Abstract
Objective
To develop regression equations to predict forced oscillation technique (FOT) parameters in Indian children and adolescents.
Methods
Lung function was assessed in a multigeographic cohort of residential school children using a portable FOT-based device (PulmoScan) and spirometry. FOT measurements were performed in 1497 study participants, aged 9–19 y, from 8 Indian districts. Bland–Altman analysis was performed for additional 32 adult subjects to compare the results of PulmoScan to a standard IOS device in an outpatient setting. Reference equations were developed for Rrs and Xrs from the data of healthy subjects with normal spirometry using multivariate regression model for Indo-European, Dravidian, and mixed ethnic groups.
Results
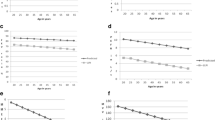
X5 (bias = 0.02) showed a better agreement than resistance parameters (R5 bias = 0.75, R20 bias = −0.22) in IOS/PulmoScan comparison. Anthropometric variables (age, height, and weight) were positively correlated with reactance (X5) and negatively with resistance parameters (R5, R10, R15, and R20), with most associations being stronger in boys. Final regression model considered ethnicity as a key determinant along with anthropometry.
Conclusion
Multiethnic reference equations were developed for Indian children aged 9–19 y based on a novel handheld FOT device.



Similar content being viewed by others
Data Availability
Deidentified categorized data of the participants can be provided on request basis after approval of ethics committee of the institute/organization to which the requesting person belongs, stating the potential need and usage and signing of an agreement with the corresponding authors on behalf of CSIR-IGIB. The request could be made to the corresponding authors after 90 d of publication and the final data used for developing equations will be provided on as it is basis after deanonymization.
References
World Health Organization. Asthma. World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/asthma. Accessed on 15 April 2021.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Deepak D, Prasad A, Atwal SS, Agarwal K. Recognition of small airways obstruction in asthma and COPD - the road less travelled. J Clin Diagn Res. 2017;11:TE01–5.
Dubois AB, Brody AW, Lewis DH, Burgess BF Jr. Oscillation mechanics of lungs and chest in man. J Appl Physiol. 1956;8:587–94.
Shirai T, Kurosawa H. Clinical application of the forced oscillation technique. Intern Med. 2016;55:559–66.
Starczewska-Dymek L, Bożek A, Dymek T. Application of the forced oscillation technique in diagnosing and monitoring asthma in preschool children. Adv Respir Med. 2019;87:26–35.
Ribeiro CO, Faria ACD, Lopes AJ, de Melo PL. Forced oscillation technique for early detection of the effects of smoking and COPD: contribution of fractional-order modeling. Int J Chron Obstruct Pulmon Dis. 2018;13:3281–95.
Li LY, Yan TS, Yang J, et al. Impulse oscillometry for detection of small airway dysfunction in subjects with chronic respiratory symptoms and preserved pulmonary function. Respir Res. 2021;22:68.
Butzko RP, Sotolongo AM, Helmer DA, et al. Forced oscillation technique in veterans with preserved spirometry and chronic respiratory symptoms. Respir Physiol Neurobiol. 2019;260:8–16.
De S, Banerjee N, Kushwah GDS, Dharwey D. Regression equations of respiratory impedance of Indian adults measured by forced oscillation technique. Lung India. 2020;37:30–6.
De S, Banerjee N, Tiwari RR. Regression equations of respiratory impedance measured by forced oscillation technique for Indian children. Indian J Pediatr. 2020;87:192–9.
Aggarwal M, Singh S, Bansal A, Desiraju BK, Agrawal A. Screening of cardiovascular risk assessment accuracy of anthropometric indices in Indian children and adolescents. Wellcome Open Res. 2020. https://doi.org/10.12688/wellcomeopenres.16385.1.
Aggarwal M, Bansal A, Desiraju BK, Singh S, Agrawal A. Determinants of adolescent lung function in Indians: race, nutrition and systemic inflammation. Am J Respir Crit Care Med. 2021;204:1109–11.
Indian Genome Variation Consortium. The Indian genome variation database (IGVdb): a project overview. Hum Genet. 2005;118:1–11.
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Quanjer PH, Stanojevic S, Cole TJ. ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function, et al 2012 equations. Eur Respir J. 2012;40;1324:1343
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Ram J, Pineda-Cely J, Calhoun WJ. Forced oscillometry: a new tool for assessing airway function-is It ready for prime time? J Allergy Clin Immunol Pract. 2019;7:2861–2.
Desai U, Joshi JM. Impulse oscillometry. Adv. Respir Med. 2019;87:235–8.
Kalchiem-Dekel O, Hines SE. Forty years of reference values for respiratory system impedance in adults: 1977–2017. Respir Med. 2018;136:37–47.
Frei J, Jutla J, Kramer G, Hatzakis GE, Ducharme FM, Davis GM. Impulse oscillometry: reference values in children 100 to 150 cm in height and 3 to 10 years of age. Chest. 2005;128:1266–73.
Ducharme FM, Davis GM, Ducharme GR. Pediatric reference values for respiratory resistance measured by forced oscillation. Chest. 1998;113:1322–8.
Oostveen E, Boda K, van der Grinten CP, et al. Respiratory impedance in healthy subjects: baseline values and bronchodilator response. Eur Respir J. 2013;42:1513–23.
Gupta S, Kabra SK. Indigenous regression equations for forced oscillation technique - a much needed affair. Indian J Pediatr. 2020;87:173–4.
Majumder PP, Basu A. A genomic view of the peopling and population structure of India. Cold Spring Harb Perspect Biol. 2014;7:a008540.
Dandurand RJ, Lavoie J-P, Lands LC, Hantos Z. Comparison of oscillometry devices using active mechanical test loads. ERJ Open Research. 2019. Available at: https://openres.ersjournals.com/content/5/4/00160-2019. Accessed on 1 Sept 2021.
Paredi P, Goldman M, Alamen A, et al. Comparison of inspiratory and expiratory resistance and reactance in patients with asthma and chronic obstructive pulmonary disease. Thorax. 2010;65:263–7.
Acknowledgements
MA would like to acknowledge CSIR for fellowship. AA and VS would like to acknowledge Wellcome Trust DBT India Alliance IA/CPHS/ 14/1/501489, Indo-US S&T Forum grant USISTEF/HI-011/2015-16 and CSIR MLP 5502 for support of this work. MA, AA and VS would like to acknowledge Anubhuti Bansal and Shailendra for their contribution in data collection.
Funding
Wellcome Trust, CSIR and USISTEF. The sponsor of this study had no role in study design, data collection, data analysis, data interpretation, or writing of this report.
Author information
Authors and Affiliations
Contributions
AA and VS conceived the objectives; MA collected the data; MA, VS, AA, and NMG did the primary analysis; VS and MA wrote the first draft; AA and NMG reviewed and edited the manuscript. AA will act as the guarantor for this paper.
Corresponding authors
Ethics declarations
Ethics Approval
The study protocol was approved by the institutional human ethics committee of CSIR-IGIB, New Delhi.
Conflict of Interest
MA, NM and VS declare no conflict of interest. AA is a part of the development team of Pulmoscan.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aggarwal, M., Garg, N.M., Agrawal, A. et al. Lung Function Reference Equations for Indian Ethnic Groups Based on a Handheld Forced Oscillation Device for Age 9–19 Years. Indian J Pediatr 90, 61–68 (2023). https://doi.org/10.1007/s12098-022-04176-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04176-2