Abstract
Purpose
Non-functioning pituitary adenomas (NFPAs) are often associated with hyperprolactinemia, which is known as the “stalk effect”. However, the relationships between hyperprolactinemia and the radiographic characteristics of the tumor that affects the pituitary stalk have not been well characterized. We aimed to identify the differences in the clinical and radiographic characteristics of patients with NFPA, with and without hyperprolactinemia.
Methods
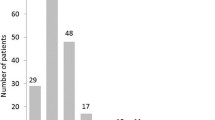
We enrolled 107 patients with NFPA and allocated them to hyperprolactinemia and non-hyperprolactinemia groups using two different cut-off values: (1) the upper limit of the normal reference range, adjusted for sex and menopausal status, and (2) the upper quartile across the cohort, and compared their clinical and radiographic characteristics. These analyses were conducted to clarify the relationship between the “stalk effect” and the postoperative change in antidiuretic hormone secretion.
Results
The specific radiographic characteristics of the patients included the presence of a cystic or hemorrhagic tumor and the presence of pituitary stalk deviation, which were more frequent in the patients with hyperprolactinemia. Interestingly, the incidence of postoperative transient diabetes insipidus was statistically significantly higher in the hyperprolactinemia group (≥40 ng/mL) and in the group with radiologic evidence of stalk deviation, which were shown to be independent risk factors on multivariate analysis.
Conclusion
The presence of a “stalk effect” was associated with a higher risk of postoperative transient diabetes insipidus, reflecting perioperative pituitary stalk dysfunction following NFPA surgery, especially in patients with serum prolactin concentrations ≥40 ng/mL and radiologic evidence of stalk deviation.





Similar content being viewed by others
References
M.B.S. Lopes, Pathology of prolactinomas: any predictive value? Pituitary 23, 3–8 (2020). https://doi.org/10.1007/s11102-019-00997-1
G. Ntali, J.A. Wass, Epidemiology, clinical presentation and diagnosis of non-functioning pituitary adenomas. Pituitary 21, 111–118 (2018). https://doi.org/10.1007/s11102-018-0869-3
N. Ben-Jonathan, R. Hnasko, Dopamine as a prolactin (PRL) inhibitor. Endocr. Rev. 22, 724–763 (2001). https://doi.org/10.1210/edrv.22.6.0451
J. Chahal, J. Schlechte, Hyperprolactinemia. Pituitary 11, 141–146 (2008). https://doi.org/10.1007/s11102-008-0107-5
I. Samperi, K. Lithgow, N. Karavitaki, Hyperprolactinemia. J. Clin. Med. 8, 2203 (2019). https://doi.org/10.3390/jcm8122203
L. Vilar, C.F. Vilar, R. Lyra, M.D.C. Freitas, Pitfalls in the diagnostic evaluation of hyperprolactinemia. Neuroendocrinology 109, 7–19 (2019). https://doi.org/10.1159/000499694
S. Melmed, F.F. Casanueva, A.R. Hoffman, D.L. Kleinberg, V.M. Montori, J.A. Schlechte, J.A. Wass, Endocrine Society: Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 273–288 (2011). https://doi.org/10.1210/jc.2010-1692
S. Petersenn, M. Fleseriu, F.F. Casanueva, A. Giustina, N. Biermasz, B.M.K. Biller, M. Bronstein, P. Chanson, H. Fukuoka, M. Gadelha, Y. Greenman, M. Gurnell, K.K.Y. Ho, J. Honegger, A.G. Ioachimescu, U.B. Kaiser, N. Karavitaki, L. Katznelson, M. Lodish, D. Maiter, H.J. Marcus, A. McCormack, M. Molitch, C.A. Muir, S. Neggers, A.M. Pereira, R. Pivonello, K. Post, G. Raverot, R. Salvatori, S.L. Samson, I. Shimon, J. Spencer-Segal, G. Vila, J. Wass, S. Melmed, Diagnosis and management of prolactin-secreting pituitary adenomas: a Pituitary Society international Consensus Statement. Nat. Rev. Endocrinol. 19, 722–740 (2023). https://doi.org/10.1038/s41574-023-00886-5
M. Fleseriu, M.E. Bodach, L.M. Tumialan, V. Bonert, N.M. Oyesiku, C.G. Patil, Z. Litvack, M.K. Aghi, G. Zada, Congress of neurosurgical surgeons systematic review and evidence-based guideline for pretreatment endocrine evaluation of patients with nonfunctioning pituitary adenomas. Neurosurgery 79, E527–E529 (2016). https://doi.org/10.1227/NEU.0000000000001387
F. Zhang, Y. Huang, C. Ding, G. Huang, S. Wang, The prevalence of hyperprolactinemia in non-functioning pituitary macroadenomas. Int. J. Clin. Exp. Med 8, 18990–18997 (2015)
F. de Vries, D.J. Lobatto, M.J.T. Verstegen, W.R. van Furth, A.M. Pereira, N.R. Biermasz, Postoperative diabetes insipidus: how to define and grade this complication? Pituitary 24, 284–291 (2021). https://doi.org/10.1007/s11102-020-01083-7
E.K. Brooks, W.J. Inder, Disorders of salt and water balance after pituitary surgery. J. Clin. Endocrinol. Metab. 108, 198–208 (2022). https://doi.org/10.1210/clinem/dgac622
S.S.M. Anwar, K. Hilal, A. Khan, A. Ahmad, Magnetic resonance imaging grading of pituitary macroadenoma – SIPAP classification revised. Eur. J. Radiol. Open. 10, 100486 (2023). https://doi.org/10.1016/j.ejro.2023.100486
B. Cabuk, I. Anik, S. Kokturk, S. Ceylan, S. Ceylan, Anatomic and histologic features of diaphragma sellae that effects the suprasellar extension. J. Clin. Neurosci. 71, 234–244 (2020). https://doi.org/10.1016/j.jcon.2019.11.014
S. Gulsen, A.H. Dinc, M. Unal, N. Cantürk, N. Altinors, Characterization of the anatomic location of the pituitary stalk and its relationship to the dorsum sellae, tuberculum sellae and chiasmatic cistern. J. Korean Neurosurg. Soc. 47, 169–173 (2010). https://doi.org/10.3340/jkns.2010.47.3.169
E. Knosp, E. Steiner, K. Kitz, C. Matula, Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33, 610–617 (1993). https://doi.org/10.1227/00006123-199310000-00008. discussion 617-618
L. Lyu, S. Yin, Y. Hu, C. Chen, Y. Jiang, Y. Yu, W. Ma, Z. Wang, S. Jiang, P. Zhou, Hyperprolactinemia in clinical non-functional pituitary macroadenomas: A STROBE-compliant study. Medicine 99, e22673 (2020). https://doi.org/10.1097/M.D.0000000000022673
S.S. Park, J.H. Kim, Y.H. Kim, J.H. Lee, Y.S. Dho, C.S. Shin, Clinical and radiographic characteristics related to hyperprolactinemia in nonfunctioning pituitary adenomas. World Neurosurg. 119, e1035–e1040 (2018). https://doi.org/10.1016/j.wneu.2018.08.068
M. Bergsneider, L. Mirsadraei, W.H. Yong, N. Salamon, M. Linetsky, M.B. Wang, D.L. McArthur, A.P. Heaney, The pituitary stalk effect: is it a passing phenomenon? J. Neurooncol. 117, 477–484 (2014). https://doi.org/10.1007/s11060-014-1386-5
A. Kruse, J. Astrup, C. Gyldensted, G.E. Cold, Hyperprolactinaemia in patients with pituitary adenomas. The pituitary stalk compression syndrome. Br. J. Neurosurg. 9, 453–457 (1995). https://doi.org/10.1080/02688699550041089
M.V. Smith, E.R. Laws Jr, Magnetic resonance imaging measurements of pituitary stalk compression and deviation in patients with nonprolactin-secreting intrasellar and parasellar tumors: lack of correlation with serum prolactin levels. Neurosurgery 34, 834–839 (1994). https://doi.org/10.1227/00006123-199405000-00007. discussion 839
B.M. Arafah, D. Prunty, J. Ybarra, M.L. Hlavin, W.R. Selman, The dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas. J. Clin. Endocrinol. Metab. 85, 1789–1793 (2000). https://doi.org/10.1210/jcem.85.5.6611
P.D. Lees, J.D. Pickard, Hyperprolactinemia intrasellar pituitary tissue pressure, and the pituitary stalk compression syndrome. J. Neurosurg. 67, 192–196 (1987). https://doi.org/10.3171/jns.1987.67.2.0192
G. Hildebrandt, H.W. Mueller, H. Stracke, Z.M. Rap, N. Klung, Different types of postoperative diabetes insipidus and the relation to basal and stimulated serum prolactin levels in patients with hypothalamo-hypophyseal tumorous lesions. Acta Neurochir. 104, 110–120 (1990). https://doi.org/10.1007/BF01842828
A.M. Ajlan, S.B. Abdulqader, A.S. Achrol, Y. Aljamaan, A.H. Feroze, L. Katznelson, G.R. Harsh, Diabetes insipidus following endoscopic transsphenoidal surgery for pituitary adenoma. J. Neurol. Surg. B. Skull Base. 79, 117–122 (2018). https://doi.org/10.1055/s-0037-1604363
M. Araujo-Castro, F. Mariño-Sánchez, A. Acitores Cancela, A. García Fernández, S. García Duque, V. Rodríguez Berrocal, Is it possible to predict the development of diabetes insipidus after pituitary surgery? Study of 241 endoscopic transsphenoidal pituitary surgeries. J. Endocrinol. Invest 44, 1457–1464 (2021). https://doi.org/10.1007/s40618-020-01448-6
W.T. Burke, D.J. Cote, D.L. Penn, S. Luliano, K. McMillen, E.R. Laws, Diabetes insipidus after endoscopic transsphenoidal surgery. Neurosurgery 87, 949–955 (2020). https://doi.org/10.1093/neuros/nyaa148
J. Hensen, A.H.R. Fahlbusch, M. Meyer, M. Boehnert, M. Buchfelder, Prevalence, predictors and patterns of postoperative polyuria and hyponatraemia in the immediate course after transsphenoidal surgery for pituitary adenomas. Clin. Endocrinol. 50, 431–439 (1999). https://doi.org/10.1046/j.1365-2265.1999.00666.x
R.S. Joshi, M.P. Pereira, R.C. Osorio, T. Oh, A.F. Haddad, K.M. Pereira, K.C. Donohue, Z. Peeran, S. Sundhir, S. Jain, A. Beniwal, A. Chandra, S.J. Han, J.D. Rolston, P.V. Theodosopoulos, S. Kunwar, L.S. Blevins Jr, M.K. Aghi, Identifying risk factors for postoperative diabetes insipidus in more than 2500 patients undergoidng transsphenoidal surgery: a single-institution experience. J. Neurosurg. 137, 647–657 (2022). https://doi.org/10.3171/2021.11,JSN211260
E.L. Sorba, V.E. Staartjes, S. Voglis, L. Tosic, G. Brandi, O. Tschopp, C. Serra, L. Regli, Diabetes insipidus and syndrome of inappropriate antidiuresis (SIADH) after pituitary surgery: incidence and risk factors. Neurosurg. Rev. 44, 1503–1511 (2021). https://doi.org/10.1007/s10143-020-01340-0
M.E. Yasuda, D. Renedo, S. Sosa, K. Danilowicz, R. Recalde, R. Zaninovich, G. Abbati, A. Cervio, S. Giovannini, J. Villalonga, L. Ulloque-Caamaño, K. Reddy, M. Socolovsky, A. Campero, Risk factors related to transient diabetes insipidus development following transsphenoidal pituitary adenoma resection: A multicentric study. World Neurosurg. 175, e636–e643 (2023). https://doi.org/10.1016/j.wneu.2023.03.150
P. Nayak, A.S. Montaser, J. Hu, D.M. Prevedello, L.S. Kirschner, L. Ghalib, Predictors of postoperative diabetes insipidus following endoscopic resection of pituitary adenomas. J. Endocr. Soc. 2, 1010–1019 (2018). https://doi.org/10.1210/js.2018-00121
M. Schreckinger, B. Walker, J. Knepper, M. Hornyak, D. Hong, J.-M. Kim, A. Folbe, M. Guthikonda, S. Mittal, N.J. Szerlip, Post-operative diabetes insipidus after endoscopic transsphenoidal surgery. Pituitary 16, 445–451 (2013). https://doi.org/10.1007/s11102-012-0453-1
N. Alidaei, G. Sharifi, Z. Davoudi, Importance of intraoperative factors in postoperative arginine vasopressin deficiency after pituitary adenoma surgery. Endocr. Pract. 30, 253–258 (2024). https://doi.org/10.1016/j.eprac.2023.12.003
E.C. Nemergut, Z. Zuo, J.A. Jane Jr, E.R. Laws Jr, Predictors of diabetes insipidus after transsphenoidal surgery: a review of 881 patients. J. Neurosurg. 103, 448–454 (2005). https://doi.org/10.3171/jns.2005.103.3.0448
D.G. Sigounas, J.L. Sharpless, D.M.L. Cheng, T.G. Johnson, B.A. Senior, M.G. Ewend, Predictors and incidence of central diabetes insipidus after endoscopic pituitary surgery. Neurosurgery 62, 71–78 (2008). https://doi.org/10.1227/01.NEU.0000311063.10745.D8
M. Tanji, Y. Mineharu, M. Kikuchi, T. Nakagawa, T. Sakamoto, M. Yamashita, M. Matsunaga, F. Kuwata, Y. Kitada, Y. Terada, Y. Arakawa, K. Yoshida, H. Kataoka, S. Miyamoto, Intraoperative cerebrospinal fluid leak graded by Esposito grade is a predictor for diabetes insipidus after endoscopic endonasal pituitary adenoma resection. World Neurosurg. 158, e896–e902 (2022). https://doi.org/10.1016/j.wneu.2021.11.090
O. Alexopoulou, V. Everard, M. Etoa, E. Fomekong, S. Gaillard, F. Parker, C. Raftopoulos, P. Chanson, D. Maiter, Outcome of pituitary hormone deficits after surgical treatment of nonfunctioning pituitary macroadenomas. Endocrine 73, 166–176 (2021). https://doi.org/10.1007/s12020-021-02701-5
A.N. Hoang, B.G. McGahan, S. Cua, S.T. Magill, P. Nayak, A.S. Montaser, L. Ghalib, L.M. Prevedello, D.A. Hardesty, R.L. Carrau, D.M. Prevedello, Pituitary stalk stretch predicts postoperative diabetes insipidus after pituitary macroadenoma transsphenoidal resection. Oper. Neurosurg. 24, 248–255 (2023). https://doi.org/10.1227/ons.0000000000000501
K. Lin, K. Fan, S. Mu, S. Wang, Change in cephalocaudal tumor cavity diameter after transsphenoidal surgery is a predictor of diabetes insipidus in pituitary adenoma. Eur. J. Med. Res. 27, 72 (2022). https://doi.org/10.1186/s40001-022-00700-4
J. Ma, P. Gooderham, R. Akagami, S. Makarenko, Correlation of pituitary descent and diabetes insipidus after transsphenoidal pituitary macroadenoma resection. Neurosurgery 92, 1269–1275 (2023). https://doi.org/10.1227/neu.0000000000002360
H. Oh, H. Cheun, Y.J. Kim, H.K. Yoon, H. Kang, H.C. Lee, H.P. Park, J.H. Kim, Y.H. Kim, Cephalocaudal tumor diameter is a predictor of diabetes insipidus after endoscopic transsphenoidal surgery for non-functioning pituitary adenoma. Pituitary 24, 303–311 (2021). https://doi.org/10.1007/s11102-020-01108-1
L. Xue, J. Wu, J. Chen, Y. Yang, Change in the pituitary stalk deviation angle after transsphenoidal surgery can predict the development of diabetes insipidus for pituitary adenomas. Endocr. Connect. 11, e220187 (2022). https://doi.org/10.1530/EC-22-0187
B.R. Olson, J. Gumowski, D. Rubino, E.H. Oldfield, Pathophysiology of hyponatoremia after transsphenoidal pituitary surgery. J. Neurosurg. 87, 499–507 (1997). https://doi.org/10.3171/jns.1997.87.4.0499
K. Takano, [Endocrine diseases: progress in diagnosis and treatments. Topics: I. Anterior lobes of the pituitary; 3. Diagnosis and treatment of prolactinoma] Nihon. Naika. Gakkai. Zasshi 103, 841–848 (2014). https://doi.org/10.2169/naika.103.841
B.M. Arafah, K.E. Nekl, R.S. Gold, W.R. Selman, Dynamics of prolactin secretion in patients with hypopituitarism and pituitary macroadenomas. J. Clin. Endocrinol. Metab. 80, 3507–3512 (1995). https://doi.org/10.1210/jcem.80.12.8530591
H.A. Zaidi, D.J. Cote, J.P. Castlen, W.T. Burke, Y.H. Liu, T.R. Smith, E.R. Laws Jr, Time course of resolution of hyperprolactinemia after transsphenoidal surgery among patients presenting with pituitary stalk compression. World Neurosurg. 97, 2–7 (2017). https://doi.org/10.1016/j.wneu.2016.09.066
Acknowledgements
We would like to thank the nursing, ENT, and anesthesiology teams for perioperative management of the patients undergoing endoscopic endonasal pituitary surgery. We also thank Mark Cleasby, PhD from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author contributions
Conceptualization: K.S. and A.H., Methodology: K.S., N.T., A.N., and K.A., Formal analysis and investigation: A.H., and K.O., Writing – original draft preparation: K.S., Writing – review and editing: K.A. and M.M., Supervision: M.N. and M.M., All authors have read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not report animal studies. This study was approved by the ethics committee of the Kurume University School of Medicine (approval number: 18019).
Informed consent
All the participants concurred with the proposed treatment plan after all the options for the management of non-functioning pituitary adenomas and prolactinomas had been clearly explained. Informed consent was obtained from all the participants in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakata, K., Hashimoto, A., Takeshige, N. et al. Clinical and radiographic characteristics of patients with non-functioning pituitary adenomas categorized according to their serum prolactin concentration: novel predictors of postoperative transient diabetes insipidus following surgery. Endocrine (2024). https://doi.org/10.1007/s12020-024-03835-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12020-024-03835-y