Abstract
Background
Increasing incidences of swallowing dysfunction, or dysphagia, a risk factor for aspiration pneumonia, are being reported in aging populations.
Aims
To investigate the relationship between swallowing function and oral bacteria in independent, community-dwelling elderly.
Methods
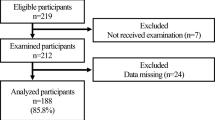
This study recruited 139 community-dwelling individuals aged ≥ 70 years with poor swallowing function. The presence of anaerobic (Prevotella spp. and Fusobacterium spp.) and aerobic bacteria was examined in the participants’ oral cavity flora. Swallowing function was evaluated using a 30 mL water swallowing test. Multivariate logistic regression analyses were performed to examine the association between oral bacteria and swallowing function.
Results
Swallowing function was assessed as abnormal in 2.9% and as abnormal in 47.5% of the subjects. The colony-forming units (CFUs/ml) of Prevotella spp. were associated with the swallowing dysfunction (odds ratio [OR] 3.45, 95% confidence interval [CI] 1.49–8.11). Further, CFUs/ml of Fusobacterium spp. and aerobes did not correlate with the swallowing dysfunction but were related with the number of teeth (OR 2.71; 95% CI 1.28–5.74, and OR 0.40; 95% CI, 0.18–0.91, respectively)
Conclusions
Swallowing dysfunction in community-dwelling elderly is associated with increased abundance of Prevotella spp., which indirectly may be an increased risk factor for aspiration pneumonia.
Similar content being viewed by others
References
Kaplan V, Angus DC, Griffin MF et al (2002) Hospitalized community-acquired pneumonia in the elderly: age- and sex-related patterns of care and outcome in the United States. Am J Respir Crit Care Med 165:766–772
Morimoto K, Suzuki M, Ishifuji T et al (2015) The burden and etiology of community-onset pneumonia in the aging Japanese population: a multicenter prospective study. PLoS ONE 10:e0122247. https://doi.org/10.1371/journal.pone.0122247
Teramoto S, Fukuchi Y, Sasaki H et al (2008) High Incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicentre, prospective study in Japan. J Am Geriatr Soc 56:577–579. https://doi.org/10.1111/j.1532-5415.2008.01597.x
Almirall J, Rofes L, Serra-Prat M et al (2013) Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J 41:923–928. https://doi.org/10.1183/09031936.00019012
van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM (2011) Meta-analysis of dysphagia and aspiration pneumonia in frail elders. J Dent Res 90:1398–1404. https://doi.org/10.1177/0022034511422909
Wirth R, Dziewas R, Beck AM et al (2016) Oropharyngeal dysphagia in older persons – from pathophysiology to adequate intervention: a review and summary of an international expert meeting. Clin Interv Aging 11:189–208. https://doi.org/10.2147/CIA.S97481
Yamasaki K, Kawanami T, Yatera K et al (2013) Significance of anaerobes and oral Bacteria in community-acquired pneumonia. PLoS ONE 8:e63103. https://doi.org/10.1371/journal.pone.0063103
Scannapieco FA (1999) Role of oral bacteria in respiratory infection. J Periodontol 70:793–802
Percival RS, Challacombe SJ, Marsh PD (1991) Age-related microbiological changes in the salivary and plaque microflora of healthy adults. J Med Microbiol 35:5–11
Guidelines committee on the Japanese Respiratory Society for respiration infection (2010) The JRS Guidelines for the Management of Community-Acquired Pneumonia in Adults. Tokyo, pp 72–73
Tohara H, Saitoh E, Mays KA et al. (2003) Three tests for predicting aspiration without videofluorography. Dysphagia 18:126–134
Teramoto S, Fukuchi Y (2000) Detection of aspiration and swallowing disorder in older stroke patients: simple swallowing provocation test versus water swallowing test. Arch Phys Med Rehabil 81:1517–1519
Nishiwaki K, Tsuji T, Liu M et al. (2005) Identification of a simple screening tool for dysphagia in patients with stroke using factor analysis of multiple dysphagia variables. J Rehabil Med 37:247–251
The Japan Dental Association (2015) Evidence of contributing dental medical and oral health in healthy longevity society edited by the Public Interest Incorporated Orchestra Japan Dental Association. Tokyo, pp 24–32
Morino T, Ookawa K, Hagiwara Y et al. (2012) Relationship between deterioration of swallowing function and oral health status in elders who require nursing care and have preserved teeth. J Dent Health 62:478–483
Bartlett JG (2013) How important are anaerobic bacteria in aspiration pneumonia: when should they be treated and what is optimal therapy. Infect Dis Clin North Am 27:149–155. https://doi.org/10.1016/j.idc.2012.11.016
Teramoto S, Yoshida K, Hizawa N (2015) Update on the pathogenesis and management of pneumonia in the elderly-roles of aspiration pneumonia. Respir Investig 53:178–184. https://doi.org/10.1016/j.resinv.2015.01.003
Ortega O, Sakwinska O, Combremont S et al. (2015) High prevalence of colonization of oral cavity by respiratory pathogens in frail older patients with oropharyngeal dysphagia. Neurogastroenterol Motil 27:1804–1816
Kageyama S, Takeshita T, Furuta M et al. (2018) Relationships of variations in the tongue microbiota and pneumonia mortality in nursing home residents. J Gerontol A Biol Sci Med Sci 73:1097–1102. https://doi.org/10.1093/gerona/glx205
Kageyama S, Takeshita T, Asakawa M et al. (2017) Relative abundance of total subgingival plaque-specific bacteria in salivary microbiota reflects the overall periodontal condition in patients with periodontitis. PLoS ONE 12: e0174782. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0174782
Asakawa M, Takeshita T, Furuta M et al (2018) Tongue microbiota and oral health status in community-dwelling elderly adults. mSphere 3: 00332-18. https://doi.org/10.1128/mSphere.00332-18
Kikutani T, Tamura F, Tashiro H et al. (2015) Relationship between oral bacteria count and pneumonia onset in elderly nursing home residents. Geriatr Gerontol Int 15:417–421
Nishizawa T, Niikura Y, Akasaka K et al. (2019) Pilot study for risk assessment of aspiration pneumonia based on oral bacteria levels and serum biomarkers. BMC Infect Dis 19:761. https://doi.org/10.1186/s12879-019-4327-2
Sjoren P, Nilsson E, Forsell M et al. (2008) A systematic review of the preventive effect of oral hygiene on pneumonia and respiratory tract infection in elderly people in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. J Am Geriatr Soc 58:2124–2130
Tada A, Miura H (2012) Prevention of aspiration pneumonia (AP) with oral care. Arch Gerontol Geriatr 55:16–21. https://doi.org/10.1016/j.archger.2011.06.029
Kertscher B, Speyer R, Palmieri M et al. (2014) Bedside screening to detect oropharyngeal dysphagia in patients with neurological disorders: an updated systematic review. Dysphagia 29:204–212
Clavé P, Arreola V, Romea M et al. (2008) Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr 27:806–815
Serra-Prat M, Hinojosa G, Lopez D et al. (2011) Prevalence of oropharyngeal dysphagia and impaired safety and efficacy of swallow in independently living older persons. J Am Geriatr Soc 59:186–187
Amann RI, Ludwig W, Schleifer KH (1995) Phylogenetic identification and in situ detection of individual microbial cells without cultivation. Microbiol Rev 59:143–169
Hugenholz P, Goebel BM, Pace NR (1998) Impact of culture-independent studies on the emerging phylogenetic view of bacterial diversity. J Bacteriol 180:4765–4774
Author information
Authors and Affiliations
Contributions
YH conceived this study, participated in its design and coordination, performed the statistical analysis, and drafted the manuscript. TN and CT contributed to the statistical analysis and helped draft the manuscript. HS contributed to the conception and design of this study, contributed to the statistical analysis, helped draft the manuscript and supervised the whole study process. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
This study was approved by the bioethics committee in Nagoya University Graduate School of Medicine (approval number 13–139) and was performed in accordance with the ethical standards laid down in an appropriate version of the 1964 Declaration of Helsinki.
Informed consent
All the participants in this study provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hida, Y., Nishida, T., Taniguchi, C. et al. Association between swallowing function and oral bacterial flora in independent community-dwelling elderly. Aging Clin Exp Res 33, 157–163 (2021). https://doi.org/10.1007/s40520-020-01521-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01521-3