Abstract
Objective
ComPsych communication skills training is designed to teach psychiatry trainees effective skills and strategies for undertaking key communication tasks relating to mental illness, such as schizophrenia, with patients and their families/carers. This study examined the program’s feasibility, utility, and trainees’ self-efficacy.
Methods
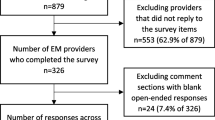
Trainee cohorts attending their first year formal education course were recruited annually over 4 years between 2015 and 2018. Each trainee attended at least one session of training in their cohort year. Trainees completed a questionnaire presenting questions about personal demographics, their perceived confidence in communication, and the effectiveness of elements of training delivery. A total of 41 trainee psychiatrists (15 male) completed the questionnaires presented at four time points (two pre-training and two post-training).
Results
Participants reported a significant increase in confidence in their own communication skills post-training (d = 1.12) and rated elements of training delivery (video feedback, feedback from peers in small groups, small group facilitation, and use of simulated patients) as significantly more helpful or effective post-training (d = 0.42). Trainees also reported a significantly increased ability to critically evaluate their own communication skills post-training (d = 0.59), suggesting an increased ability to recognize their own communication skill competence.
Conclusions
Following ComPsych training, trainees were more confident discussing information about schizophrenia with patients and their families/carers and were more able to critically evaluate their own communication skills: an important feature of good clinical acumen. These subjective ratings provide important self-efficacy information, including the benefits perceived and evidence of the program’s feasibility and utility.

Similar content being viewed by others
References
Priebe S, Dimic S, Wildgrube C, Jankovic J, Cushing A, McCabe R. Good communication in psychiatry–a conceptual review. Eur Psychiatry. 2011;26(7):403–7.
Loughland C, Cheng K, Harris G, Kelly B, Cohen M, Sandhu H, et al. Communication of a schizophrenia diagnosis: a qualitative study of patients' perspectives. Int J Soc Psychiatry. 2015;61(8):729–34.
Outram S, Harris G, Kelly B, Cohen M, Sandhu H, Vamos M, et al. Communicating a schizophrenia diagnosis to patients and families: a qualitative study of mental health clinicians. Psychiatr Serv. 2014;65(4):551–4.
Outram S, Harris G, Kelly B, Cohen M, Bylund CL, Landa Y, et al. Contextual barriers to discussing a schizophrenia diagnosis with patients and families: need for leadership and teamwork training in psychiatry. Acad Psychiatry. 2015;39(2):174–80.
Outram S, Harris G, Kelly B, Bylund CL, Cohen M, Landa Y, et al. “We didn’t have a clue”: Family caregivers’ experiences of the communication of a diagnosis of schizophrenia. Int J Soc Psychiatry. 2015;61(1):10–6.
Angermeyer MC, Schulze B. Reducing the stigma of schizophrenia: understanding the process and options for interventions. Epidemiol Psichiatr Soc. 2001;10(1):1–5.
Ditton-Phare P, Loughland C, Duvivier R, Kelly B. Communication skills in the training of psychiatrists: a systematic review of current approaches. Aust N Z J Psychiatry. 2017;51(7):675–92.
Ditton-Phare P, Halpin S, Sandhu H, Kelly B, Vamos M, Outram S, et al. Communication skills in psychiatry training. Australas Psychiatry. 2015;23(4):429–31.
Ditton-Phare P, Sandhu H, Kelly B, Kissane D, Loughland C. Pilot evaluation of a communication skills training program for psychiatry residents using standardized patient assessment. Acad Psychiatry. 2016;40(5):768–75.
Loughland C, Kelly B, Ditton-Phare P, Sandhu H, Vamos M, Outram S, et al. Improving clinician competency in communication about schizophrenia: a pilot educational program for psychiatry trainees. Acad Psychiatry. 2015;39(2):160–4.
Cohen M, Llewellyn A, Ditton-Phare P, Sandhu H, Vamos M. Hunter New England Training (HNET): how to effect culture change in a psychiatry medical workforce. Australas Psychiatry. 2011;19(6):531–4.
Levin TT, Kelly BJ, Cohen M, Vamos M, Landa Y, Bylund CL. Case studies in public-sector leadership: using a psychiatry e-list to develop a model for discussing a schizophrenia diagnosis. Psychiatr Serv. 2011;62(3):244–6.
Loughland C, Ditton-Phare P, Kissane DW. Communication and relational skills in medicine. Person centered approach to recovery in medicine. Insights from psychosomatic medicine and consultation-liaison psychiatry: Springer International Publishing AG, part of Springer Nature; 2019;163–76.
Bylund CL, Brown R, Gueguen JA, Diamond C, Bianculli J, Kissane DW. The implementation and assessment of a comprehensive communication skills training curriculum for oncologists. Psychooncology. 2010;19(6):583–93.
Warner R. Recovery from schizophrenia and the recovery model. Curr Opin Psychiatry. 2009;22(4):374–80.
Whitney SN, McCullough LB, Fruge E, McGuire AL, Volk RJ. Beyond breaking bad news: the roles of hope and hopefulness. Cancer. 2008;113(2):442–5.
Bylund CL, Peterson EB, Cameron KA. A practitioner’s guide to interpersonal communication theory: an overview and exploration of selected theories. Patient Educ Couns. 2012;87(3):261–7.
Kiely BE, Tattersall MH, Stockler MR. Certain death in uncertain time: informing hope by quantifying a best case scenario. J Clin Oncol. 2010;28(16):2802–4.
Kiely BE, Soon YY, Tattersall MH, Stockler MR. How long have I got? Estimating typical, best-case, and worst-case scenarios for patients starting first-line chemotherapy for metastatic breast cancer: a systematic review of recent randomized trials. J Clin Oncol. 2011;29(4):456–63.
Tattersall MH. Clinical perspectives on shared decision-making. In: Kissane DW, Bultz BD, Butow P, Finlay I, editors. Handbook of communication in oncology and palliative care. Oxford: Oxford University Press; 2010. p. 339–50.
Kissane DW. Communication training to achieve shared decision making. In: Kissane DW, Bultz BD, Butow P, Finlay I, editors. Handbook of communication in oncology and palliative care. Oxford: Oxford University Press; 2010. p. 127–34.
Coyle N, Kissane DW. Conducting a family meeting. In: Kissane DW, Bultz BD, Butow PM, Finaly IG, editors. Handbook of communication in oncology and palliative care. New York: Oxford University Press; 2010. p. 165–75.
Gueguen JA, Bylund CL, Brown RF, Levin TT, Kissane DW. Conducting family meetings in palliative care: themes, techniques, and preliminary evaluation of a communication skills module. Palliat Support Care. 2009;7(2):171–9.
Crum A, Zuckerman B. Changing mindsets to enhance treatment effectiveness. JAMA. 2017;317(20):2063–4.
IBM Corp. IBM SPSS statistics for windows, version 25.0. Armonk, NY: IBM Corp.; 2017.
Kolb DA. Experiential learning: experience as the source of learning and development. Pearson Education; 2014.
Hodges B, Regehr G, Martin D. Difficulties in recognizing one’s own incompetence: novice physicians who are unskilled and unaware of it. Acad Med. 2001;76(10 Suppl):S87–9.
Acknowledgements
This study was conducted by a PhD student from the University of Newcastle, in conjunction with the student’s supervisors. We would like to thank HNET Psychiatry trainees for participating in this study. Thanks to Kerrin Palazzi at HMRI Clinical Research Design and Statistical Services for statistical assistance.
Funding
This research was supported by an Australian Government Research Training Program (RTP) Scholarship and additional grant assistance from the Centre for Brain and Mental Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Disclaimer
The funding body of the student’s PhD played no role in study design, collection, analysis, interpretation of data, writing the report, or in the decision to submit the paper for publication. They accept no responsibility for the contents.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ditton-Phare, P., Sandhu, H., Kelly, B. et al. Does ComPsych Communication Skills Training Alter Trainee Self-Efficacy?. Acad Psychiatry 46, 303–310 (2022). https://doi.org/10.1007/s40596-021-01517-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40596-021-01517-9