Abstract
Background
Traumatic brain injury is a common and devastating injury that is the leading cause of neurological disability and death worldwide. Patients with cerebral lobe contusion received conservative treatment because of their mild manifestations, but delayed intracranial hematoma may increase and even become life-threatening. We explored the noninvasive method to predict the prognosis of progression and Glasgow Outcome Scale (GOS) by using a quantitative radiomics approach and statistical analysis.
Methods
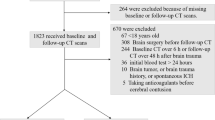
Eighty-eight patients who were pathologically diagnosed were retrospectively studied. The radiomics method developed in this work included image segmentation, feature extraction, and feature selection. The nomograms were established based on statistical analysis and a radiomics method. We conducted a comparative study of hematoma progression and GOS between the clinical factor alone and fusion radiomics features.
Results
Nineteen clinical factors, 513 radiomics features, and 116 locational features were considered. Among clinical factors, international normalized ratio, prothrombin time, and fibrinogen were enrolled for hematoma progression. As for GOS, treatment strategy, age, Glasgow Coma Scale score, and blood platelet were associated factors. Eight features for GOS and five features for hematoma progression were filtered by using sparse representation and locality preserving projection-combined method. Four nomograms were constructed. After fusion radiomics features, area under the curve of hematoma progression prediction increased from 0.832 to 0.899, whereas GOS prediction went from 0.794 to 0.844.
Conclusions
A radiomic-based model that merges radiomics and clinical features is a noninvasive approach to predict hematoma progression and clinical outcomes of cerebral contusions in traumatic brain injury.



Similar content being viewed by others
References
Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728–41.
Gao L, Wu X, Hu J, Jin Y, Han X, Wu X, et al. Intensive management and prognosis of 127 cases with traumatic bilateral frontal contusions. World Neurosurg. 2013;80(6):879–88.
Carnevale JA, Segar DJ, Powers AY, Shah M, Doberstein C, Drapcho B, et al. Blossoming contusions: identifying factors contributing to the expansion of traumatic intracerebral hemorrhage. J Neurosurg. 2018;129(5):1305–16.
Allison RZ, Nakagawa K, Hayashi M, Donovan DJ, Koenig MA. Derivation of a predictive score for hemorrhagic progression of cerebral contusions in moderate and severe traumatic brain injury. Neurocrit Care. 2017;26(1):80–6.
Van de Zande N, Manivannan S, Sharouf F, Shastin D, Abdulla M, Chumas PD, et al. Demographics, presentation, and clinical outcomes after traumatic bifrontal contusions: a systematic review. Neurosurg Rev. 2019;3:195.
Coroller TP, Grossmann P, Hou Y, Rios Velazquez E, Leijenaar RT, Hermann G, et al. CT-based radiomic signature predicts distant metastasis in lung adenocarcinoma. Radiother Oncol. 2015;114(3):345–50.
Wibmer A, Hricak H, Gondo T, Matsumoto K, Veeraraghavan H, Fehr D, et al. Haralick texture analysis of prostate MRI: utility for differentiating non-cancerous prostate from prostate cancer and differentiating prostate cancers with different Gleason scores. Eur Radiol. 2015;25(10):2840–50.
Wu G, Chen Y, Wang Y, Yu J, Chen Z. Sparse representation-based radiomics for the diagnosis of brain tumors. IEEE Trans Med Imaging. 2017;99:1.
Lv J, Iraji A, Chen H, Ge F, Liu T. Group-wise sparse representation of brain states reveal network abnormalities in mild traumatic brain injury. In: IEEE International Symposium on Biomedical Imaging 2016.
Wright J, Yang AY, Ganesh A, Sastry SS, Ma Y. Robust face recognition via sparse representation. IEEE Trans Pattern Anal Mach Intell. 2009;31(2):210–27.
Elad M, Aharon M. Image denoising via sparse and redundant representations over learned dictionaries. IEEE Trans Image Process. 2006;15(12):3736–45.
Brain TF, American Association of Neurological S, Congress of Neurological S, Joint Section on N, Critical Care AC, Carney NA, et al. Guidelines for the management of severe traumatic brain injury. Introduction. J Neurotrauma 2007;24 Suppl 1:S1–2.
Chen LC, Papandreou G, Kokkinos I, Murphy K, Yuille AL. Semantic image segmentation with deep convolutional nets and fully connected CRFs. Computer Science. 2014;4:357–61.
Ronneberger O, Fischer P, Brox T. U-Net: Convolutional Networks for Biomedical Image Segmentation. 2015.
Wu G, Chunhong J, Jinhua Y, Yuanyuan W, Liang C, Zhifeng S, et al. Automatic segmentation of Glioma from 3D MR images by using location free asymmetry detection. SM J Biomed Eng. 2017;3(1):1012–20.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006.
Xiaofeng Z, Heung-Il S, Seong-Whan L, et al. Subspace regularized sparse multitask learning for multiclass neurodegenerative disease identification. IEEE Trans Bio Med Eng. 2016;26:9.
Dong W, Lei Z, Shi G. Centralized sparse representation for image restoration. In: IEEE International Conference on Computer Vision 2012.
Rückstieß T, Osendorfer C, Smagt PVD. Sequential Feature Selection for Classification. 2011.
Shimoda K, Maeda T, Tado M, Yoshino A, Katayama Y, Bullock MR. Outcome and surgical management for geriatric traumatic brain injury: analysis of 888 cases registered in the Japan Neurotrauma Data Bank. World Neurosurg. 2014;82(6):1300–6.
Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, D’Urso P, et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364(16):1493–502.
Jiang JY, Xu W, Li WP, Xu WH, Zhang J, Bao YH, et al. Efficacy of standard trauma craniectomy for refractory intracranial hypertension with severe traumatic brain injury: a multicenter, prospective, randomized controlled study. J Neurotrauma. 2005;22(6):623–8.
Cepeda S, Gomez PA, Castano-Leon AM, Munarriz PM, Paredes I, Lagares A. Contrecoup traumatic intracerebral hemorrhage: a geometric study of the impact site and association with hemorrhagic progression. J Neurotrauma. 2016;33(11):1034–46.
Wong H, Lovett N, Curry N, Shah K, Stanworth SJ. Antithrombotics in trauma: management strategies in the older patients. J Blood Med. 2017;8:165–74.
E S, H K, Y F, H Y, M S. Predictors of deterioration indicating a requirement for surgery in mild to moderate traumatic brain injury. Clini Neurol Neurosurg 2014;127:97–100.
Zhang J, Zhang F, Dong JF. Coagulopathy induced by traumatic brain injury: systemic manifestation of a localized injury. Blood. 2018;131(18):2001–6.
Kawano-Castillo J, Ward E, Elliott A, Wetzel J, Hassler A, McDonald M, et al. Thrombelastography detects possible coagulation disturbance in patients with intracerebral hemorrhage with hematoma enlargement. Stroke. 2014;45(3):683–8.
Einarsen CE, van der Naalt J, Jacobs B, Follestad T, Moen KG, Vik A, et al. Moderate traumatic brain injury: clinical characteristics and a prognostic model of 12-month outcome. World Neurosurg. 2018;114:e1199–210.
Farzaneh N, Williamson CA, Gryak J, Najarian K. A hierarchical expert-guided machine learning framework for clinical decision support systems: an application to traumatic brain injury prognostication. NPJ Digit Med. 2021;4(1):78.
Martin RM, Wright MJ, Lutkenhoff ES, Ellingson BM, Van Horn JD, Tubi M, et al. Traumatic hemorrhagic brain injury: impact of location and resorption on cognitive outcome. J Neurosurg. 2017;126(3):796–804.
Tang Q, Lian Y, Yu J, Wang Y, Shi Z, Chen L. Anatomic mapping of molecular subtypes in diffuse glioma. BMC Neurol. 2017;17(1):183.
Yuh EL, Cooper SR, Ferguson AR, Manley GT. Quantitative CT improves outcome prediction in acute traumatic brain injury. J Neurotrauma. 2012;29(5):735–46.
de la Rosa E, Sima DM, Vyvere TV, Kirschke JS, Menze B. A Radiomics Approach to Traumatic Brain Injury Prediction in CT Scans. 2018.
Hale AT, Stonko DP, Brown A, Lim J, Voce DJ, Gannon SR, et al. Machine-learning analysis outperforms conventional statistical models and CT classification systems in predicting 6-month outcomes in pediatric patients sustaining traumatic brain injury. Neurosurg Focus. 2018;45(5):E2.
Dong D, Tang L, Li ZY, Fang MJ, Gao JB, Shan XH, et al. Development and validation of an individualized nomogram to identify occult peritoneal metastasis in patients with advanced gastric cancer. Ann Oncol. 2019;30(3):431–8.
Funding
This study was supported by the Shanghai Municipal Science and Technology Major Project (No. 2018SHZDZX01) and ZJLab, National Natural Science Foundation of China (91959127), The Natural Science Foundation and Major Basic Research Program of Shanghai (16JC1420100), and Shanghai Muncipal Health Commission Project (2018ZHYL0107).
Author information
Authors and Affiliations
Author notes
Liqiong Zhang and Qiyuan Zhuang are contributed equally to this paper.
Contributions
L.Z. and Q.Z. contributed equally to this work. J.Y. and Q.Y: Study concept and design. L.Z. and Q.Z: Drafting of the manuscript. Q.Z: Statistical analysis. L.Z. and Q.Z: Interpretation of data. J.H., J.Y. and Q.Y: Critical revision of the manuscript for important intellectual content. G.W., J.Y., and Z.S: Administrative, technical, or material support.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval/informed consent.
We confirm adherence to ethical guidelines and indicate ethical approvals (institutional review board). Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, L., Zhuang, Q., Wu, G. et al. Combined Radiomics Model for Prediction of Hematoma Progression and Clinical Outcome of Cerebral Contusions in Traumatic Brain Injury. Neurocrit Care 36, 441–451 (2022). https://doi.org/10.1007/s12028-021-01320-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01320-2