Abstract
Background and Objective
Although tumor lysis syndrome was reported with obinutuzumab and rituximab, the association with CD20 monoclonal antibodies for chronic lymphocytic leukemia is unclear.
Methods
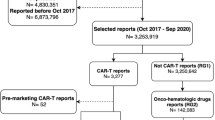
A disproportionality analysis was conducted to investigate the link between CD20 monoclonal antibodies and tumor lysis syndrome by accounting for known confounders and comparing with other anticancer drugs, using data from the US Food and Drug Administration Adverse Event Reporting System. Reporting odds ratios and the information component were calculated as disproportionality measures. A stepwise sensitivity analysis was conducted to test the robustness of disproportionality signals. Bradford Hill criteria were adopted to globally assess the potential causal relationship.
Results
From 2004 to 2022, 197, 368, 41, and 14 tumor lysis syndrome reports were detected for obinutuzumab, rituximab, ofatumumab, and alemtuzumab (CD52 monoclonal antibody), respectively. Disproportionality signals were found for the above four monoclonal antibodies when compared with other anticancer drugs. Sensitivity analyses confirmed robust disproportionality signals for obinutuzumab, rituximab, and ofatumumab. The median onset time was 4.5, 1.5, and 2.5 days for rituximab, obinutuzumab, and ofatumumab, respectively. A potential causal relationship was fulfilled by assessing Bradford Hill criteria.
Conclusions
This pharmacovigilance study on the FDA Adverse Event Reporting System detected a plausible association between CD20 monoclonal antibodies (but not CD52) and tumor lysis syndrome by assessing the adapted Bradford Hill criteria. Urgent clarification of drug- and patient-related risk factors is needed through large comparative population-based studies.



Similar content being viewed by others
References
Shadman M. Diagnosis and treatment of chronic lymphocytic leukemia: a review. JAMA. 2023;329(11):918–32.
Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, et al. iwCLL guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018;131(25):2745–60.
Hallek M, Al-Sawaf O. Chronic lymphocytic leukemia: 2022 update on diagnostic and therapeutic procedures. Am J Hematol. 2021;96(12):1679–705.
Howard SC, Trifilio S, Gregory TK, Baxter N, McBride A. Tumor lysis syndrome in the era of novel and targeted agents in patients with hematologic malignancies: a systematic review. Ann Hematol. 2016;95(4):563–73.
Howard SC, Jones DP, Pui CH. The tumor lysis syndrome. N Engl J Med. 2011;364(19):1844–54.
Williams SM, Killeen AA. Tumor lysis syndrome. Arch Pathol Lab Med. 2019;143(3):386–93.
Wanchoo R, Bernabe Ramirez C, Barrientos J, Jhaveri KD. Renal involvement in chronic lymphocytic leukemia. Clin Kidney J. 2018;11(5):670–80.
Cheson BD, Heitner Enschede S, Cerri E, Desai M, Potluri J, Lamanna N, et al. Tumor lysis syndrome in chronic lymphocytic leukemia with novel targeted agents. Oncologist. 2017;22(11):1283–91.
Mustafa M, Mohamed MB, Hayat A. Tumour lysis syndrome and partial remission occurring after administration of a test dose of obinutuzumab. Eur J Case Rep Intern Med. 2017;4(1): 000516.
Jensen M, Winkler U, Manzke O, Diehl V, Engert A. Rapid tumor lysis in a patient with B-cell chronic lymphocytic leukemia and lymphocytosis treated with an anti-CD20 monoclonal antibody (IDEC-C2B8, rituximab). Ann Hematol. 1998;77(1–2):89–91.
Yang H, Rosove MH, Figlin RA. Tumor lysis syndrome occurring after the administration of rituximab in lymphoproliferative disorders: high-grade non-Hodgkin’s lymphoma and chronic lymphocytic leukemia. Am J Hematol. 1999;62(4):247–50.
Raschi E, Gatti M, Gelsomino F, Ardizzoni A, Poluzzi E, De Ponti F. Lessons to be learnt from real-world studies on immune-related adverse events with checkpoint inhibitors: a clinical perspective from pharmacovigilance. Target Oncol. 2020;15(4):449–66.
Sarangdhar M, Tabar S, Schmidt C, Kushwaha A, Shah K, Dahlquist JE, et al. Data mining differential clinical outcomes associated with drug regimens using adverse event reporting data. Nat Biotechnol. 2016;34(7):697–700.
Faillie JL. Case-non-case studies: principle, methods, bias and interpretation. Therapie. 2019;74(2):225–32.
Noguchi Y, Tachi T, Teramachi H. Detection algorithms and attentive points of safety signal using spontaneous reporting systems as a clinical data source. Brief Bioinform. 2021;22(6): bbab347.
Rothman KJ, Lanes S, Sacks ST. The reporting odds ratio and its advantages over the proportional reporting ratio. Pharmacoepidemiol Drug Saf. 2004;13(8):519–23.
Noren GN, Hopstadius J, Bate A. Shrinkage observed-to-expected ratios for robust and transparent large-scale pattern discovery. Stat Methods Med Res. 2013;22(1):57–69.
Tambaro FP, Wierda WG. Tumour lysis syndrome in patients with chronic lymphocytic leukaemia treated with BCL-2 inhibitors: risk factors, prophylaxis, and treatment recommendations. Lancet Haematol. 2020;7(2):e168–76.
Raschi E, Fusaroli M, Ardizzoni A, Poluzzi E, De Ponti F. Cyclin-dependent kinase 4/6 inhibitors and interstitial lung disease in the FDA adverse event reporting system: a pharmacovigilance assessment. Breast Cancer Res Treat. 2021;186(1):219–27.
Barbar T, Jaffer SI. Tumor lysis syndrome. Adv Chronic Kidney Dis. 2021;28(5):438-46.e1.
National Cancer Institute. Drugs approved for chronic lymphocytic leukemia (CLL). https://www.cancer.gov/about-cancer/treatment/drugs/leukemia. Accessed 17 Sep 2023.
Wierda WG, Byrd JC, Abramson JS, Bilgrami SF, Bociek G, Brander D, et al. Chronic lymphocytic leukemia/small lymphocytic lymphoma, version 4.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw. 2020;18(2):185–217.
European Medicines Agency. Screening for adverse reactions in EudraVigilance. Inspections, Human Medicines, Pharmacovigilance and Committees Division, EMA/849944/2016; 2016.
Yang K, Li J, Sun Z, Bai C, Zhao L. Effect of age on the risk of immune-related adverse events in patients receiving immune checkpoint inhibitors. Clin Exp Med. 2023. https://doi.org/10.1007/s10238-023-01055-8.
Zhang T, Ye X, Guo X, Wu G, Hou Y, Xu J, et al. Signal detection based on time to onset algorithm in spontaneous reporting system of China. Drug Saf. 2017;40(4):343–50.
Nakamura M, Umetsu R, Abe J, Matsui T, Ueda N, Kato Y, et al. Analysis of the time-to-onset of osteonecrosis of jaw with bisphosphonate treatment using the data from a spontaneous reporting system of adverse drug events. J Pharm Health Care Sci. 2015;1:34.
Khaleel MA, Khan AH, Ghadzi SMS, Adnan AS, Abdallah QM. A standardized dataset of a spontaneous adverse event reporting system. Healthcare (Basel). 2022;10(3):420.
Ando G, Taguchi K, Enoki Y, Yokoyama Y, Kizu J, Matsumoto K. Evaluation of the expression time of ganciclovir-induced adverse events using JADER and FAERS. Biol Pharm Bull. 2019;42(11):1799–804.
Raschi E, Fusaroli M, Giunchi V, Repaci A, Pelusi C, Mollica V, et al. Adrenal insufficiency with anticancer tyrosine kinase inhibitors targeting vascular endothelial growth factor receptor: analysis of the FDA Adverse Event Reporting System. Cancers (Basel). 2022;14(19):4610.
Fusaroli M, Raschi E, Giunchi V, Menchetti M, Rimondini Giorgini R, De Ponti F, et al. Impulse control disorders by dopamine partial agonists: a pharmacovigilance-pharmacodynamic assessment through the FDA Adverse Event Reporting System. Int J Neuropsychopharmacol. 2022;25(9):727–36.
Muganurmath CS, Curry AL, Schindzielorz AH. Causality assessment of olfactory and gustatory dysfunction associated with intranasal fluticasone propionate: application of the Bradford Hill criteria. Adv Ther. 2018;35(2):173–90.
Constantinides M, Fayd’herbe De Maudave A, Potier-Cartereau M, Campos-Mora M, Cartron G, Villalba M. Direct cell death induced by CD20 monoclonal antibodies on B cell lymphoma cells revealed by new protocols of analysis. Cancers (Basel). 2023;15(4):1109.
Nuckel H, Frey UH, Roth A, Duhrsen U, Siffert W. Alemtuzumab induces enhanced apoptosis in vitro in B-cells from patients with chronic lymphocytic leukemia by antibody-dependent cellular cytotoxicity. Eur J Pharmacol. 2005;514(2–3):217–24.
Kater AP, Kersting S, van Norden Y, Dubois J, Dobber JA, Mellink CH, et al. Obinutuzumab pretreatment abrogates tumor lysis risk while maintaining undetectable MRD for venetoclax + obinutuzumab in CLL. Blood Adv. 2018;2(24):3566–71.
Al-Sawaf O, Fink A-M, Robrecht S, Sinha A, Tandon M, Eichhorst BF, et al. Prevention and management of tumor lysis syndrome in patients with CLL and coexisting conditions treated with venetoclax-obinutuzumab or chlorambucil-obinutuzumab: results from the randomized CLL14 trial. Blood. 2019;134:4315.
Pierpont TM, Limper CB, Richards KL. Past, present, and future of rituximab: the world’s first oncology monoclonal antibody therapy. Front Oncol. 2018;8:163.
Acknowledgements
We appreciate the help of Dr. Mohammad Ali Khaleel in extracting raw data from a cleaned FAERS dataset.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by the National Natural Science Foundation of China (No. 81974532), the Hunan Natural Science Funds for Distinguished Young Scholars (No. 2022JJ10097), and the Research Foundation of Education Bureau of Hunan Province for Young Scholars (No. 21B0014).
Conflict of Interest
Shuang Xia, Jia-ting Ma, Emanuel Raschi, Rui Ma, Bi-kui Zhang, Linna Guo, Yoshihiro Noguchi, Mayur Sarangdhar, Hui Gong, and Miao Yan have no conflicts of interest that are directly relevant to the content of this study.
Ethics Approval
No institutional ethics approval was required because this study utilized anonymized data from an open-access database.
Consent to Participate
Because all data in FAERS are anonymized, patient informed consent is not required.
Consent for Publication
Not applicable.
Data Availability
All data are publicly available on the website of AERSMine, a curated FAERS database: https://research.cchmc.org/aers/.
Code Availability
Not applicable.
Author Contributions
Conceptualization: MY, HG, SX; methodology: NY, ER, SX; formal analysis and investigation: SX, JTM; writing, original draft preparation: SX, JTM, ER; writing, review, and editing: SX, ER, NY, HG, MY; funding acquisition: MY; resources: MS, LG, BKZ; supervision: MY, HG.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xia, S., Ma, Jt., Raschi, E. et al. Tumor Lysis Syndrome with CD20 Monoclonal Antibodies for Chronic Lymphocytic Leukemia: Signals from the FDA Adverse Event Reporting System. Clin Drug Investig 43, 773–783 (2023). https://doi.org/10.1007/s40261-023-01308-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-023-01308-0