Abstract
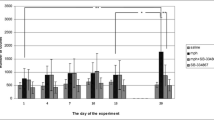
We examined the role of toll-like receptors (TLRs) and proinflammatory cytokine signaling pathways in the prefrontal cortex (PFC) in anxiety-like behaviors after repeated use of morphine. Morphine (10 mg/kg) was used twice daily for 8 days to induce morphine dependence in male Wistar rats. On day 8, opioid dependence was confirmed by measuring naloxone-precipitated withdrawal signs. On days 1 and 8, anxiety-like behaviors were evaluated using a light/dark box test. Expression of TLR1 and 4, proinflammatory cytokines, and some of the downstream signaling molecules was also evaluated in the bilateral PFC at mRNA and protein levels following morphine dependence. The results revealed that morphine caused anxiolytic-like effects on day 1 while induced anxiety following 8 days of repeated injection. On day 8, a significant decrease in TLR1 expression was detected in the PFC in morphine-dependent rats, but TLR4 remained unaffected. Repeated morphine injection significantly increased IL1-β, TNFα, and IL6 expression, but decreased IL1R and TNFR at mRNA and protein levels except for IL6R at the protein level in the PFC. The p38α mitogen-activated protein (MAP) kinase expression significantly increased but the JNK3 expression decreased in the PFC in morphine-dependent rats. Repeated injection of morphine also significantly increased the NF-κB expression in the PFC. Further, significant increases in Let-7c, mir-133b, and mir-365 were detected in the PFC in morphine-dependent rats. We conclude that TLR1 and proinflammatory cytokines signaling pathways in the PFC are associated with the anxiogenic-like effects of morphine following its chronic use in rats via a MAP kinase/NF-κB pathway.







Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Ueda H, Ueda M (2009) Mechanisms underlying morphine analgesic tolerance and dependence. Front Biosci (Landmark Ed) 14:5260–5272. https://doi.org/10.2741/3596
Watkins LR, Hutchinson MR, Rice KC, Maier SF (2009) The “toll” of opioid-induced glial activation: improving the clinical efficacy of opioids by targeting glia. Trends Pharmacol Sci 30:581–591. https://doi.org/10.1016/j.tips.2009.08.002
Glover EM, Davis M (2008) Anxiolytic-like effects of morphine and buprenorphine in the rat model of fear-potentiated startle: tolerance, cross-tolerance, and blockade by naloxone. Psychopharmacol 198:167–180. https://doi.org/10.1007/s00213-008-1112-0
Motaghinejad M, Karimian SM, Motaghinejad O, Shabab B, Asadighaleni M, Fatima S (2015) The effect of various morphine weaning regimens on the sequelae of opioid tolerance involving physical dependency, anxiety and hippocampus cell neurodegeneration in rats. Fundam Clin Pharmacol 29:299–309. https://doi.org/10.1111/fcp.12121
Wilson-Poe AR, Jeong HJ, Vaughan CW (2017) Chronic morphine reduces the readily releasable pool of GABA, a presynaptic mechanism of opioid tolerance. J Physiol 595:6541–6555. https://doi.org/10.1113/jp274157
Koller G, Schwarzer A, Halfter K, Soyka M (2019) Pain management in opioid maintenance treatment. Expert Opin Pharmacother 20:1993–2005. https://doi.org/10.1080/14656566.2019.1652270
Mercadante S, Arcuri E, Santoni A (2019) Opioid-induced tolerance and hyperalgesia. CNS Drugs 33:943–955. https://doi.org/10.1007/s40263-019-00660-0
Kim J, Ham S, Hong H, Moon C (2016) Im HI Brain reward circuits in morphine addiction. Mol Cells 39:645–53. https://doi.org/10.14348/molcells.2016.0137
Koob GF, Volkow ND (2016) Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry 3:760–773. https://doi.org/10.1016/s2215-0366(16)00104-8
Kelley AE, Domesick VB (1982) The distribution of the projection from the hippocampal formation to the nucleus accumbens in the rat: an anterograde- and retrograde-horseradish peroxidase study. Neurosci 7:2321–2335
Sesack SR, Pickel VM (1990) In the rat medial nucleus accumbens, hippocampal and catecholaminergic terminals converge on spiny neurons and are in apposition to each other. Brain Res 527:266–279
Ong WY, Stohler CS, Herr DR (2019) Role of the prefrontal cortex in pain processing. Mol Neurobiol 56:1137–1166. https://doi.org/10.1007/s12035-018-1130-9
Dixon ML, Thiruchselvam R, Todd R, Christoff K (2017) Emotion and the prefrontal cortex: an integrative review. Psychol Bull 143:1033–1081. https://doi.org/10.1037/bul0000096
Adhikari A, Topiwala MA, Gordon JA (2010) Synchronized activity between the ventral hippocampus and the medial prefrontal cortex during anxiety. Neuron 65:257–269. https://doi.org/10.1016/j.neuron.2009.12.002
Lowery-Gionta EG, Crowley NA, Bukalo O, Silverstein S, Holmes A, Kash TL (2018) Chronic stress dysregulates amygdalar output to the prefrontal cortex. Neuropharmacol 139:68–75. https://doi.org/10.1016/j.neuropharm.2018.06.032
Yang Y, Wang JZ (2017) From structure to behavior in basolateral amygdala-hippocampus circuits. Front Neural Circuits 11:86. https://doi.org/10.3389/fncir.2017.00086
Zaki Y, Mau W, Cincotta C, Monasterio A, Odom E, Doucette E et al (2022) Hippocampus and amygdala fear memory engrams re-emerge after contextual fear relapse. Neuropsychopharmacol 47:1992–2001. https://doi.org/10.1038/s41386-022-01407-0
McEwen BS, Morrison JH (2013) The brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron 79:16–29. https://doi.org/10.1016/j.neuron.2013.06.028
Mah L, Szabuniewicz C, Fiocco AJ (2016) Can anxiety damage the brain? Curr Opin Psychiatry 29:56–63. https://doi.org/10.1097/yco.0000000000000223
Koob GF, Volkow ND (2010) Neurocircuitry of addiction. Neuropsychopharmacol 35:217–238. https://doi.org/10.1038/npp.2009.110
Listos J, Łupina M, Talarek S, Mazur A, Orzelska-Górka J, Kotlińska J (2019) The mechanisms involved in morphine addiction: an overview. Int J Mol Sci 20 https://doi.org/10.3390/ijms20174302
Spetea M, Asim MF, Wolber G, Schmidhammer H (2013) The µ opioid receptor and ligands acting at the µ opioid receptor, as therapeutics and potential therapeutics. Curr Pharm Des 19:7415–7434. https://doi.org/10.2174/13816128113199990362
Song P, Zhao ZQ (2001) The involvement of glial cells in the development of morphine tolerance. Neurosci Res 39:281–286. https://doi.org/10.1016/s0168-0102(00)00226-1
Eidson LN, Murphy AZ (2019) Inflammatory mediators of opioid tolerance: Implications for dependency and addiction. Peptides 115:51–58. https://doi.org/10.1016/j.peptides.2019.01.003
Eidson LN, Murphy AZ (2013) Blockade of Toll-like receptor 4 attenuates morphine tolerance and facilitates the pain relieving properties of morphine. J Neurosci 33:15952–15963. https://doi.org/10.1523/jneurosci.1609-13.2013
Wu R, Li JX (2020) Toll-like receptor 4 signaling and drug addiction. Front Pharmacol 11:603445. https://doi.org/10.3389/fphar.2020.603445
Jacobsen JH, Watkins LR, Hutchinson MR (2014) Discovery of a novel site of opioid action at the innate immune pattern-recognition receptor TLR4 and its role in addiction. Int Rev Neurobiol 118:129–163. https://doi.org/10.1016/b978-0-12-801284-0.00006-3
Zhang Y, Li H, Li Y, Sun X, Zhu M, Hanley G et al (2011) Essential role of toll-like receptor 2 in morphine-induced microglia activation in mice. Neurosci Lett 489:43–47. https://doi.org/10.1016/j.neulet.2010.11.063
Liu QF, Li L, Guo YQ, Li X, Mou ZD, Wang X et al (2016) Injection of toll-like receptor 4 siRNA into the ventrolateral periaqueductal gray attenuates withdrawal syndrome in morphine-dependent rats. Arch Ital Biol 154:133–42. https://doi.org/10.12871/00039829201644
Thomas JHL, Lui L, Abell A, Tieu W, Somogyi AA, Bajic JE et al (2022) Toll-like receptors change morphine-induced antinociception, tolerance and dependence: studies using male and female TLR and signalling gene KO mice. Brain Behav Immun 102:71–85. https://doi.org/10.1016/j.bbi.2022.02.001
Shafie A, Moradi F, Izadpanah E, Mokarizadeh A, Moloudi MR, Nikzaban M et al (2015) Neuroprotection of donepezil against morphine-induced apoptosis is mediated through toll-like receptors. Eur J Pharmacol 764:292–297. https://doi.org/10.1016/j.ejphar.2015.07.027
Wang X, Loram LC, Ramos K, de Jesus AJ, Thomas J, Cheng K et al (2012) Morphine activates neuroinflammation in a manner parallel to endotoxin. Proc Natl Acad Sci U S A 109:6325–6330. https://doi.org/10.1073/pnas.1200130109
Liu DQ, Zhou YQ, Gao F (2019) Targeting cytokines for morphine tolerance: a narrative review. Curr Neuropharmacol 17:366–376. https://doi.org/10.2174/1570159x15666171128144441
Barbierato M, Zusso M, Skaper SD, Giusti P (2015) MicroRNAs: emerging role in the endogenous μ opioid system. CNS Neurol Disord Drug Targets 14:239–250. https://doi.org/10.2174/1871527314666150116123932
Huang J, Wang J, Guo Q, Zou W (2019) Emerging roles of microRNAs in morphine tolerance. J Pain Res 12:1139–1147. https://doi.org/10.2147/jpr.s187592
Sartor GC, St Laurent G 3rd, Wahlestedt C (2012) The emerging role of non-coding RNAs in drug addiction. Front Genet 3:106. https://doi.org/10.3389/fgene.2012.00106
Zhang TJ, Qiu Y, Hua Z (2019) The emerging perspective of morphine tolerance: microRNAs. Pain Res Manag 2019:9432965. https://doi.org/10.1155/2019/9432965
Toyama K, Kiyosawa N, Watanabe K, Ishizuka H (2017) Identification of circulating miRNAs differentially regulated by opioid treatment. Int J Mol Sci 18 https://doi.org/10.3390/ijms18091991.
He Y, Wang ZJ (2012) Let-7 microRNAs and opioid tolerance. Front Genet 3:110. https://doi.org/10.3389/fgene.2012.00110
García-Pérez D, López-Bellido R, Hidalgo JM, Rodríguez RE, Laorden ML, Núñez C et al (2015) Morphine regulates argonaute 2 and TH expression and activity but not miR-133b in midbrain dopaminergic neurons. Addict Biol 20:104–119. https://doi.org/10.1111/adb.12083
Rodríguez RE (2012) Morphine and microRNA activity: is there a relation with addiction? Front Genet 3:223. https://doi.org/10.3389/fgene.2012.00223
Wang J, Xu W, Zhong T, Song Z, Zou Y, Ding Z et al (2016) miR-365 targets β-arrestin 2 to reverse morphine tolerance in rats. Sci Rep 6:38285. https://doi.org/10.1038/srep38285
Wu XP, She RX, Yang YP, Xing ZM, Chen HW, Zhang YW (2018) MicroRNA-365 alleviates morphine analgesic tolerance via the inactivation of the ERK/CREB signaling pathway by negatively targeting β-arrestin2. J Biomed Sci 25:10. https://doi.org/10.1186/s12929-018-0405-9
Yu G, Yan H, Gong ZH (2014) Effects of acute and repeated morphine treatment on κ-opioid receptor protein levels in mesocorticolimbic system. J Recept Signal Transduct Res 34:44–47. https://doi.org/10.3109/10799893.2013.856919
Ahmadi S, Zobeiri M, Mohammadi Talvar S, Masoudi K, Khanizad A, Fotouhi S et al (2021) Differential expression of H19, BC1, MIAT1, and MALAT1 long non-coding RNAs within key brain reward regions after repeated morphine treatment. Behav Brain Res 414:113478. https://doi.org/10.1016/j.bbr.2021.113478
Ahmadi S, Khaledi S (2020) Anxiety in rats with bile duct ligation is associated with activation of JNK3 mitogen-activated protein kinase in the hippocampus. Metab Brain Dis 35:579–588. https://doi.org/10.1007/s11011-020-00542-1
Ramos A (2008) Animal models of anxiety: do I need multiple tests? Trends Pharmacol Sci 29:493–498. https://doi.org/10.1016/j.tips.2008.07.005
Bourin M, Hascoet M (2003) The mouse light/dark box test. Eur J Pharmacol 463:55–65
Costall B, Jones BJ, Kelly ME, Naylor RJ, Tomkins DM (1989) Exploration of mice in a black and white test box: validation as a model of anxiety. Pharmacol Biochem Behav 32:777–785. https://doi.org/10.1016/0091-3057(89)90033-6
Ahmadi S, Poureidi M, Rostamzadeh J (2015) Hepatic encephalopathy induces site-specific changes in gene expression of GluN1 subunit of NMDA receptor in rat brain. Metab Brain Dis 30:1035–1041. https://doi.org/10.1007/s11011-015-9669-x
Chiu K, Lau WM, Lau HT, So KF, Chang RC (2007) Micro-dissection of rat brain for RNA or protein extraction from specific brain region. J Vis Exp 269 https://doi.org/10.3791/269
Ahmadi S, Karami Z, Mohammadian A, Khosrobakhsh F, Rostamzadeh J (2015) Cholestasis induced antinociception and decreased gene expression of MOR1 in rat brain. Neurosci 284:78–86. https://doi.org/10.1016/j.neuroscience.2014.08.063
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25:402–408. https://doi.org/10.1006/meth.2001.1262
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254. https://doi.org/10.1006/abio.1976.9999
Liu JG, Anand KJ (2001) Protein kinases modulate the cellular adaptations associated with opioid tolerance and dependence. Brain Res Brain Res Rev 38:1–19. https://doi.org/10.1016/s0165-0173(01)00057-1
Bali P, Kenny PJ (2019) Transcriptional mechanisms of drug addiction. Dialogues Clin Neurosci 21:379–87. https://doi.org/10.31887/DCNS.2019.21.4/pkenny
Robison AJ, Nestler EJ (2011) Transcriptional and epigenetic mechanisms of addiction. Nat Rev Neurosci 12:623–637. https://doi.org/10.1038/nrn3111
Roeska K, Doods H, Arndt K, Treede RD, Ceci A (2008) Anxiety-like behaviour in rats with mononeuropathy is reduced by the analgesic drugs morphine and gabapentin. Pain 139:349–357. https://doi.org/10.1016/j.pain.2008.05.003
Shin IC, Kim HC, Swanson J, Hong JT, Oh KW (2003) Anxiolytic effects of acute morphine can be modulated by nitric oxide systems. Pharmacol 68:183–189. https://doi.org/10.1159/000070457
Miladi-Gorji H, Rashidy-Pour A, Fathollahi Y (2012) Anxiety profile in morphine-dependent and withdrawn rats: effect of voluntary exercise. Physiol Behav 105:195–202. https://doi.org/10.1016/j.physbeh.2011.08.010
Lee B, Sur B, Yeom M, Shim I, Lee H, Hahm DH (2012) Effect of berberine on depression- and anxiety-like behaviors and activation of the noradrenergic system induced by development of morphine dependence in rats. Korean J Physiol Pharmacol 16:379–386. https://doi.org/10.4196/kjpp.2012.16.6.379
Motaghinejad M, Fatima S, Banifazl S, Bangash MY, Karimian M (2016) Study of the effects of controlled morphine administration for treatment of anxiety, depression and cognition impairment in morphine-addicted rats. Adv Biomed Res 5:178. https://doi.org/10.4103/2277-9175.188491
Jarvik LF, Simpson JH, Guthrie D, Liston EH (1981) Morphine, experimental pain, and psychological reactions. Psychopharmacol 75:124–131. https://doi.org/10.1007/bf00432173
Niu H, Zhang G, Li H, Zhang Q, Li T, Ding S et al (2017) Multi-system state shifts and cognitive deficits induced by chronic morphine during abstinence. Neurosci Lett 640:144–151. https://doi.org/10.1016/j.neulet.2016.10.057
Wang Y, Zhang H, Cui J, Zhang J, Yin F, Guo H et al (2019) Opiate-associated contextual memory formation and retrieval are differentially modulated by dopamine D1 and D2 signaling in hippocampal-prefrontal connectivity. Neuropsychopharmacol 44:334–343. https://doi.org/10.1038/s41386-018-0068-y
Quintero GC (2013) Role of nucleus accumbens glutamatergic plasticity in drug addiction. Neuropsychiatr Dis Treat 9:1499–1512. https://doi.org/10.2147/ndt.s45963
Hutchinson MR, Shavit Y, Grace PM, Rice KC, Maier SF, Watkins LR (2011) Exploring the neuroimmunopharmacology of opioids: an integrative review of mechanisms of central immune signaling and their implications for opioid analgesia. Pharmacol Rev 63:772–810. https://doi.org/10.1124/pr.110.004135
Gay NJ, Gangloff M, Weber AN (2006) Toll-like receptors as molecular switches. Nat Rev Immunol 6:693–698. https://doi.org/10.1038/nri1916
Triantafilou M, Gamper FG, Haston RM, Mouratis MA, Morath S, Hartung T et al (2006) Membrane sorting of toll-like receptor (TLR)-2/6 and TLR2/1 heterodimers at the cell surface determines heterotypic associations with CD36 and intracellular targeting. J Biol Chem 281:31002–31011. https://doi.org/10.1074/jbc.M602794200
Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N et al (2008) Opioid complications and side effects. Pain Physician 11:S105–S120
Allouche S, Noble F, Marie N (2014) Opioid receptor desensitization: mechanisms and its link to tolerance. Front Pharmacol 5:280. https://doi.org/10.3389/fphar.2014.00280
Corder G, Castro DC, Bruchas MR, Scherrer G (2018) Endogenous and exogenous opioids in pain. Annu Rev Neurosci 41:453–473. https://doi.org/10.1146/annurev-neuro-080317-061522
Law PY, Wong YH, Loh HH (2000) Molecular mechanisms and regulation of opioid receptor signaling. Annu Rev Pharmacol Toxicol 40:389–430. https://doi.org/10.1146/annurev.pharmtox.40.1.389
Raman M, Chen W, Cobb MH (2007) Differential regulation and properties of MAPKs. Oncogene 26:3100–3112. https://doi.org/10.1038/sj.onc.1210392
Yuill MB, Zee ML, Marcus D, Morgan DJ (2016) Tolerance to the antinociceptive and hypothermic effects of morphine is mediated by multiple isoforms of c-Jun N-terminal kinase. NeuroReport 27:392–396. https://doi.org/10.1097/wnr.0000000000000551
Marcus DJ, Zee M, Hughes A, Yuill MB, Hohmann AG, Mackie K et al (2015) Tolerance to the antinociceptive effects of chronic morphine requires c-Jun N-terminal kinase. Mol Pain 11:34. https://doi.org/10.1186/s12990-015-0031-4
Chen Y, Sommer C (2009) The role of mitogen-activated protein kinase (MAPK) in morphine tolerance and dependence. Mol Neurobiol 40:101–107. https://doi.org/10.1007/s12035-009-8074-z
Cui Y, Chen Y, Zhi JL, Guo RX, Feng JQ, Chen PX (2006) Activation of p38 mitogen-activated protein kinase in spinal microglia mediates morphine antinociceptive tolerance. Brain Res 1069:235–243. https://doi.org/10.1016/j.brainres.2005.11.066
Cui Y, Liao XX, Liu W, Guo RX, Wu ZZ, Zhao CM et al (2008) A novel role of minocycline: attenuating morphine antinociceptive tolerance by inhibition of p38 MAPK in the activated spinal microglia. Brain Behav Immun 22:114–123. https://doi.org/10.1016/j.bbi.2007.07.014
Hong SI, Nguyen TL, Ma SX, Kim HC, Lee SY, Jang CG (2017) TRPV1 modulates morphine-induced conditioned place preference via p38 MAPK in the nucleus accumbens. Behav Brain Res 334:26–33. https://doi.org/10.1016/j.bbr.2017.07.017
Zhang X, Cui Y, Jing J, Cui Y, Xin W, Liu X (2011) Involvement of p38/NF-κB signaling pathway in the nucleus accumbens in the rewarding effects of morphine in rats. Behav Brain Res 218:184–189. https://doi.org/10.1016/j.bbr.2010.11.049
He Y, Yang C, Kirkmire CM, Wang ZJ (2010) Regulation of opioid tolerance by let-7 family microRNA targeting the mu opioid receptor. J Neurosci 30:10251–10258. https://doi.org/10.1523/jneurosci.2419-10.2010
Acknowledgements
This research was funded by the Cognitive Sciences and Technologies Council of Iran (Contract No. D/100/11988).
Funding
This study was funded by the Cognitive Sciences and Technologies Council of Iran (Contract No. D/100/11988).
Author information
Authors and Affiliations
Contributions
Shamseddin Ahmadi: conceptualization and design of the work, writing—original draft preparation, writing—reviewing and editing, supervision, project administration, and funding acquisition. Mohammad Zobeiri, Shiva Mohammadi Talvar, and Kayvan Masoudi: acquisition, analysis, interpretation of data, and writing—original draft preparation. All authors approved the final version for publication.
Corresponding author
Ethics declarations
Ethics Approval
All procedures were done according to the Guide for the Care and Use of Laboratory Animals (2011) prepared by the National Academy of Sciences’ Institute for Laboratory Animal Research. The Research Ethics Committee (REC) at the University of Kurdistan approved the study protocol (IR.UOK.REC.1398.021).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahmadi, S., Mohammadi Talvar, S., Masoudi, K. et al. Repeated Use of Morphine Induces Anxiety by Affecting a Proinflammatory Cytokine Signaling Pathway in the Prefrontal Cortex in Rats. Mol Neurobiol 60, 1425–1439 (2023). https://doi.org/10.1007/s12035-022-03144-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-03144-3