Abstract
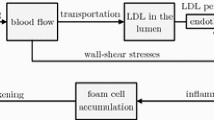
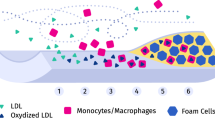
Studying the formation and stability of atherosclerotic plaques in the hemodynamic field is essential for understanding the growth mechanism and preventive treatment of atherosclerotic plaques. In this paper, based on a multiplayer porous wall model, we established a two-way fluid–solid interaction with time-varying inlet flow. The lipid-rich necrotic core (LRNC) and stress in atherosclerotic plaque were described for analyzing the stability of atherosclerotic plaques during the plaque growth by solving advection–diffusion–reaction equations with finite-element method. It was found that LRNC appeared when the lipid levels of apoptotic materials (such as macrophages, foam cells) in the plaque reached a specified lower concentration, and increased with the plaque growth. LRNC was positively correlated with the blood pressure and was negatively correlated with the blood flow velocity. The maximum stress was mainly located at the necrotic core and gradually moved toward the left shoulder of the plaque with the plaque growth, which increases the plaque instability and the risk of the plaque shedding. The computational model may contribute to understanding the mechanisms of early atherosclerotic plaque growth and the risk of instability in the plaque growth.
Graphic abstract
















Similar content being viewed by others
Data availability
All data generated or used during the study appear in the submitted article.
Abbreviations
- C :
-
Concentration
- D :
-
Diffusion coefficient
- ρ:
-
Blood density
- u w :
-
Convection coefficient of the conserved flux
- P :
-
Blood pressure
- μ :
-
Dynamic viscosity
- U :
-
Velocity of the blood
- t :
-
Time
- WSS:
-
Shear stress
- V :
-
Volume
- R :
-
The height of the necrotic core
- L :
-
Length of damage
- Kr:
-
Correction factor
- υ:
-
Poisson’s ratio
- \(\Omega\) :
-
Two-dimensional domain
- \(J\) :
-
Boundary flux
- \(\varepsilon_{p}\) :
-
porosity
- k :
-
Permeability
References
Zhou D, Li J, Liu D, Ji LY, Wang NQ, Jie D, Wang JC, Ye M, Zhao XH (2019) Irregular surface of carotid atherosclerotic plaque is associated with ischemic stroke: a magnetic resonance imaging study. J Geriatr Cardiol 16(12):872–879. https://doi.org/10.11909/j.issn.1671-5411.2019.12.002
Li J, Li D, Yang D, Hang HL, Wu YW, Yao R, Chen XY, Xu YL, Dai W, Zhou D, Zhao XH (2020) Irregularity of carotid plaque surface predicts subsequent vascular event: a MRI study. J Magn Reson Imaging 52(1):185–194. https://doi.org/10.1002/jmri.27038
Lei W, Hu J, Xie Y et al (2023) Mathematical modelling of the effects of statins on the growth of necrotic core in atherosclerotic plaque. Math Model Nat Phenom 18:11–28. https://doi.org/10.1051/mmnp/2023005
Thon MP, Hemmler A, Glinzer A, Mayr M, Widgruber M, Zernecke-Madsen A, Gee MW (2018) A multiphysics approach for modeling early atherosclerosis. Biomech Model Mechanobiol 17:617–644. https://doi.org/10.1007/s10237-017-0982-7
Basak S, Khare HA, Kempen PJ, Kamaly N, Almdal K (2022) Nanoconfined anti-oxidizing RAFT nitroxide radical polymer for reduction of low-density lipoprotein oxidation and foam cell formation. Nanoscale Adv. 4(3):742–753. https://doi.org/10.1039/D1NA00631B
Victoria-Montesinos D, Abellán Ruiz MS, Luque Rubia AJ, Martinez DG, Pérez-Piñero S, Sánchez Macarro M, García-Muñoz AM, García FC, Sánchez JC, López-Román FJ (2021) Effectiveness of consumption of a combination of citrus fruit flavonoids and olive leaf polyphenols to reduce oxidation of low-density lipoprotein in treatment-naive cardiovascular risk subjects: a randomized double-blind controlled study. Antioxidants 10(4):589–599. https://doi.org/10.3390/antiox10040589
Fok PW (2012) Growth of necrotic cores in atherosclerotic plaque. Math Med Biol A J Ima 29(4):301–327. https://doi.org/10.1093/imammb/dqr012
Newby AC, George SJ, Ismail Y, Johnson JL, Sala-Newby GB, Thomas AC (2009) Vulnerable atherosclerotic plaque metalloproteinases and foam cell phenotypes. Thromb Haemost 2009(101):1006–1011. https://doi.org/10.1160/TH08-07-0469
Kedem O, Katchalsky A (1958) Thermodynamic analysis of the permeability of biological membranes to non-electrolytes. Acta Biochim Biophys Sin 27:229–246. https://doi.org/10.1016/0006-3002(58)90330-5
Prosi M, Zunino P, Perktold K, Quarteroni A (2005) Mathematical and numerical models for transfer of low-density lipoproteins through the arterial walls: a new methodology for the model set up with applications to the study of disturbed lumenal flow. J Biomech 38(4):903–917. https://doi.org/10.1016/j.jbiomech.2004.04.024
Knight J, Olgac U, Saur SC, Poulikakos D, Marshall W Jr, Cattin PC, Alkadhi H, Kurtcuoglu V (2010) Choosing the optimal wall shear parameter for the prediction of plaque location—a patient-specific computational study in human right coronary arteries. Atherosclerosis 211(2):445–450. https://doi.org/10.1016/j.atherosclerosis.2010.03.001
Roustaei M, Nikmaneshi MR, Firoozabadi B (2018) Simulation of Low Density Lipoprotein (LDL) permeation into multilayer coronary arterial wall: Interactive effects of wall shear stress and fluid-structure interaction in hypertension. J Biomech 67:114–122. https://doi.org/10.1016/j.jbiomech.2017.11.029
Calvez V, Ebde A, Meunier N, Raoult A (2009) Mathematical modelling of the atherosclerotic plaque formation//Esaim: proceedings. EDP Sciences 28:1–12. https://doi.org/10.1051/proc/2009036
Wong KKL, Thavornpattanapong P, Cheung SCP, Sun ZH, Tu JY (2012) Effect of calcification on the mechanical stability of plaque based on a three-dimensional carotid bifurcation model. BMC Cardiovasc Disord 12:1–18. https://doi.org/10.1186/1471-2261-12-7
Pasqualino G (2019) Pattern formation in atherosclerotic plaques. http://hdl.handle.net/10222/76250. Accessed 26 Feb 2023
Mirzaei NM, Weintraub WS, Fok PW (2020) An integrated approach to simulating the vulnerable atherosclerotic plaque. Am J Physiol Heart Circ Physiol 319(4):H835–H846. https://doi.org/10.1152/ajpheart.00174.2020
Seneviratne AN, Edsfeldt A, Cole JE, Kassiteridi C, Swart M, Park I, Green P, Khoyratty T, Saliba D, Goddard ME, Sansom SN, Goncalves I, Krams R, Udalova IA, Monaco C (2017) Interferon regulatory factor 5 controls necrotic core formation in atherosclerotic lesions by impairing efferocytosis. Circulation 136(12):1140–1154. https://doi.org/10.1161/CIRCULATIONAHA.117.027844
Hao W, Friedman A (2014) The LDL-HDL profile determines the risk of atherosclerosis: a mathematical model. PLoS ONE 9(3):e90497. https://doi.org/10.1371/journal.pone.0090497
Rostam-Alilou AA, Jarrah HR, Zolfagharian A, Bodaghi M (2022) Fluid–structure interaction (FSI) simulation for studying the impact of atherosclerosis on hemodynamics, arterial tissue remodeling, and initiation risk of intracranial aneurysms. Biomech Model Mechanobiol 21:1393–1406. https://doi.org/10.1007/s10237-022-01597-y
Dirksen MT, van der Wal AC, van den Berg FM, van der Loos CM, Becker AE (1998) Distribution of inflammatory cells in atherosclerotic plaques relates to the direction of flow. Circulation 98(19):2000–2003. https://doi.org/10.1161/01.CIR.98.19.2000
Pedrigi RM, Mehta VV, Bovens SM, Mohri Z, Poulsen CB, Gsell W, Tremoleda JL, Towhidi L, Silva RD, Petretto E, Krams R (2016) Influence of shear stress magnitude and direction on atherosclerotic plaque composition. R Soc Open Sci. 3(10):160588. https://doi.org/10.1098/rsos.160588
Jager NA, de WallisVries BM, Hillebrands JL, Harlaar NJ, Tio RA, Slart RHJA, van Dam GM, Boersma HH, Zeebregts CJ, Westra J (2016) Distribution of matrix metalloproteinase in human atherosclerotic carotid plaques and their production by smooth muscle cells and macrophage subsets. Mol Imaging Biol 18:283Y291. https://doi.org/10.1007/s11307-015-0882-0
Morbiducci U, Kok AM, Kwak B, Stone PH, Steinman DA, Wentzel JJ (2016) Atherosclerosis at arterial bifurcations: evidence for the role of haemodynamics and geometry. Thromb Haemost 115(3):484–492. https://doi.org/10.1160/th15-07-0597
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP (2020) Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation 141:e139-596. https://doi.org/10.1161/CIR.0000000000000757
Liu Y, Luo X, Jia H and Yu B. The Effect of Blood Pressure Variability on Coronary Atherosclerosis Plaques. Front Cardiovasc Med. 2022; 9:803810. https://doi.org/10.3389/fcvm.2022.803810
Jarrah HR, Zolfagharian A, Bodaghi M (2022) Finite element modeling of shape memory polyurethane foams for treatment of cerebral aneurysms. Biomech Model Mechanobiol 21:383–399. https://doi.org/10.1007/s10237-021-01540-7
Sugiyama S, Niizuma K, Nakayama T, Shimizu H, Endo H, Inoue T, Fujimura M, Ohta M, Takahashi A, Tominaga T (2013) Relative residence time prolongation in intracranial aneurysms: a possible association with atherosclerosis. Neurosurgery 73(5):767–776. https://doi.org/10.1227/NEU.0000000000000096
He F, Hua L, Gao L (2017) Computational analysis of blood flow and wall mechanics in a model of early atherosclerotic artery. J Mech Sci Technol 31:1015–1020. https://doi.org/10.1007/s12206-017-0154-9
Ahmadpour-B M, Nooraeen A, Tafazzoli-Shadpour M, Taghizadeh H (2021) Contribution of atherosclerotic plaque location and severity to the near-wall hemodynamics of the carotid bifurcation: an experimental study and FSI modeling. Biomech Model Mechanobiol 20:1069–1085. https://doi.org/10.1007/s10237-021-01431-x
Wang H, Uhlmann K, Vedula V, Balzani D, Varnik F (2022) Fluid-structure interaction simulation of tissue degradation and its effects on intra-aneurysm hemodynamics. Biomech Model Mechanobiol 21(2):671–683. https://doi.org/10.1007/s10237-022-01556-7
Ebrahimi S, Fallah F (2022) Investigation of coronary artery tortuosity with atherosclerosis: a study on predicting plaque rupture and progression. Int J Mech Sci 223:107295. https://doi.org/10.1016/j.ijmecsci.2022.107295
Dhawan SS, Avati Nanjundappa RP, Branch JR, Taylor WR, Quyyumi AA, Jo H, McDaniel MC, Suo J, Giddens D, Samady H (2010) Shear stress and plaque development. Expert Rev Cardiovasc Ther 8(4):545–556. https://doi.org/10.1586/erc.10.28
Chalmers AD, Bursill CA, Myerscough MR (2017) Nonlinear dynamics of early atherosclerotic plaque formation may determine the efficacy of high-density lipoproteins (HDL) in plaque regression. PLoS ONE 12(11):e0187674. https://doi.org/10.1371/journal.pone.0187674
Linsel-Nitschke P, Tall AR (2005) HDL as a target in the treatment of atherosclerotic cardio vascular disease. Nat Rev Drug Discovery 4(3):193–205. https://doi.org/10.1038/nrd1658
Chalmers AD, Cohen A, Bursill CA, Myerscough MR (2015) Bifurcation and dynamics in a mathematical model of early atherosclerosis. J Math Biol 71:1451–1480. https://doi.org/10.1007/s00285-015-0864-5
Bulelzai MAK, Dubbeldam JLA (2012) Long time evolution of atherosclerotic plaques. J Theor Biol 297:1–10. https://doi.org/10.1016/j.jtbi.2011.11.023
Carvalho V, Carneiro F, Ferreira AC, Gama V, Teixeira JC, Teixeira S (2021) Numerical study of the unsteady flow in simplified and realistic iliac bifurcation models. Fluids 6(8):284–302. https://doi.org/10.3390/fluids6080284
Cilla M, Pena E, Martinez MA (2014) Mathematical modelling of atheroma plaque formation and development in coronary arteries. J R Soc Interface 11(90):20130866. https://doi.org/10.1098/rsif.2013.0866
Hariharan P, Nabili M, Guan A, Zderic V, Myers M (2017) Model for porosity changes occurring during ultrasound-enhanced transcorneal drug delivery. Ultrasound Med Biol 43(6):1223–1236. https://doi.org/10.1016/j.ultrasmedbio.2017.01.013
Cheema TA, Kim GM, Lee CY, Hong JG, Kwak MK, Park CW (2014) Characteristics of blood vessel wall deformation with porous wall conditions in an aortic arch. Appl Rheol 24(2):17–24. https://doi.org/10.3933/applrheol-24-24590
Palombo C, Kozakova M (2016) Arterial stiffness, atherosclerosis and cardiovascular risk: pathophysiologic mechanisms and emerging clinical indications. Vascul Pharmacol 77:1–7. https://doi.org/10.1016/j.vph.2015.11.083
Tang D, Yang C, Kobayashi S, Zheng J, Woodard PK, Teng ZZ, Billiar K, Bach R, Ku DN (2019) 3D MRI-based anisotropic FSI models with cyclic bending for human coronary atherosclerotic plaque mechanical analysis. J Biomech Eng 131(6):061010. https://doi.org/10.1115/1.3127253
Silva T, Jäger W, Neuss-Radu M, Sequeira A (2020) Modeling of the early stage of atherosclerosis with emphasis on the regulation of the endothelial permeability. J Theor Biol 496:496–515. https://doi.org/10.1016/j.jtbi.2020.110229
Chen C, Gu Y, Tu J, Guo X, Zhang D (2016) Microbubble oscillating in a microvessel filled with viscous fluid: a finite element modeling study. Ultrasonics 66:54–64. https://doi.org/10.1016/j.ultras.2015.11.010
Kirillova IV, Kossovich EL, Safonov RA, Chelnokova NO, Golyadkina AA; Shevtsova MS (2016) Finite Element Modeling of Atherosclerotic Plaque Evolution vol 3. 2016 3rd International Conference on Information Science and Control Engineering (ICISCE) IEEE. pp 973–977. https://doi.org/10.1109/ICISCE.2016.211
Ball RY, Stowers EC, Burton JH, Cary NRB, Skepper JN, Mitchinson MJ (1995) Evidence that the death of macrophage foam cells contributes to the necrotic core of atheroma. Atherosclerosis 114(1):45–54. https://doi.org/10.1016/0021-9150(94)05463-
Yuan Y, Li P, Ye J (2012) Lipid homeostasis and the formation of macrophage-derived foam cells in atherosclerosis. Protein Cell 3(3):173–181. https://doi.org/10.1007/s13238-012-2025-6
Lei W, Hu J, Liu Y, Liu W, Chen XK (2021) Numerical evaluation of high-intensity focused ultrasound-induced thermal lesions in atherosclerotic plaques. Math Biosci Eng 18:1154–1168. https://doi.org/10.3934/mbe.2021062
Esterbauer H, Striegl G, Puhl H, Rotheneder M (1989) Continuous monitoring of in vitro oxidation of human low density lipoprotein. Free Radical Res 6(1):67–75. https://doi.org/10.3109/10715768909073429
Schiesser WE (2018) PDE models for atherosclerosis computer implementation in R. J. synthesis lectures on biomedical engineering. Biomed Eng Lett 11:1–141. https://doi.org/10.2200/S00877ED1V01Y201810MAS022
Kruth HS, Huang W, Ishii I, Zhang WY (2002) Macrophage foam cell formation with native low-density lipoprotein. J Biol Chem 77(37):34573–34580. https://doi.org/10.1074/jbc.M205059200
Taylor BA, Panza G, Pescatello LS, Chipkin S, Gipe D, Shao WP, White CM, Thompson PD (2014) Serum PCSK9 levels distinguish individuals who do not respond to high-dose statin therapy with the expected reduction in LDL-C. J Lipids. 2014:140723. https://doi.org/10.1155/2014/140723
Akyildiz AC, Speelman L, Brummelen VH, Gutiérrez MA, Virmani R, Lugt AV, van der Steen FWA, Wentzel JJ, Gijsen F (2011) Effects of intima stiffness and plaque morphology on peak cap stress. Biomed Eng Online 10:1–13. https://doi.org/10.1186/1475-925X-10-25
Xie J, Zhou J, Fung YC (1995) Bending of blood vessel wall: stress-strain laws of the intima-media and adventitial layers. J Biomech Sci Eng 1(136):136–145. https://doi.org/10.1115/1.2792261
Khanafer K, Berguer R (2009) Fluid–structure interaction analysis of turbulent pulsatile flow within a layered aortic wall as related to aortic dissection. J biomech 42(16):2642–2648. https://doi.org/10.1016/j.jbiomech.2009.08.010
Chen XK, Hu XY, Jia P, Xie ZX, Liu J (2021) Tunable anisotropic thermal transport in porous carbon foams: The role of phonon coupling. Int J Mech Sci 306:106576. https://doi.org/10.1016/j.ijmecsci.2021.106576
Sun J, Balu N, Hippe DS, Xue YJ, Dong L, Zhao XH, Li FY, Xu DX, Hatsukami TS, Yuan C (2013) Subclinical carotid atherosclerosis: short-term natural history of lipid-rich necrotic core—a multicenter study with MR imaging. Radiology 268(1):61–68. https://doi.org/10.1148/radiol.13121702
Chang HJ, Lin FY, Lee SE et al (2018) Coronary atherosclerotic precursors of acute coronary syndromes. J Am Coll Cardiol 71(22):2511–2522. https://doi.org/10.1016/j.jacc.2018.02.079
Getz GS, Reardon CA (2012) Animal models of atherosclerosis. Prog Mol Biol Transl Sci 32(5):1–23. https://doi.org/10.1016/B978-0-12-394596-9.00001-9
Feuchtner G, Langer C, Barbieri F, Beyer C, Dichtl WG, Friedrich G, Schgoer W, Widmann G, Plank F (2021) The effect of omega-3 fatty acids on coronary atherosclerosis quantified by coronary computed tomography angiography. Clin Nutr 40(3):1123–1129. https://doi.org/10.1016/j.clnu.2020.07.016
Zhao X, Hippe DS, Li R, Canton GM, Sui BB, Song Y, Li FY, Xue YJ, Sun J, Yamada K, Hatsukami TS, Xu DX, Wang MX, Yuan C (2017) Prevalence and characteristics of carotid artery high-risk atherosclerotic plaques in Chinese patients with cerebrovascular symptoms: a Chinese atherosclerosis risk evaluation II study. J Am Heart Assoc 6(8):e005831. https://doi.org/10.1161/JAHA.117.005831
Virmani R, Kolodgie FD, Burke AP, Finn AV, Gold HK, Tulenko TN, Wrenn SP, Narula J (2005) Atherosclerotic plaque progression and vulnerability to rupture: angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol 25(10):2054–2061. https://doi.org/10.1161/01.ATV.0000178991.71605.18
Li AC, Glass CK (2002) The macrophage foam cell as a target for therapeutic intervention. Nat Med 8(11):1235–1242. https://doi.org/10.1038/nm1102-1235
Tash OA, Razavi SE (2012) Numerical investigation of pulsatile blood flow in a bifurcation model with a non-planar branch: the effect of different bifurcation angles and non-planar branch. Bioimpacts 2(4):195–205. https://doi.org/10.5681/bi.2012.023
Velican D, Velican C (1989) Coronary anatomy and microarchitecture as related to coronary atherosclerotic involvement. Med Interne 27(4):257–262. https://doi.org/10.1007/978-0-387-76852-6_4
Nishizawa A, Suemoto CK, Farias-Itao DS, Campos FM, Karen C, Silva S, Bittencourt MS, Grinberg LT, Leite REP, Ferretti-Rebustini REL, Farfel JM, Jacob-Filho W, Pasqualucci CA (2017) Morphometric measurements of systemic atherosclerosis and visceral fat: Evidence from an autopsy study. PLoS ONE 12(10):e0186630. https://doi.org/10.1371/journal.pone.0186630
Wang X, Ge J (2021) Haemodynamics of atherosclerosis: a matter of higher hydrostatic pressure or lower shear stress? Cardiovasc Res 117(4):e57–e59. https://doi.org/10.1093/cvr/cvab001
Meng H, Tutino VM, Xiang J, Siddiqui A (2014) High WSS or low WSS? Complex interactions of hemodynamics with intracranial aneurysm initiation, growth, and rupture: toward a unifying hypothesis. Am J Neuroradiol 35(7):1254–1262. https://doi.org/10.3174/ajnr.A3558
Xiong H, Liu X, Tian X, Pu L, Zhang HY, Lu MH, Huang WH, Zhang YT (2014) A numerical study of the effect of varied blood pressure on the stability of carotid atherosclerotic plaque. Biomed Eng Online 13(1):1–13. https://doi.org/10.1186/1475-925X-13-152
Manning-Tobin JJ, Moore KJ, Seimon TA, Bell SA, Sharuk M, Alvarez-Leite JI, Menno P, Winther JD, Tabas I, MasonFreeman W (2009) Loss of SR-A and CD36 activity reduces atherosclerotic lesion complexity without abrogating foam cell formation in hyperlipidemic mice. Arterioscler Thromb Vasc Biol 29(1):19–26. https://doi.org/10.1161/ATVBAHA.108.176644
Yang S, Wang Q, Shi W, Guo WC, Jiang ZI, Gong XB (2019) Numerical study of biomechanical characteristics of plaque rupture at stenosed carotid bifurcation: a stenosis mechanical property-specific guide for blood pressure control in daily activities. Acta Mech Sin 35:1279–1289. https://doi.org/10.1007/s10409-019-00883-w
Campbell IC, Weiss D, Suever JD, Virmani R, Veneziani A, Vito RP, Oshinski JN, Taylor WR (2013) Biomechanical modeling and morphology analysis indicates plaque rupture due to mechanical failure unlikely in atherosclerosis-prone mice. Am J Physiol Heart Circ Physiol 304(3):H473–H486. https://doi.org/10.1152/ajpheart.00620.2012
Pu L, Xiong H, Liu X (2014) Quantifying effect of blood pressure on stress distribution in atherosclerotic plaque. Int Conf Health Informaticsy 42(1):P216–P219. https://doi.org/10.1007/978-3-319-03005-0_55
Huang Y, Teng ZZ, Sadat U, Graves MJ, Bennett MR, Gillard JH (2014) The influence of computational strategy on prediction of mechanical stress in carotid atherosclerotic plaques: Comparison of 2D structure-only, 3D structure-only, one-way and fully coupled fluid-structure interaction analyses. J Biomech 47(6):1465–1471. https://doi.org/10.1016/j.jbiomech.2014.01.030
Manduteanu I, Simionescu M (2012) Inflammation in atherosclerosis: a cause or a result of vascular disorders? J Cell Mol Med 16(9):1978–1990. https://doi.org/10.1111/j.1582-4934.2012.01552.x
Fuchs FD, Whelton PK (2020) High blood pressure and cardiovascular disease. Hypertension 75(2):285–329. https://doi.org/10.1161/HYPERTENSIONAHA.119.14240
Eshtehardi P, Mcdaniel MC, Suo J, Dhawan SS, Timmins LH, Binongo JNG, Golub LJ, Corban MT, Finn AV, Oshinski JN (2012) Association of coronary wall shear stress with atherosclerotic plaque burden, composition, and distribution in patients with coronary artery disease. J Am Heart Assoc 1(4):e002543. https://doi.org/10.1161/JAHA.112.002543
Cecchi E, Giglioli C, Valente S, Lazzeri C, Gensini GF, Gensini R, Gensini L (2011) Role of hemodynamic shear stress in cardiovascular disease. Atherosclerosis 214(2):249–256. https://doi.org/10.1016/j.atherosclerosis.2010.09.008
Kim S, Giddens DP (2015) Thrombosis formation on atherosclerotic lesions and plaque rupture. J Biomech Sci Eng 137(4):0410071–04100711. https://doi.org/10.1111/joim.12296
Wang LM, Hu JW, Lei WR, Liu WY, Liu YT (2019) Mechanical stress analysis of defects in atherosclerotic plaque. J Anhui Normal Univ. 42(6):538–543. https://doi.org/10.14182/J.cnki.1001-2443.2019.06.006
Li ZY, Howarth S, Tang T, Martin G, Jean Marie UK, Jonathan G (2007) Does calcium deposition play a role in the stability of atheroma? Location may be the key. Cerebrovasc Dis 24(5):452–459. https://doi.org/10.1159/000108436
Theofilatos K, Stojkovic S, Hasman M, Baig F, Barallobre-Barreiro J, Schmidt L, Yin S, Yin X, Burnap S, Singh B (2022) A proteomic atlas of atherosclerosis: regional proteomic signatures for plaque inflammation and calcification. Cardiovasc Res. https://doi.org/10.1093/cvr/cvac066.204
Bajaj R, Eggermont J, Grainger SJ, Raber L, Parasa R, Khan AHA, Costa C, Erdogan E, Hendricks MJ, Chandrasekharan KH (2022) Machine learning for atherosclerotic tissue component classification in combined near-infrared spectroscopy intravascular ultrasound imaging: validation against histology. Atherosclerosis. https://doi.org/10.1016/j.atherosclerosis.2022.01.021
Acknowledgements
This study was supported by the National Nature Science Foundation of China (No.12274200、11774088) and Hengyang science and technology plan projects (No.202250045335).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declared that no conflict of interest among all authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lei, W., Qian, S., Zhu, X. et al. Haemodynamic Effects on the Development and Stability of Atherosclerotic Plaques in Arterial Blood Vessel. Interdiscip Sci Comput Life Sci 15, 616–632 (2023). https://doi.org/10.1007/s12539-023-00576-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12539-023-00576-w