Abstract
Introduction
Swallowing impairment (SI) is an underdiagnosed dysfunction frequently seen as an expected condition of aging. However, SI can lead to health complications and considerable social impact.
Methods
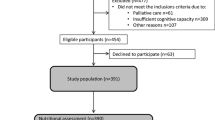
The objective of this systematic review with meta-analysis was to evaluate the frequency and associated factors with SI in community-dwelling older persons. Searches were performed in 13 electronic databases including MEDLINE and EMBASE (from inception to September 18, 2021). Data extraction and methodological quality assessment of included studies were performed by two independent reviewers. Meta-analysis of proportions with 95% confidence interval (CI) and prediction interval (PI) was used to pool estimates. Subgroup analysis by Country and Assessment Method was performed. General meta-analysis was used to pool measures of association between potential risk factors and SI occurrence (odds ratio [OR] or prevalence ratio [PR]).
Results
The worldwide estimated frequency of SI in community-dwelling older persons was 20.35% (95%CI 16.61–24.68%, 95%PI 4.79–56.45, I2 99%, n = 33,291). This estimation varied across assessment methods and by country. The main factors associated with SI were a dry mouth (OR 8.1, 95%CI 4.9–13.4), oral diadochokinesis (OR 5.3, 95%CI 1.0–27.3), ≥ 80 years old (OR 4.9, 95%CI 2.6–9.2), genetic factor (SNPrs17601696) (OR 4.8, 95%CI 2.7–8.3), and partial dependence (OR 4.3, 95%CI 2.0–9.3). And the main factors associated with SI estimated by PR were dry mouth sensation (PR 4.1, 95%CI 2.6–6.5), oral sensorimotor alteration (PR 2.6, 95%CI 1.4–4.9), osteoporosis (PR 2.51, 95%CI 1.2–5.3), and heart diseases (PR 2.31, 95%CI 1.1–5.0).
Conclusion
One in five older adults worldwide are expected to experience SI and factors associated with this underdiagnosed dysfunction included biological and physiological changes related to aging, physical and psychological conditions, and poor oral health. Early assessment is paramount for the prevention of future clinical complications and should be a high priority in health care practices.




Similar content being viewed by others
References
Kyu HH, Abate D, Abate KH et al (2018) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1859–1922. https://doi.org/10.1016/S0140-6736(18)32335-3
Rommel N, Hamdy S (2016) Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol 13:49–59. https://doi.org/10.1038/nrgastro.2015.199
Mann T, Heuberger R, Wong H (2013) The association between chewing and swallowing difficulties and nutritional status in older adults. Aust Dent J 58:200–206. https://doi.org/10.1111/adj.12064
Rech RS, Baumgarten A, Colvara BC et al (2018) Association between oropharyngeal dysphagia, oral functionality, and oral sensorimotor alteration. Oral Dis 24:664–672. https://doi.org/10.1111/odi.12809
Rofes L, Arreola V, Almirall J et al (2011) Diagnosis and management of oropharyngeal Dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract 2011:818979. https://doi.org/10.1155/2011/818979
Audag N, Goubau C, Toussaint M et al (2019) Screening and evaluation tools of dysphagia in adults with neuromuscular diseases: a systematic review. Ther Adv Chronic Dis 10:2040622318821622. https://doi.org/10.1177/2040622318821622
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Munn Z, Moola S, Lisy K et al (2015) Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 13:147–153. https://doi.org/10.1097/xeb.0000000000000054
Barendregt JJ, Doi SA, Lee YY et al (2013) Meta-analysis of prevalence. J Epidemiol Community Health 67:974–978. https://doi.org/10.1136/jech-2013-203104
IntHout J, Ioannidis JP, Rovers MM et al (2016) Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 6:e010247. https://doi.org/10.1136/bmjopen-2015-010247
Borges Migliavaca C, Stein C, Colpani V et al (2020) How are systematic reviews of prevalence conducted? A methodological study. BMC Med Res Methodol 20:96. https://doi.org/10.1186/s12874-020-00975-3
Balduzzi S, Rücker G, Schwarzer G (2019) How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 22:153–160. https://doi.org/10.1136/ebmental-2019-300117
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36:1–48
Team RC (2013) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Inui A, Takahashi I, Kurauchi S et al (2017) Oral conditions and dysphagia in Japanese, community-dwelling middle- and older- aged adults, independent in daily living. Clin Interv Aging 12:515–521. https://doi.org/10.2147/cia.S132637
Chen MY, Lin LC (2012) Nonimaging clinical assessment of impaired swallowing in community-dwelling older adults in Taiwan. J Nurs Res 20:272–280. https://doi.org/10.1097/jnr.0b013e31827364ec
Raginis-Zborowska A, Mekli K, Payton A et al (2015) Genetic determinants of swallowing impairments among community dwelling older population. Exp Gerontol 69:196–201. https://doi.org/10.1016/j.exger.2015.06.014
Roy N, Stemple J, Merrill RM et al (2007) Dysphagia in the elderly: preliminary evidence of prevalence, risk factors, and socioemotional effects. Ann Otol Rhinol Laryngol 116:858–865. https://doi.org/10.1177/000348940711601112
Byeon H (2016) Analysis of dysphagia risk using the modified dysphagia risk assessment for the community-dwelling elderly. J Phys Ther Sci 28:2507–2509. https://doi.org/10.1589/jpts.28.2507
Mourão LF, Xavier DAN, Neri AL et al (2016) Association study between natural chronic diseases of aging and swallowing changes referred by community elderly. Audiol Commun Res. https://doi.org/10.1590/2317-6431-2015-1657
Yang EJ, Kim KW, Lim JY et al (2014) Relationship between dysphagia and mild cognitive impairment in a community-based elderly cohort: the Korean longitudinal study on health and aging. J Am Geriatr Soc 62:40–46. https://doi.org/10.1111/jgs.12606
Okamoto N, Tomioka K, Saeki K et al (2012) Relationship between swallowing problems and tooth loss in community-dwelling independent elderly adults: the Fujiwara-kyo study. J Am Geriatr Soc 60:849–853. https://doi.org/10.1111/j.1532-5415.2012.03935.x
Cha S, Kim WS, Kim KW et al (2019) Sarcopenia is an independent risk factor for dysphagia in community-dwelling older adults. Dysphagia 34:692–697. https://doi.org/10.1007/s00455-018-09973-6
Bahat G, Yilmaz O, Durmazoglu S et al (2019) Association between dysphagia and frailty in community dwelling older adults. J Nutr Health Aging 23:571–577. https://doi.org/10.1007/s12603-019-1191-0
Nishida T, Yamabe K, Honda S (2020) Dysphagia is associated with oral, physical, cognitive and psychological frailty in Japanese community-dwelling elderly persons. Gerodontology 37:185–190. https://doi.org/10.1111/ger.12455
Nishida T, Yamabe K, Ide Y et al (2020) Utility of the Eating Assessment Tool-10 (EAT-10) in evaluating self-reported dysphagia associated with oral frailty in Japanese community-dwelling older people. J Nutr Health Aging 24:3–8. https://doi.org/10.1007/s12603-019-1256-0
Mulheren RW, Azola AM, Kwiatkowski S et al (2018) Swallowing changes in community-dwelling older adults. Dysphagia 33:848–856. https://doi.org/10.1007/s00455-018-9911-x
Park S (2015) Dysphagia risk and associated factors among community-dwelling elders. J Korean Soc Food Sci Nutr 44:49–56
Kawashima K, Motohashi Y, Fujishima I (2004) Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia 19:266–271. https://doi.org/10.1007/s00455-004-0013-6
Chen PH, Golub JS, Hapner ER et al (2009) Prevalence of perceived dysphagia and quality-of-life impairment in a geriatric population. Dysphagia 24:1–6. https://doi.org/10.1007/s00455-008-9156-1
González-Fernández M, Humbert I, Winegrad H et al (2014) Dysphagia in old-old women: prevalence as determined according to self-report and the 3-ounce water swallowing test. J Am Geriatr Soc 62:716–720. https://doi.org/10.1111/jgs.12745
Garand KLF, Hill EG, Amella E et al (2019) Bolus airway invasion observed during videofluoroscopy in healthy, non-dysphagic community-dwelling adults. Ann Otol Rhinol Laryngol 128:426–432. https://doi.org/10.1177/0003489419826141
Butler SG, Stuart A, Leng X et al (2011) The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerontol A Biol Sci Med Sci 66:452–458. https://doi.org/10.1093/gerona/glq234
Molfenter SM, Brates D, Herzberg E et al (2018) The swallowing profile of healthy aging adults: comparing noninvasive swallow tests to videofluoroscopic measures of safety and efficiency. J Speech Lang Hear Res 61:1603–1612. https://doi.org/10.1044/2018_jslhr-s-17-0471
Igarashi K, Kikutani T, Tamura F (2019) Survey of suspected dysphagia prevalence in home-dwelling older people using the 10-Item Eating Assessment Tool (EAT-10). PLoS ONE 14:e0211040. https://doi.org/10.1371/journal.pone.0211040
Takeuchi K, Furuta M, Okabe Y et al (2017) Swallowing disorders and 1-year functional decline in community-dwelling older adults receiving home care. J Oral Rehabil 44:982–987. https://doi.org/10.1111/joor.12577
Mikami Y, Watanabe Y, Motokawa K et al (2019) Association between decrease in frequency of going out and oral function in older adults living in major urban areas. Geriatr Gerontol Int 19:792–797. https://doi.org/10.1111/ggi.13715
Hida Y, Nishida T, Taniguchi C et al (2021) Association between swallowing function and oral bacterial flora in independent community-dwelling elderly. Aging Clin Exp Res 33:157–163. https://doi.org/10.1007/s40520-020-01521-3
Jardine M, Miles A, Allen J (2021) Self-reported swallowing and nutrition status in community-living older adults. Dysphagia 36:198–206. https://doi.org/10.1007/s00455-020-10125-y
Holland G, Jayasekeran V, Pendleton N et al (2011) Prevalence and symptom profiling of oropharyngeal dysphagia in a community dwelling of an elderly population: a self-reporting questionnaire survey. Dis Esophagus 24:476–480. https://doi.org/10.1111/j.1442-2050.2011.01182.x
Namasivayam-MacDonald AM, Shune SE (2020) The influence of swallowing impairments as an independent risk factor for burden among caregivers of aging parents: a cross-sectional study. Geriatr Nurs 41:81–88. https://doi.org/10.1016/j.gerinurse.2019.06.008
Shimazaki Y, Saito M, Nonoyama T et al (2020) Oral factors associated with swallowing function in independent elders. Oral Health Prev Dent 18:683–691. https://doi.org/10.3290/j.ohpd.a45071
Zhang H, Guo F, Tang M et al (2020) Association between skeletal muscle strength and dysphagia among chinese community-dwelling elderly adults. J Nutr Health Aging 24:642–649. https://doi.org/10.1007/s12603-020-1379-3
Zhang M, Li C, Zhang F et al (2021) Prevalence of dysphagia in China: an epidemiological survey of 5943 participants. Dysphagia 36:339–350. https://doi.org/10.1007/s00455-020-10138-7
Chaleekrua S, Janpol K, Wattanapan P (2021) Swallowing problems among community-dwelling elderly in northeastern Thailand. J Prim Care Community Health 12:21501327211019596. https://doi.org/10.1177/21501327211019596
Liu HY, Chen JH, Hsu KJ et al (2021) Decreased tongue pressure associated with aging, chewing and swallowing difficulties of community-dwelling older adults in Taiwan. J Pers Med 11:653. https://doi.org/10.3390/jpm11070653
Mello RP, Xavier MO, Tomasi E et al (2021) Dysphagia perception among community-dwelling older adults from a municipality in southern Brazil. Dysphagia 37:879–888. https://doi.org/10.1007/s00455-021-10347-8
Nishida T, Yamabe K, Honda S (2021) The influence of dysphagia on nutritional and frailty status among community-dwelling older adults. Nutrients 13:512. https://doi.org/10.3390/nu13020512
Sella-Weiss O (2021) Association between swallowing function, malnutrition and frailty in community dwelling older people. Clin Nutr ESPEN 45:476–485. https://doi.org/10.1016/j.clnesp.2021.06.028
Takeuchi N, Sawada N, Ekuni D et al (2021) Oral diadochokinesis is related to decline in swallowing function among community-dwelling Japanese elderly: a cross-sectional study. Aging Clin Exp Res 33:399–405. https://doi.org/10.1007/s40520-020-01547-7
Fernández-Rosati J, Lera L, Fuentes-López E et al (2018) Validez y confiabilidad del cuestionario Eating Assessment Tool 10 (EAT-10) para detectar disfagia en adultos mayores chilenos. Rev Med Chil 146:1008–1015
Yamabe K, Nishida T, Ide Y et al (2019) Performance of Japanese community-dwelling older adults in the 100-mL water swallowing test. Acta Med Nagasaki 63:1–10
Ogino Y, Suzuki H, Ayukawa Y et al (2021) Analyses of swallowing function and its related factors in community-dwelling elderly patients: a case-control study. J Clin Med 10:3437. https://doi.org/10.3390/jcm10153437
Daniels SK, Anderson JA, Willson PC (2012) Valid items for screening dysphagia risk in patients with stroke: a systematic review. Stroke 43:892–897. https://doi.org/10.1161/strokeaha.111.640946
Paiva KMD, Xavier IC, Farias N (2012) Envelhecimento e disfagia: uma questão de saúde pública. J Aging Innov 1:56–67
Marik PE, Kaplan D (2003) Aspiration pneumonia and dysphagia in the elderly. Chest 124:328–336. https://doi.org/10.1378/chest.124.1.328
Achem SR, Devault KR (2005) Dysphagia in aging. J Clin Gastroenterol 39:357–371. https://doi.org/10.1097/01.mcg.0000159272.88974.54
O’Horo JC, Rogus-Pulia N, Garcia-Arguello L et al (2015) Bedside diagnosis of dysphagia: a systematic review. J Hosp Med 10:256–265. https://doi.org/10.1002/jhm.2313
Bours GJ, Speyer R, Lemmens J et al (2009) Bedside screening tests vs videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. J Adv Nurs 65:477–493. https://doi.org/10.1111/j.1365-2648.2008.04915.x
Cordier R, Joosten A, Clavé P et al (2017) Evaluating the psychometric properties of the Eating Assessment Tool (EAT-10) using Rasch analysis. Dysphagia 32:250–260. https://doi.org/10.1007/s00455-016-9754-2
Swan K, Cordier R, Brown T et al (2019) Psychometric properties of visuoperceptual measures of videofluoroscopic and fibre-endoscopic evaluations of swallowing: a systematic review. Dysphagia 34:2–33. https://doi.org/10.1007/s00455-018-9918-3
Ney DM, Weiss JM, Kind AJ et al (2009) Senescent swallowing: impact, strategies, and interventions. Nutr Clin Pract 24:395–413. https://doi.org/10.1177/0884533609332005
Baijens LW, Clavé P, Cras P et al (2016) European society for swallowing disorders—European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging 11:1403–1428. https://doi.org/10.2147/cia.S107750
National Academies of Sciences, Engineering, and Medicine, Division of Behavioral and Social Science and Education, Committee on Population, Majmundar MK, Hayward MD (2018) Future directions for the demography of aging: proceedings of a workshop, (eds.), National Academies Press (US), Washington (DC)
Braveman PA, Cubbin C, Egerter S et al (2005) Socioeconomic status in health research: one size does not fit all. JAMA 294:2879–2888. https://doi.org/10.1001/jama.294.22.2879
Howe LD, Galobardes B, Matijasevich A et al (2012) Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol 41:871–886. https://doi.org/10.1093/ije/dys037
Duncan GJ, Daly MC, McDonough P et al (2002) Optimal indicators of socioeconomic status for health research. Am J Public Health 92:1151–1157. https://doi.org/10.2105/ajph.92.7.1151
Raghupathi V, Raghupathi W (2020) The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Health 78:20. https://doi.org/10.1186/s13690-020-00402-5
Dewalt DA, Berkman ND, Sheridan S et al (2004) Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med 19:1228–1239. https://doi.org/10.1111/j.1525-1497.2004.40153.x
Nogueira D, Reis E (2013) Swallowing disorders in nursing home residents: how can the problem be explained? Clin Interv Aging 8:221–227. https://doi.org/10.2147/cia.S39452
Jansen T, Rademakers J, Waverijn G et al (2018) The role of health literacy in explaining the association between educational attainment and the use of out-of-hours primary care services in chronically ill people: a survey study. BMC Health Serv Res 18:394. https://doi.org/10.1186/s12913-018-3197-4
Ribeiro UASL, Vicente LCC, Lemos SMA (2021) Functional health literacy in adults and elderly with dysphagia. Audiol Commun Res. https://doi.org/10.1590/2317-6431-2020-2351
von Wühlisch FS, Pascoe M (2011) Maximizing health literacy and client recall in a developing context: speech-language therapist and client perspectives. Int J Lang Commun Disord 46:592–607. https://doi.org/10.1111/j.1460-6984.2011.00014.x
Nutbeam D, Lloyd JE (2021) Understanding and responding to health literacy as a social determinant of health. Annu Rev Public Health 42:159–173. https://doi.org/10.1146/annurev-publhealth-090419-102529
Acknowledgements
This work was supported by the Brazilian Ministry of Education; National Council for Scientific and Technological Development—CNPq. JBH and BNGG hold productivity fellowship from CNPq and RSR received a PhD scholarship. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (Capes)—Finance Code 001 (JBH and MAZM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
The study protocol is registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020153738).
Informed consent
For this type of study, no informed consent is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rech, R.S., de Goulart, B.N.G., dos Santos, K.W. et al. Frequency and associated factors for swallowing impairment in community-dwelling older persons: a systematic review and meta-analysis. Aging Clin Exp Res 34, 2945–2961 (2022). https://doi.org/10.1007/s40520-022-02258-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-022-02258-x