Abstract
Introduction
Polymorphism ABCG2 c.421C>A (rs2231142) results in reduced activity of the important drug efflux transporter breast cancer-resistance protein (BCRP/ABCG2). One study has suggested that it may affect enterohepatic recirculation of mycophenolic acid (MPA). We evaluated the effect of rs2231142 on steady-state exposure to MPA in renal transplant recipients.
Methods
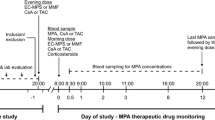
Consecutive, stable adult (age ≥ 16 years) renal transplant recipients on standard MPA-based immunosuppressant protocols (N = 68; 43 co-treated with cyclosporine, 25 with tacrolimus) underwent routine therapeutic drug monitoring after a week of initial treatment, and were genotyped for ABCG2 c.421C>A and 11 polymorphisms in genes encoding enzymes and transporters implicated in MPA pharmacokinetics. ABCG2 c.421C>A variant versus wild-type (wt) patients were matched with respect to demographic, biopharmaceutic, and genetic variables (full optimal combined with exact matching) and compared for dose-adjusted steady-state MPA pharmacokinetics [frequentist and Bayes (skeptical neutral prior) estimates of geometric means ratios, GMR].
Results
Raw data (12 variant versus 56 wt patients) indicated around 40% higher total exposure (frequentist GMR = 1.45, 95% CI 1.10–1.91; Bayes = 1.38, 95% CrI 1.07–1.81) and around 30% lower total body clearance (frequentist GMR = 0.66, 0.58–0.90; Bayes = 0.71, 0.53–0.95) in variant carriers than in wt controls. The estimates were similar in matched data (11 variant versus 43 wt patients): exposure GMR = 1.41 (1.11–1.79) frequentist, 1.39 (1.15–1.81) Bayes, with 90.7% and 85.5% probability of GMR > 1.20, respectively; clearance GMR = 0.73 (0.58–0.93) frequentist, 0.71 (0.54–0.95) Bayes. Sensitivity analysis indicated low susceptibility of the estimates to unmeasured confounding.
Conclusions
Loss-off-function polymorphism ABCG2 c.421C>A increases steady-state exposure to MPA in stable renal transplant patients.



Similar content being viewed by others
References
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of mycophenolate in solid organ transplant recipients. Clin Pharmacokinet. 2007;46:13–58.
Tett SE, Saint-Marcoux F, Staatz CE, Brunet M, Vinks AA, Miura M, et al. Mycophenolate, clinical pharmacokinetics, formulations, and methods for assessing drug exposure. Transplant Rev. 2011;5:47–57.
Lamba V, Sanhavi K, Fish A, Altman RB, Klein TE. PharmGKB summary: mycophenolic acid pathway. Pharmacogenet Genom. 2014;24:73–9.
Dalla VecchiaGenvigir F, Cerda A, Dominguez Crespo Hirata T, Hirata MH, Hirata DC. Mycophenolic acid pharmacogenomics in kidney transplantation. J Transl Genet Genom. 2020;4:320–55.
Bergan S, Brunet M, Hesselink DA, Johnson-Davis KL, Kunicki PK, Lemaitre F, et al. Personalized therapy for mycophenolate: consensus report by the International association on therapeutic drug monitoring and clinical toxicology. Ther Drug Monit. 2021;43:150–200.
Giacomini KM, Huang SM, Tweedie DJ, Benet LZ, Brouwer KL, Chu X, et al. International transporter consortium: membrane transporters in drug development. Nat Rev Drug Discov. 2010;9:215–36.
Giacomini KM, Balimane PV, Cho SK, Eadon M, Edeki T, Hillgren KM, et al. International transporter consortium commentary on clinically important transporter polymorphisms. Clin Pharmacol Ther. 2013;94:23–6.
Foher AE, Brackman DJ, Giacomini KM, Altman RB, Klein TE. Pharm GKB summary: very important pharmacogene information for ABCG2. Pharmacogenet Genom. 2017;27:420–7.
Kondo C, Suzuki H, Itoda M, Ozawa S, Kobayashi D, et al. Functional analysis of SNPs variants of BCRP/ABCG2. Pharm Res. 2004;21:1895–903.
Furukawa T, Wakabayashi K, Tamura A, Nakagawa H, Morishima Y, Osawa Y, et al. Major SNP (Q141K) variant of human ABC transporter ABCG2 undergoes lysosomal and proteosomal degradations. Pharm Res. 2009;26:469–79.
Miura M, Kagaya H, Satoh S, Inoue K, Saito M, Habuchi T, Suzuki T. Influence of drug transporters and UGT polymorphisms on pharmacokinetics of phenolic glucuronide metabolite of mycophenolic acid in Japanese renal transplant recipients. Ther Drug Monit. 2008;30:559–64.
Trkulja V, Lalić Z, Nađ-Škegro S, Lebo A, Granić P, Lovrić M, et al. Effect of cyclosporine on steady-state pharmacokinetics of MPA in renal transplant recipients is not affected by the MPA formulation: analysis based on therapeutic drug monitoring data. Ther Drug Monit. 2014;36:456–64.
Božina N, Lalić Z, NađŠkegro S, Borić-Bilušić A, Božina T, Kaštelan Ž, Trkulja V. Steady-state pharmacokinetics of mycophenolic acid in renal transplant patients: exploratory analysis of the effects of cyclosporine, recipients’ and donors’ ABCC2 gene variants and their interactions. Eur J Clin Pharmacol. 2017;73:1129–40.
Hu DG, Meech R, Lu L, McKinnon RA, Mackenzie PI. Polymorphisms and haplotypes of the UDP-glucuronosyltransferase 2B7 gene promoter. Drug Metab Dispos. 2014;42:854–62.
Pearl J. Causality: models, reasoning and inference. 2nd ed. Cambridge: Cambridge University Press; 2009.
Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2016;42:514–20.
VenderWeele TJ, Rothman KJ, Lash TL. Confounding and confounders. In: Lash TL, VanderWeele TJ, Haneuse S, Rothman KJ, editors. Modern epidemiology. 4th ed. Philadephia: Wolters Kluwver; 2021. p. 610–67.
Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Elliot GTH. Robust causal inference using directed acyclic graphs: the R package “dagitty.” Int J Epidemiol. 2016;45:1887–94.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2020.
Endrenyi L, Gritsch S, Yan W. Cmax/AUC is a clearer measure than Cmax for absorption rates in investigations of bioequivalence. Int J Clin Pharmacol Ther Toxicol. 1991;29:394–9.
Ho DE, Imai K, King G, Stuart EA. MatchIT: nonparmetric preprocessing for parametric causal inference. J Stat Software. 2011;42:1–28. https://doi.org/10.18637/jss.v042.i08.
Hansen BB, Olsen KS. Optimal full matching and related designs via network flows. J Comput Global Stat. 2006;15:609–27.
King G, Nielsen R. Why propensity scores should not be used for matching. Polit Anal. 2019;27:435–54.
Goodrich B, Gabry J, Ali I, Brilleman S. rstanarm: Bayesian applied regression modeling via Stan. R package version 2.21.3, 2022, https://mc-stan.org/rstanarm/
Gaunt TR, Rodríguez S, Day IN. Cubic exact solutions for the estimation of pairwise haplotype frequencies: implications for linkage disequilibrium analyses and a web tool “CubeX.” BMC Bioinform. 2007;8(1):428. https://doi.org/10.1186/1471-2105-8-428.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–74.
Schneeweiss S. Sensitivity analysis and external adjustment for unmeasured confounders in epidemiological database studies of therapeutics. Pharmacoepidemol Drug Saf. 2006;15:291–303.
Haine D. The episensr package: basic sensitivity analysis of epidemiological results. https://doi.org/10.5281/zenodo.4554553, R package version 1.1.0, https://dhaine.github.io/episensr
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Friedrich JO, Adhikari NKJ, Beyene J. The ratio of means method as an alternative to mean differences for analyzing continuous outcome variables in meta-analysis: a simulation study. BMC Med Res Methodol. 2008;8:32. https://doi.org/10.1186/1471-2288-8-32.
Boumar R, Hessenlink DA, van Schaik RHN, Weimar W, van der Heiden I, de Fijter JW, et al. Mycophenolic acid-related diarrhea is not associated with polymorphisms in SLCO1B nor with ABCB1 in renal transplant recipients. Pharmacogen Genom. 2012;22:399–407.
van Schaik RHN, van Agteren M, de Fijter JW, Hartmann A, Schmidt J, Budde K, et al. UGT1A9 -275T>A/-2152C>T polymorphisms correlate with low MPA exposure and acute rejection in MMF/tacrolimus-treated kidney transplant patients. Clin Pharmacol Ther. 2009;86:319–27.
Picard N, Yee SW, Woillard JB, Lebranchu Y, Le Meur Y, Giacomini KM, Marquet P. The role of organic antion-transporting polypeptides and their common genetic variants in mycophenolic acid pharmacokinetics. Clin Pharm Ther. 2010;87:100–8.
Geng F, Jiao Z, Dao YJ, Qiu XY, Ding JJ, Shi X, et al. The association of the UGT1A8, SLCO1B3 and ABCC2/ABCG2 genetic polymorphisms with the pharmacokinetics of mycophenolic aid and its phenolic glucuronide metabolite in Chinese individuals. Clin Chim Acta. 2012;423:683–90.
Miura M, Satoh S, Inoue K, Kagaya H, Saito M, Inoue M, et al. Influence of SLCO1B1, 1B3, 2B1 and ABCC2 genetic polymorphisms on mycophenolic acid pharmacokinetics in Japanese renal transplant recipients. Eur J Clin Pharmacol. 2007;63:1161–9.
Bernard O, Cuillemette C. The main role of UGT1A9 in the hepatic metabolism of mycophenolic acid and the effectsof naturally occurring variants. Drug Metab Dispos. 2004;32:775–8.
Kuypers DR, Naesens M, Vermeire S, Vanrentghem Y. The impact of uridine diphosphate-glucuronosyltrasferase 1A9 (UGT1A9) gene promoter region single-nucleotide polymorphisms T-275A and C-2152T on early mycophenolic acid dose-interval exposure in de novo renal allograft recipients. Clin Pharmacol Ther. 2005;78:351–61.
Zhao W, Fakhoury M, Deschenes G, Roussey G, Brochard K, Niaudet P, et al. Population pharmacokinetics and pharmacogenetics of mycophenolic acid following administration of mycophenolate mofetil in de novo pediatric renal transplant patients. J Clin Pharmacol. 2010;50:1280–91.
Yang CI, Shen CC, Liao GY, Yong S, Feng LJ, Xia Q, et al. Genetic polymorphisms in metabolic enzymes and transporters have no impact on mycophenolic acid pharmacokinetics in adult kindey transplant patients co-treated with tacrolimus: a population analysis. J Clin Pharm Ther. 2021;00:1–12. https://doi.org/10.1111/jcpt.13488.
UGT alleles Nomenclature. Available at https://www.pharmacogenomics.pha.ulaval.ca/ugt-alleles-nomenclature/ (last accessed July 11, 2022)
Takuathung MN, Sakuludomkan W, Koonrungsesomboon N. The impact of genetic polymorphisms on the pharmacokinetics and pharmacodynamics of mycophenolic acid: systematic review and meta-analysis. Clin Pharmacokinet. 2021;60:1291–302.
Wolking S, Schaeffeler E, Lerche H, Schwab M, Nies AT. Impact of genetic polymorphisms of ABCB1 (MDR1, P-glycoprotein) on drug disposition and potential clinical implications: update of the literature. Clin Pharmacokinet. 2015;54:709–35.
Bruckmueller H, Cascorbi I. ABCB1, ABCG2, ABCC1, ABCC2 and ABCC3 drug transporter polymorphisms and their impact on drug bioavailability: what is our current understanding. Exp Opin Drug Metab Toxicol. 2021;17:369–96.
Barbarino JM, Staatz CE, Venkataramanan R, Klein TE, Altman RB. PharmGKB summary: cyclosporine and tacrolimus pathways. Pharmacogenet Genomics. 2013;23:563–85.
Gupta A, Dai Y, Vethanayagam RR, Herber MF, Thummel KE, Unadkat JD, et al. Cyclosporin A, tacrolimus and sirolimus are potent inhibitors of the human breast cancer resistance protein (ABCG2) and reverse resistance to mitoxantrone and topotecan. Cancer Chemother Pharmacol. 2006;58:374–83.
Bakhsheshian J, Hall MD, Robey RW, Herrmann MA, Chen JQ, Bates SE, Gottesman MM. Overlapping substrate and inhibitor specificity of human and murine ABCG2. Drug Metab Dispos. 2013;41:1805–12.
Li LQ, Chen DN, Li CJ, Li QP, Chen Y, Fang P, et al. Impact of UGT2B7 and ABCC2 genetic polymorphisms on mycophenolic acid metabolism in Chinese renal transplant recipients. Pharmacogenomics. 2018;19:1323–34.
Dalla VecchiaGenvigir F, Campus-Salazar AB, Rosso Felipe C, Tedesco-Silv H, Medina-Pestana JO, de Quateli DS, et al. CYP3A5*3 and CYP2C8*3 variants influence exposure and clinical outcomes of tacrolimus-based therapy. Pharmacogenomics. 2020;21:7–21.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Ana Borić Bilušić, Nada Božina, Zdenka Lalić, Mila Lovrić, Sandra Nađ-Škegro, Luka Penezić, Karmela Barišić and Vladimir Trkulja have nothing to disclose.
Compliance with Ethics Guidelines
Study was approved by the Ethics Committee of the University Hospital Center Zagreb (approval No. 8.1-17/242-2 02/21, January 30, 2018). All procedures performed in the study were in accordance with the 1964 Declaration of Helsinki and its later amendments. All patients included in the present analysis underwent standard routine therapeutic drug monitoring in their post-transplant period. Those meeting inclusion criteria were included only if they signed an informed consent for genotyping of pharmacogenes for research purposes.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Borić-Bilušić, A.A., Božina, N., Lalić, Z. et al. Loss of Function ABCG2 c.421C>A (rs2231142) Polymorphism Increases Steady-State Exposure to Mycophenolic Acid in Stable Renal Transplant Recipients: An Exploratory Matched Cohort Study. Adv Ther 40, 601–618 (2023). https://doi.org/10.1007/s12325-022-02378-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-022-02378-w