Abstract
Invasive mucinous adenocarcinoma (IMA) is a rare variant of adenocarcinoma with unique clinical, radiological, and pathological features, among which KRAS mutation is the most common. However, the differences in the efficacy of immunotherapy between KRAS-positive IMA and invasive non-mucinous adenocarcinoma (INMA) patients remain unclear. Patients with KRAS mutated adenocarcinomas receiving immunotherapy between June 2016 and December 2022 were enrolled. Based on mucin-producing status, the patients were placed into two subgroups: the IMA group and INMA group. Patients with IMA were further classified into two subtypes according to the presence of mucin patterns: pure IMA (≥ 90%) and mixed mucinous/nonmucinous adenocarcinoma (≥ 10% of each histological component). Kaplan–Meier Curves and log-rank tests were used to analyze survival. Cox regression analysis of PFS were used to analyze the independent factors associated with efficacy. Sixty-five advanced adenocarcinoma patients with KRAS mutations received immunotherapy, including 24 patients with IMA and 41 with INMA. The median progression-free survival (PFS) was 7.7 months, whereas the median overall survival (OS) was 24.0 months. Significant difference in PFS could be observed in IMA and INMA (3.5 months vs. 8.9 months; P = 0.047). Patients with pure IMA tended toward prolonger survival in contrast to mixed mucinous/nonmucinous adenocarcinoma in PFS (8.4 months vs. 2.3 months; P = 0.349). The multivariable analysis demonstrated that IMA was an independent risk factor for PFS. In KRAS mutated patients, IMA was associated with poorer PFS after immunotherapy compared with INMA.






Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Chang JC, Offin M, Falcon C, Brown D, Houck-Loomis BR, Meng F, Rudneva VA, Won HH, Amir S, Montecalvo J, Desmeules P, Kadota K, Adusumilli PS, Rusch VW, Teed S, Sabari JK, Benayed R, Nafa K, Borsu L, Li BT, Schram AM, Arcila ME, Travis WD, Ladanyi M, Drilon A, Rekhtman N. Comprehensive molecular and clinicopathologic analysis of 200 pulmonary invasive mucinous adenocarcinomas identifies distinct characteristics of molecular subtypes. Clin Cancer Res. 2021;27(14):4066–76. https://doi.org/10.1158/1078-0432.CCR-21-0423.
Gow CH, Hsieh MS, Liu YN, Lee YH, Shih JY. Clinicopathological features and survival outcomes of primary pulmonary invasive mucinous adenocarcinoma. Cancers. 2021;13(16):4103. https://doi.org/10.3390/cancers13164103.
Cai D, Li H, Wang R, Li Y, Pan Y, Hu H, Zhang Y, Gong R, Pan B, Sun Y, Chen H. Comparison of clinical features, molecular alterations, and prognosis in morphological subgroups of lung invasive mucinous adenocarcinoma. Onco Targets Ther. 2014;7:2127–32. https://doi.org/10.2147/OTT.S70984.
Yang SR, Chang JC, Leduc C, Tan KS, Dogan S, Benayed R, Borsu L, Offin M, Drilon A, Travis WD, Arcila ME, Ladanyi M, Rekhtman N. Invasive mucinous adenocarcinomas with spatially separate lung lesions: analysis of clonal relationship by comparative molecular profiling. J Thorac Oncol. 2021;16(7):1188–99. https://doi.org/10.1016/j.jtho.2021.03.023.
Luo J, Wang R, Han B, Zhang J, Zhao H, Fang W, Luo Q, Yang J, Yang Y, Zhu L, Chen T, Cheng X, Huang Q, Wang Y, Zheng J, Chen H. Analysis of the clinicopathologic characteristics and prognostic of stage I invasive mucinous adenocarcinoma. J Cancer Res Clin Oncol. 2016;142(8):1837–45. https://doi.org/10.1007/s00432-016-2201-9.
Sun F, Wang P, Zheng Y, Jia W, Liu F, Xiao W, Bao J, Wang S, Lu K. Diagnosis, clinicopathological characteristics and prognosis of pulmonary mucinous adenocarcinoma. Oncol Lett. 2018;15:489–94. https://doi.org/10.3892/ol.2017.7312.
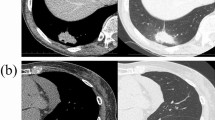
Zhang S, Yu X, Huang Y, Nie P, Deng Y, Mao N, Li S, Zhu B, Wang L, Wang B, Wang X. Pneumonic-type invasive mucinous adenocarcinoma and infectious pneumonia: clinical and CT imaging analysis from multiple centers. BMC Pulm Med. 2022;22(1):460. https://doi.org/10.1186/s12890-022-02268-5.
Wang T, Yang Y, Liu X, Deng J, Wu J, Hou L, Wu C, She Y, Sun X, Xie D, Chen C. Primary invasive mucinous adenocarcinoma of the lung: prognostic value of CT imaging features combined with clinical factors. Korean J Radiol. 2021;22(4):652. https://doi.org/10.3348/kjr.2020.0454.
Zhang X, Qiao W, Kang Z, Pan C, Chen Y, Li K, Shen W, Zhang L. CT features of stage IA invasive mucinous adenocarcinoma of the lung and establishment of a prediction model. IJGM. 2022;15:5455–63. https://doi.org/10.2147/IJGM.S368344.
Yamakawa H, Takayanagi N, Ishiguro T, Kagiyama N, Shimizu Y, Sugita Y. A favorable response to cisplatin, pemetrexed and bevacizumab in two cases of invasive mucinous adenocarcinoma formerly known as pneumonic-type mucinous bronchioloalveolar carcinoma. Intern Med. 2013;52(24):2781–4. https://doi.org/10.2169/internalmedicine.52.0766.
Zhou D, Gulinuer W, Zhu N. Chemotherapy in combination with pembrolizumab and antiangiogenesis in young patients with advanced primary pulmonary mucinous adenocarcinoma: two case reports. Sci Prog. 2021;104(4):003685042110619. https://doi.org/10.1177/00368504211061971.
Cha YJ, Kim HR, Lee HJ, Cho BC, Shim HS. Clinical course of stage IV invasive mucinous adenocarcinoma of the lung. Lung Cancer. 2016;102:82–8. https://doi.org/10.1016/j.lungcan.2016.11.004.
Chen Z, Li M, Ma K, Shang G, Liang J, Yin J, Luo J, Zhan C, Shi Y, Wang Q. Analysis of the clinicopathological characteristics, genetic phenotypes, and prognostic of pure mucinous adenocarcinoma. Cancer Med. 2020;9(2):517–29. https://doi.org/10.1002/cam4.2726.
Moon SW, Choi SY, Moon MH. Effect of invasive mucinous adenocarcinoma on lung cancer-specific survival after surgical resection: a population-based study. J Thorac Dis. 2018;10(6):3595–608. https://doi.org/10.21037/jtd.2018.06.09.
Gu Y, Zhu H, Deng J, Zhang J, Chen T, Lai S. Comparison of treatment strategies for resectable locally advanced primary mucinous adenocarcinoma of the lung. Cancer Med. 2023. https://doi.org/10.1002/cam4.5684.
Casali C, Rossi G, Marchioni A, Sartori G, Maselli F, Longo L, Tallarico E, Morandi U. A single institution-based retrospective study of surgically treated bronchioloalveolar adenocarcinoma of the lung: clinicopathologic analysis, molecular features, and possible pitfalls in routine practice. J Thorac Oncol. 2010;5(6):830–6. https://doi.org/10.1097/jto.0b013e3181d60ff5.
Gianoncelli L, Spitaleri G, Passaro A, Fumagalli C, Del Signore E, Stati V, Catania CM, Guerini-Rocco E, Barberis M, Marinis DEF. Efficacy of anti-PD1/PD-L1 therapy (IO) in KRAS mutant non-small cell lung cancer patients: a retrospective analysis. Anticancer Res. 2020;40(1):427–33. https://doi.org/10.21873/anticanres.13970.
Veccia A, Dipasquale M, Kinspergher S, Monteverdi S, Girlando S, Barbareschi M, Caffo O. Impact of KRAS mutations on clinical outcomes of patients with advanced non-squamous non-small cell lung cancer receiving anti-PD-1/PD-L1 therapy. Targ Oncol. 2023;18(1):129–38. https://doi.org/10.1007/s11523-022-00934-6.
Knetki-Wróblewska M, Tabor S, Płużański A, Lewandowska Z, Tysarowski A, Pawlik H, Kowalski DM, Krzakowski M. Efficacy of immunotherapy in second-line treatment of KRAS-mutated patients with non-small-cell lung cancer—data from daily practice. Curr Oncol. 2022;30(1):462–75. https://doi.org/10.3390/curroncol30010037.
Peng L, Guo J, Kong L, Huang Y, Tang N, Zhang J, Wang M, He X, Li Z, Peng Y, Wang Z, Han X. Efficacy of immunotherapy in KRAS-mutant advanced NSCLC: a real-world study in a Chinese population. Front Oncol. 2023;12:1070761. https://doi.org/10.3389/fonc.2022.1070761.
Yoon HJ, Kang J, Lee HY, Lee MA, Hwang NY, Kim HK, Kim J. Recurrence dynamics after curative surgery in patients with invasive mucinous adenocarcinoma of the lung. Insights Imaging. 2022;13(1):64. https://doi.org/10.1186/s13244-022-01208-5.
Boland JM, Maleszewski JJ, Wampfler JA, Voss JS, Kipp BR, Yang P, Yi ES. Pulmonary invasive mucinous adenocarcinoma and mixed invasive mucinous/nonmucinous adenocarcinoma—a clinicopathological and molecular genetic study with survival analysis. Hum Pathol. 2018;71:8–19. https://doi.org/10.1016/j.humpath.2017.08.002.
Acknowledgements
The authors would like to appreciate all patients for their cooperation and participation. In addition, we are thankful to all research staff and co-investigators involved in this study.
Funding
The study was supported by the Medical Scientific Research Foundation of Zhejiang Province (No.2022KY653), and sponsored by Zhejiang provincial program for the Cultivation of High-Level Innovative Health Talents (to Zhengbo Song).
Author information
Authors and Affiliations
Contributions
ZS designed and supervised the research. MX, YH, HZ conducted the follow-up, data collection, and correlative analysis. HZ and ZS provided support in data analysis and use of software. MX, YH provided data analysis. All authors were involved in manuscript preparation and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethics approval and consent to participate
Approval of the study protocol was obtained from Zhejiang Cancer Hospital Institutional Review Board Committee (approval number: IRB-2022–187). Individual consent for this retrospective analysis was waived.
Consent for publication
Not applicable.
Consent to participate and publish
Individual consent for analysis was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, M., Hao, Y., Zhou, H. et al. Comparison of the immunotherapy efficacy between invasive mucinous and non-mucinous adenocarcinoma in advanced lung cancer patients with KRAS mutation: a retrospective study. Med Oncol 40, 198 (2023). https://doi.org/10.1007/s12032-023-02059-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-023-02059-w