA (2013) Hypophosphatemia and growth. Pediatr Nephrol (Berl, Germany) 28(4):595–603. https://doi.org/10.1007/s00467-012-2364-9
Zivičnjak M, Schnabel D, Billing H, Staude H, Filler G, Querfeld U, Schumacher M, Pyper A, Schröder C, Brämswig J, Haffner D (2011) Age-related stature and linear body segments in children with X-linked hypophosphatemic rickets. Pediatr Nephrol (Berl, Germany) 26(2):223–231. https://doi.org/10.1007/s00467-010-1705-9
Beck-Nielsen SS, Brusgaard K, Rasmussen LM, Brixen K, Brock-Jacobsen B, Poulsen MR, Vestergaard P, Ralston SH, Albagha OM, Poulsen S, Haubek D, Gjørup H, Hintze H, Andersen MG, Heickendorff L, Hjelmborg J, Gram J (2010) Phenotype presentation of hypophosphatemic rickets in adults. Calcif Tissue Int 87(2):108–119. https://doi.org/10.1007/s00223-010-9373-0
Steendijk R, Herweijer TJ (1984) Height, sitting height and leg length in patients with hypophosphataemic rickets. Acta Paediatr Scand 73(2):181–184. https://doi.org/10.1111/j.1651-2227.1984.tb09925.x
Steendijk R, Hauspie RC (1992) The pattern of growth and growth retardation of patients with hypophosphataemic vitamin D-resistant rickets: a longitudinal study. Eur J Pediatr 151(6):422–427. https://doi.org/10.1007/BF01959355
Mäkitie O, Doria A, Kooh SW, Cole WG, Daneman A, Sochett E (2003) Early treatment improves growth and biochemical and radiographic outcome in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab 88(8):3591–3597. https://doi.org/10.1210/jc.2003-030036
Morey M, Castro-Feijóo L, Barreiro J, Cabanas P, Pombo M, Gil M, Bernabeu I, Díaz-Grande JM, Rey-Cordo L, Ariceta G, Rica I, Nieto J, Vilalta R, Martorell L, Vila-Cots J, Aleixandre F, Fontalba A, Soriano-Guillén L, García- Sagredo JM, García-Miñaur S, Loidi L (2011) Genetic diagnosis of X-linked dominant Hypophosphatemic Rickets in a cohort study: tubular reabsorption of phosphate and 1,25(OH)2D serum levels are associated with PHEX mutation type. BMC Med Genet 12:116. https://doi.org/10.1186/1471-2350-12-116
Holm IA, Nelson AE, Robinson BG, Mason RS, Marsh DJ, Cowell CT, Carpenter TO (2001) Mutational analysis and genotype-phenotype correlation of the PHEX gene in X-linked hypophosphatemic rickets. J Clin Endocrinol Metab 86(8):3889–3899. https://doi.org/10.1210/jcem.86.8.7761
del Pino M, Viterbo GL, Fano V (2017) GAP2017 Manejo de Niños con Raquitismo Hipofosfatémico Familiar. http://garrahan.gov.ar/images/intranet/guias_atencion/GAP_2017_-_MANEJO_RAQUITISMO.pdf. Accessed 26 Dec 2020
Lejarraga H, Heinrich JJ, Rodríguez A (1975) Normas y técnicas de mediciones antropométricas. Rev del Hosp de Niños 17:165–171
Caíno S, Adamo P, Kelmansky D, Lejarraga H (2002) Impacto del entrenamiento sobre el error de mediciones antropométricas. Arch Arg Ped 100:110–113
Lejarraga H, del Pino M, Fano V, Caino S, Cole TJ (2009) Referencias de peso y estatura desde el nacimiento hasta la madurez para niñas y niños argentinos: Incorporación de datos de la OMS de 0 a 2 años, recálculo de percentilos para obtención de valores LMS [Growth references for weight and height for Argentinian girls and boys from birth to maturity: incorporation of data from the World Health Organization from birth to 2 years and calculation of new percentiles and LMS values]. Arch Argent de Pediatr 107(2):126–133. https://doi.org/10.1590/S0325-00752009000200006
del Pino M, Orden AB, Arenas MA, Fano V (2017) Argentine references for the assessment of body proportions from birth to 17 years of age Referencias argentinas para la evaluación de proporciones corporales desde el nacimiento hasta los 17 años. Arch Argent de Pediatr 115(3):234–240. https://doi.org/10.5546/aap.2017.eng.234
Thacher TD, Fischer PR, Pettifor JM, Lawson JO, Manaster BJ, Reading JC (2000) Radiographic scoring method for the assessment of the severity of nutritional rickets. J Trop Pediatr 46(3):132–139. https://doi.org/10.1093/tropej/46.3.132
Preece MA, Baines MJ (1978) A new family of mathematical models describing the human growth curve. Ann Hum Biol 5(1):1–24. https://doi.org/10.1080/03014467800002601
Marshall WA, Tanner JM (1970) Variations in the pattern of pubertal changes in boys. Arch Dis Child 45(239):13–23. https://doi.org/10.1136/adc.45.239.13
Tanner JM (1973) Growth at adolescence. Blackwell Scientific Publications, Oxford
Marshall WA, Tanner JM (1969) Variations in pattern of pubertal changes in girls. Arch Dis Child 44(235):291–303. https://doi.org/10.1136/adc.44.235.291
Rowe PS, Oudet CL, Francis F, Sinding C, Pannetier S, Econs MJ, Strom TM, Meitinger T, Garabedian M, David A, Macher MA, Questiaux E, Popowska E, Pronicka E, Read AP, Mokrzycki A, Glorieux FH, Drezner MK, Hanauer A, Lehrach H, O’Riordan JL (1997) Distribution of mutations in the PEX gene in families with X-linked hypophosphataemic rickets (HYP). Hum Mol Genet 6(4):539–549. https://doi.org/10.1093/hmg/6.4.539
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, Laboratory Quality Assurance Committee ACMG (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med Off J Am Coll Med Genet 17(5):405–424. https://doi.org/10.1038/gim.2015.30
Hauspie RC, Cameron N, Molinari L (2004) Methods in human growth research. University Press, United Kingdom
Lejarraga H, Cusminsky M, Castro EP (1976) Age of onset of puberty in urban Argentinian children. Ann Hum Biol 3(4):379–381. https://doi.org/10.1080/03014467600001601
Orden AB, Vericat A, Apezteguía MC (2011) Age at menarche in urban Argentinian girls: association with biological and socioeconomic factors. Nthropologischer Anzeiger Bericht uber die biologisch anthropologische Literatur 68(3):309–322. https://doi.org/10.1127/0003-5548/2011/0109
Tanner JM, Whitehouse RH, Marubini E, Resele LF (1976) The adolescent growth spurt of boys and girls of the Harpenden Growth Study. Ann Hum Biol 3(2):109–126. https://doi.org/10.1080/03014467600001231
del Pino M, Orden AB, Arenas MA, Caíno S, Fano V (2016) Referencias argentinas de estatura sentada y longitud de miembros inferiores de 0 a 18 años. Med Infant XXXIII(4):279–286
Kinoshita Y, Saito T, Shimizu Y, Hori M, Taguchi M, Igarashi T, Fukumoto S, Fujita T (2012) Mutational analysis of patients with FGF23-related hypophosphatemic rickets. Eur J Endocrinol 167(2):165–172. https://doi.org/10.1530/EJE-12-0071
Acknowledgements
We thank Ronald Hauspie (deceased), who taught and trained us in mathematical models to analyze longitudinal growth data, and also thank the patients and their families.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the study conception and design. Material preparation, data collection and analysis was performed by MdP, GLV and MAA. The first draft of the manuscript was written by MdP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Research involving human participants and/or animals
This was a retrospective cohort study conducted in conformity with the World Medical Association and the Declaration of Helsinki for medical research involving human subjects. The study protocol was approved by the Research Review Committee and Ethics Review Committee from Garrahan Pediatric Hospital.
Informed consent
For this type of study formal consent is not required.
Consent to participate
Not applicable.
Consent for publication
All authors approved the publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
del Pino, M., Viterbo, G.L., Arenas, M.A. et al. Growth in height and body proportion from birth to adulthood in hereditary hypophosphatemic rickets: a retrospective cohort study. J Endocrinol Invest 45, 1349–1358 (2022). https://doi.org/10.1007/s40618-022-01768-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01768-9