Abstract
Purpose
Despite lung cancer is one of the leading causes of cancer-related deaths, it remains hard to discover effective diagnostic and therapeutic approaches. Moreover, the five-year survival rate is relatively lower than other tumors. So urgent needs for finding a new theranostic target to treat lung cancer effectively. This study aims to present SOCS3 and NOD2 proteins as novel targets for diagnosis and therapy.
Methods
We first confirmed SOCS3 expression level in patients’ tissues. Then, we applied knockdown and overexpression of SOCS3 on lung cancer cell lines and performed proliferation, migration, and invasion assay. After that, we found NOD2 is a target of SOCS3 and introduced overexpression of NOD2 to A549 for verifying reduced tumorigenicity of lung cancer cells.
Results
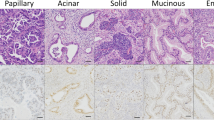
We identified protein expression level of SOCS3 was frequently higher in tumor tissues than adjacent normal tissues. Truly, overexpression of SOCS3 promoted proliferation, migration, and invasion capacity of lung cancer cells. We found that SOCS3 interacts with NOD2 and SOCS3 ubiquitinates NOD2 directly. Furthermore, lung cancer tissues with higher SOCS3 expression showed lower NOD2 expression. We confirmed overexpression of NOD2 leads to suppressed tumorigenicity of lung cancer cells, and these effects occurred through MAPK pathway.
Conclusion
Collectively, our work reveals novel roles of SOCS3 in lung tumorigenesis and proposes SOCS3 as a promising biomarker candidate for therapeutic and diagnostic target for lung cancer.






Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
R.L. Siegel, K.D. Miller, H.E. Fuchs, A. Jemal, Cancer Statistics, 2021. CA Cancer J Clin. 71(1), 7–33 (2021)
K.D. Miller, L. Nogueira, A.B. Mariotto, J.H. Rowland, K.R. Yabroff, C.M. Alfano et al., Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 69(5), 363–385 (2019)
W.-L. Tan, A. Jain, A. Takano, E.W. Newell, N.G. Iyer, W.-T. Lim et al., Novel therapeutic targets on the horizon for Lung cancer. Lancet Oncol. 17(8), e347–e62 (2016)
X. Hu, J. Li, M. Fu, X. Zhao, W. Wang, The JAK/STAT signaling pathway: from bench to clinic. Signal. Transduct. Target. Ther. 6(1), 402 (2021)
K. Inagaki-Ohara, T. Kondo, M. Ito, A. Yoshimura, SOCS, inflammation, and cancer. JAKSTAT. 2(3), e24053 (2013)
J.J. Babon, N.A. Nicola, The biology and mechanism of action of suppressor of cytokine signaling 3. Growth Factors. 30(4), 207–219 (2012)
L. Dai, Z. Li, Y. Tao, W. Liang, W. Hu, S. Zhou et al., Emerging roles of suppressor of cytokine signaling 3 in human cancers. Biomed. Pharmacother. 144, 112262 (2021)
Y. Ben-Neriah, M. Karin, Inflammation meets cancer, with NF-kappaB as the matchmaker. Nat. Immunol. 12(8), 715–723 (2011)
R. Caruso, N. Warner, N. Inohara, G. Nunez, NOD1 and NOD2: signaling, host defense, and inflammatory Disease. Immunity. 41(6), 898–908 (2014)
M.L. Disis, Immune regulation of cancer. J. Clin. Oncol. 28(29), 4531–4538 (2010)
M.J. Smyth, G.P. Dunn, R.D. Schreiber, Cancer Immunosurveillance and Immunoediting: The Roles of Immunity in Suppressing Tumor Development and Shaping Tumor Immunogenicity. Adv. Immunol. 90, 1–50 (2006)
M.A. Huber, N. Azoitei, B. Baumann, S. Grünert, A. Sommer, H. Pehamberger et al., NF-κB is essential for epithelial-mesenchymal transition and Metastasis in a model of Breast cancer progression. J. Clin. Invest. 114(4), 569–581 (2004)
H.J. Maier, U. Schmidt-Strassburger, M.A. Huber, E.M. Wiedemann, H. Beug, T. Wirth, NF-kappaB promotes epithelial-mesenchymal transition, migration and invasion of pancreatic carcinoma cells. Cancer Lett. 295(2), 214–228 (2010)
S.J. Kim, T. Hyeong Lee, S. Hee Nam, J.H. Kim, S. Oh, Y. Sook Cho et al., Association of Uba6-Specific-E2 (USE1) with Lung Tumorigenesis. J. Natl. Cancer Inst. 109(3), 1–11 (2017)
J.O. Jin, G.D. Lee, S.H. Nam, T.H. Lee, D.H. Kang, J.K. Yun et al., Sequential ubiquitination of p53 by TRIM28, RLIM, and MDM2 in lung tumorigenesis. Cell. Death Differ. 28(6), 1790–1803 (2021)
K.H. Lee, A. Biswas, Y.J. Liu, K.S. Kobayashi, Proteasomal degradation of Nod2 protein mediates tolerance to bacterial cell wall components. J. Biol. Chem. 287(47), 39800–39811 (2012)
X. Ma, Y. Qiu, Y. Sun, L. Zhu, Y. Zhao, T. Li et al., NOD2 inhibits tumorigenesis and increases chemosensitivity of hepatocellular carcinoma by targeting AMPK pathway. Cell. Death Dis. 11(3), 174 (2020)
S.M.N. Udden, L. Peng, J.L. Gan, J.M. Shelton, J.S. Malter, L.V. Hooper et al., NOD2 suppresses colorectal tumorigenesis via downregulation of the TLR pathways. Cell. Rep. 19(13), 2756–2770 (2017)
T. Kawai, S. Akira, The roles of TLRs, RLRs and NLRs in pathogen recognition. Int. Immunol. 21(4), 317–337 (2009)
F.R. Hirsch, G.V. Scagliotti, J.L. Mulshine, R. Kwon, W.J. Curran, Y.-L. Wu et al., Lung cancer: current therapies and new targeted treatments. The Lancet. 389(10066), 299–311 (2017)
Y. Yin, W. Liu, Y. Dai, SOCS3 and its role in associated Diseases. Hum. Immunol. 76(10), 775–780 (2015)
L.H. Jiang, Y.L. Hao, J.W. Zhu, Expression and prognostic value of HER-2/neu, STAT3 and SOCS3 in hepatocellular carcinoma. Clin. Res. Hepatol. Gastroenterol. 43(3), 282–291 (2019)
K. Inagaki-Ohara, H. Mayuzumi, S. Kato, Y. Minokoshi, T. Otsubo, Y.I. Kawamura et al., Enhancement of leptin receptor signaling by SOCS3 deficiency induces development of gastric tumors in mice. Oncogene. 33(1), 74–84 (2014)
M. Ying, D. Li, L. Yang, M. Wang, N. Wang, Y. Chen et al., Loss of SOCS3 expression is associated with an increased risk of recurrent Disease in breast carcinoma. J. Cancer Res. Clin. Oncol. 136(10), 1617–1626 (2010)
Y. Dong, S. Wang, C. Wang, Z. Li, Y. Ma, G. Liu, Antagonizing NOD2 Signaling with conjugates of Paclitaxel and Muramyl dipeptide derivatives sensitizes Paclitaxel Therapy and significantly prevents Tumor Metastasis. J. Med. Chem. 60(3), 1219–1224 (2017)
D.P. Chen, W.R. Ning, X.F. Li, Y. Wei, X.M. Lao, J.C. Wang et al., Peritumoral monocytes induce cancer cell autophagy to facilitate the progression of human hepatocellular carcinoma. Autophagy. 14(8), 1335–1346 (2018)
T. Yamaoka, S. Arata, M. Homma, T. Homma, S. Kusumoto, K. Ando et al., Blockade of EGFR activation promotes TNF-Induced Lung epithelial cell apoptosis and Pulmonary Injury. Int. J. Mol. Sci. 20(16), 4021 (2019)
Acknowledgements
All authors have also read the journal’s author agreement and manuscript has been reviewed and approved by all authors.
Funding
This study was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MIST) (NRF-2022R1A2C4002045, RS-2023-00208173, RS-2023-00207868).
Author information
Authors and Affiliations
Contributions
PL and GL conceptualization, IJ, JJ, JH JL, and PCL Formal analysis and investigation, Writing - original draft preparation, JY, JL, GL, PL Clinical specimen collection, Data analysis, Statistical analysis, IJ and PL Writing manuscript.All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Patient’s lung tissue samples Written informed consent was obtained from all the lung cancer patients who participated in this study. All experimental protocols were approved by the Institutional Review Board of Asan Medical Center and the University of Ulsan College of Medicine (2014 − 0960, 2020 − 1117). Human lung tissues were obtained through the Asan Bio Resource Center (2014-20(89)).
Animal studies All mice were bred at the animal facilities of the Asan Institute for Life Sciences, University of Ulsan College of Medicine. All animal procedures were approved by the Institutional Ethics Committee and Institutional Animal Care Committee of University of Ulsan College of Medicine (2016-02-168 and 2017-12-281).
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jeong, Ih., Yun, J.K., Jin, JO. et al. E3 ligase SOCS3 regulates NOD2 expression by ubiquitin proteasome system in lung cancer progression. Cell Oncol. (2023). https://doi.org/10.1007/s13402-023-00896-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s13402-023-00896-5