Abstract
As a promising drug delivery system, the temperature-sensitive liquid embolic agent (TempSLE) has yet to be reported in animal experiments in treating gastric cancer. We observed and compared computed tomography (CT) imaging changes, tumor volume, HE staining, and immunohistochemistry after transcatheter arterial chemoembolization (TACE) treatment in rabbit VX2 gastric cancer models to clarify the effectiveness of TempSLE loaded with oxaliplatin (TempSLE/Oxa) in treating gastric cancer. One milliliter TempSLE can be loaded with 20 mg oxaliplatin. The accumulative drug release rate at 30 min was 38.76%, and after 24 h, it reached more than 90%. CT examination 1 week after TACE revealed that the TempSLE/Oxa group presents unenhanced hypodense necrotic foci, the iodinated oil loaded with oxaliplatin (Ioil/Oxa) group presents shrinking tumors but still visible speckled foci of enhancement, and the normal saline (NS) group presents heterogeneous enhancement with larger tumors than before. In the postoperative autopsy of TACE, the tumor volumes of TempSLE/Oxa, Ioil/Oxa, and NS groups were 0.15 ± 0.06 cm3, 0.37 ± 0.11 cm3, and 1.19 ± 0.16 cm3, respectively, all of which were statistically different. The positive vascular endothelial growth factor (VEGF) and proliferating cell nuclear antigen (PCNA) expression percentages in the TempSLE/Oxa, Ioil/Oxa, and NS groups were statistically different and lowest in the TempSLE/Oxa group. In conclusion, the TempSLE can load a high dose of oxaliplatin to meet the demand of clinical applications. TempSLE/Oxa could effectively inhibit tumor cell proliferation and angiogenesis. This study provides experimental evidence for the further clinical application of the TempSLE/Oxa.
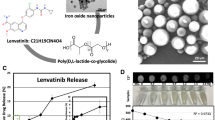
Graphical Abstract







Similar content being viewed by others
Data availability
The data generated and analyzed during the current study are available from the corresponding authors upon reasonable request.
Abbreviations
- TACE:
-
Transcatheter arterial chemoembolization
- DSA:
-
Digital subtraction angiography
- TempSLE:
-
Temperature-sensitive liquid embolic agent
- pNIPAAm:
-
Poly-N-isopropylacrylamide
- TempSLE/Oxa:
-
TempSLE loaded with oxaliplatin
- Ioil/Oxa:
-
Iodinated oil loaded with oxaliplatin
- NS:
-
Normal saline
- LC–MS/MS:
-
Liquid chromatography-tandem mass spectrometry
- HE:
-
Hematoxylin-eosin
- VEGF:
-
Vascular endothelial growth factor
- PCNA:
-
Proliferating cell nuclear antigen
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Mo DC, Qin L, Ye LJ. Neoadjuvant docetaxel, oxaliplatin, and S-1 in resectable advanced gastric cancer. J Clin Oncol. 2021;39:3883–4.
Li S, Yu W, Xie F, et al. Neoadjuvant therapy with immune checkpoint blockade, antiangiogenesis, and chemotherapy for locally advanced gastric cancer. Nat Commun. 2023;14:8.
Ajani JA, D’Amico TA, Bentrem DJ, et al. Gastric cancer, version 2.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2022;20:167–92.
Joharatnam-Hogan N, Shiu KK, Khan K. Challenges in the treatment of gastric cancer in the older patient. Cancer Treat Rev. 2020;85:101980.
Liang L, Li C, Wang MD, et al. Development and validation of a novel online calculator for estimating survival benefit of adjuvant transcatheter arterial chemoembolization in patients undergoing surgery for hepatocellular carcinoma. J Hematol Oncol. 2021;14:165.
Kim JH, Yoon HK, Kim SY, et al. Transcatheter arterial chemoembolization vs. chemoinfusion for unresectable hepatocellular carcinoma in patients with major portal vein thrombosis. Aliment Pharmacol Ther. 2009;29:1291–8.
Farinati F, Rinaldi M, Gianni S, et al. Transcatheter arterial chemoembolization in hepatocellular carcinoma. Hepatology (Baltimore, MD). 1998;28:1441–3.
Li N, Wang G, Duan G, et al. Clinical observation of transcatheter arterial chemoembolization in super-aged patients with advanced gastric cancer. Support Care Cancer. 2022;30:1441–50.
Peng D, Zhang B, Yuan C, et al. Gastric transcatheter chemoembolization can resolve advanced gastric cancer presenting with obstruction. Front Surg. 2022;9:1004064.
Golfieri R, Giampalma E, Renzulli M, et al. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer. 2014;111:255–64.
Overstreet DJ, Lee EJ, Pal A, et al. In situ crosslinking temperature-responsive hydrogels with improved delivery, swelling, and elasticity for endovascular embolization. J Biomed Mater Res B Appl Biomater. 2022;110:1911–21.
Din FU, Kim DW, Choi JY, et al. Irinotecan-loaded double-reversible thermogel with improved antitumor efficacy without initial burst effect and toxicity for intramuscular administration. Acta Biomater. 2017;54:239–48.
Xing R, Mustapha O, Ali T, et al. Development, characterization, and evaluation of SLN-loaded thermoresponsive hydrogel system of topotecan as biological macromolecule for colorectal delivery. Biomed Res Int. 2021;2021:9968602.
Din FU, Choi JY, Kim DW, et al. Irinotecan-encapsulated double-reverse thermosensitive nanocarrier system for rectal administration. Drug Delivery. 2017;24:502–10.
Moghadam S, Larson RG. Assessing the efficacy of poly(N-isopropylacrylamide) for drug delivery applications using molecular dynamics simulations. Mol Pharm. 2017;14:478–91.
Batool S, Sohail S, Ud Din F, et al. A detailed insight of the tumor targeting using nanocarrier drug delivery system. Drug Delivery. 2023;30:2183815.
He Y, Yuan T, Wang X, et al. Temperature sensitive hydrogel for preoperative treatment of renal carcinoma. Mater Sci Eng C Mater Biol Appl. 2020;111:110798.
Bi Y, Ren K, Ren J, et al. Oxaliplatin eluting CalliSpheres microspheres for the treatment of unresectable or recurrent hepatocellular carcinoma. Front Pharmacol. 2022;13:923585.
Bi Y, Li F, Ren J, et al. The safety and efficacy of oxaliplatin-loaded drug-eluting beads transarterial chemoembolization for the treatment of unresectable or advanced lung cancer. Front Pharmacol. 2022;13:1079707.
Lym JS, Nguyen QV, da Ahn W, et al. Sulfamethazine-based pH-sensitive hydrogels with potential application for transcatheter arterial chemoembolization therapy. Acta Biomater. 2016;41:253–63.
Zhao H, Zheng C, Feng G, et al. Temperature-sensitive poly(N-isopropylacrylamide-co-butyl methylacrylate) nanogel as an embolic agent: distribution, durability of vascular occlusion, and inflammatory reactions in the renal artery of rabbits. AJNR Am J Neuroradiol. 2013;34:169–76.
Ma J, Wang B, Shao H, et al. Hydrogels for localized chemotherapy of liver cancer: a possible strategy for improved and safe liver cancer treatment. Drug Delivery. 2022;29:1457–76.
Lanzalaco S, Armelin E. Poly(N-isopropylacrylamide) and copolymers: a review on recent progresses in biomedical applications. Gels (Basel, Switzerland). 2017;3.
Narayanaswamy R, and Torchilin VP. Hydrogels and their applications in targeted drug delivery. Molecules (Basel, Switzerland). 2019;24.
Kikuchi IS, Cardoso Galante RS, Dua K, et al. Hydrogel based drug delivery systems: a review with special emphasis on challenges associated with decontamination of hydrogels and biomaterials. Curr Drug Deliv. 2017;14:917–25.
Khan MW, Zou C, Hassan S, et al. Cisplatin and oleanolic acid co-loaded pH-sensitive CaCO(3) nanoparticles for synergistic chemotherapy. RSC Adv. 2022;12:14808–18.
Zhang ZS, Li HZ, Ma C, et al. Conventional versus drug-eluting beads chemoembolization for infiltrative hepatocellular carcinoma: a comparison of efficacy and safety. BMC Cancer. 2019;19:1162.
Qian K, Ma Y, Wan J, et al. The studies about doxorubicin-loaded p(N-isopropyl-acrylamide-co-butyl methylacrylate) temperature-sensitive nanogel dispersions on the application in TACE therapies for rabbit VX2 liver tumor. J Control Release. 2015;212:41–9.
Wei W, Li H, Yin C, et al. Research progress in the application of in situ hydrogel system in tumor treatment. Drug Delivery. 2020;27:460–8.
Din FU, Aman W, Ullah I, et al. Effective use of nanocarriers as drug delivery systems for the treatment of selected tumors. Int J Nanomed. 2017;12:7291–309.
Tong H, Duan LG, Zhou HY, et al. Modification of the method to establish a hepatic VX2 carcinoma model in rabbits. Oncol Lett. 2018;15:5333–8.
Zhang L, Sun JH, Ji JS, et al. Imaging changes and clinical complications after drug-eluting bead versus conventional transarterial chemoembolization for unresectable hepatocellular carcinoma: multicenter study. AJR Am J Roentgenol. 2021;217:933–43.
Partyka R, Gonciarz M, Jałowiecki P, et al. VEGF and metalloproteinase 2 (MMP 2) expression in gastric cancer tissue. Med Sci Monit. 2012;18:Br130-134.
Fu JD, Yao JJ, Wang H, et al. Effects of EGCG on proliferation and apoptosis of gastric cancer SGC7901 cells via down-regulation of HIF-1α and VEGF under a hypoxic state. Eur Rev Med Pharmacol Sci. 2019;23:155–61.
Zhang Q, Wu J, Bai X, et al. Evaluation of intra-tumoral vascularization in hepatocellular carcinomas. Front Med. 2020;7:584250.
Li N, Deng W, Ma J, et al. Prognostic evaluation of Nanog, Oct4, Sox2, PCNA, Ki67 and E-cadherin expression in gastric cancer. Med Oncol (Northwood, London, England). 2015;32:433.
Acknowledgements
We thank the Medical Research Center of the First Affiliated Hospital of Zhengzhou University for the technical support.
Funding
This work was supported by Central Plains Scholars Workstation in 2022 (workstation numbers ZYGZZ2022087; grant numbers 234400510027) and Central Plains Scholars Workstation in 2021 (workstation numbers ZYGZZ2021054; grant numbers 224400510024).
Author information
Authors and Affiliations
Contributions
Xinwei Han and Kewei Ren contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Yahua Li, Xiaoyong Ge, Zongming Li, Zihe Zhou, Kunpeng Wu, Yifan Li, Tengfei Ji, Changran Wang, Kefeng Guo, and Jianzhuang Ren. The first draft of the manuscript was written by Yahua Li and Xiaoyong Ge. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All institutional and national guidelines for the care and use of laboratory animals were followed.
Consent for publication
Consent has been asked where appropriate.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, Y., Ge, X., Li, Z. et al. Application of temperature-sensitive liquid embolic agent loaded with oxaliplatin in the TACE procedure for rabbit VX2 gastric cancer. Drug Deliv. and Transl. Res. 14, 705–717 (2024). https://doi.org/10.1007/s13346-023-01425-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01425-5