Abstract
Background
Blastocystis hominis (B. hominis) is a protozoan parasite that has a worldwide distribution. Some studies have suggested a link between B. hominis and the development of irritable bowel syndrome (IBS). The objective of this study was to determine the prevalence of B. hominis in patients with IBS compared to healthy individuals.
Material and methods
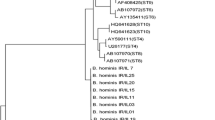
A total of 65 stool samples from patients with IBS and 65 samples from healthy individuals in northern Iran were examined. The samples were tested using various methods including direct smear, formalin ether sedimentation and culture to detect the presence of B. hominis. Additionally, polymerase chain reaction (PCR) was performed on all culture-positive isolates to confirm the results and identify the genotype.
Results
B. hominis was detected in 15.38% of IBS patients and 9.2% of the healthy group. The culture in RPMI1640 was found to be better than the formalin ether and direct smear methods. Positive samples were confirmed using the molecular method. No significant difference was observed in the order of B. hominis infection between the two groups.
Conclusions
The results of our study indicate that no significant difference was observed in the order of B. hominis infection between IBS patients and healthy groups. Therefore, further study is necessary to determine the potential pathogenic effects of this parasite and its role in causing IBS.


Similar content being viewed by others
Data availability
The data are available with the correspondence author and can be reached on request.
References
Salehi M et al (2021) Prevalence and subtype analysis of Blastocystis hominis Isolated from patients in the northeast of Iran. J Parasitol Res 2021:8821885. https://doi.org/10.1155/2021/8821885
Fletcher SM et al (2012) Enteric protozoa in the developed world: a public health perspective. Clin Microbiol Rev 25(3):420–449. https://doi.org/10.1128/CMR.05038-11
Tan KSW (2008) New insights on classification, identification, and clinical relevance of Blastocystis spp. Clin Microbiol Rev 21(4):639–665. https://doi.org/10.1128/CMR.00022-08
Norouzi P et al (2020) Investigating the prevalence of intestinal parasites with an emphasis on Strongyloides stercoralis infection in hospitalized patients: a regional report from Iran. Ann Parasitol 66(3):365–371. https://doi.org/10.17420/ap6603.275
Bilinski J et al (2021) Eosinophilic gastroenteritis and graft-versus-host disease induced by transmission of Norovirus with fecal microbiota transplant. Transpl Infect Dis 23(1):e13386. https://doi.org/10.1111/tid.13386
Roberts T et al (2013) Subtype distribution of Blastocystis isolates identified in a Sydney population and pathogenic potential of Blastocystis. Eur J Clin Microbiol Infect Dis 32(3):335–343. https://doi.org/10.1007/s10096-012-1746-z
Kaya S et al (2007) Pathogenicity of Blastocystis hominis, a clinical reevaluation. Turkiye Parazitol Derg 31(3):184–187. This reference does not have DOI. PMID: 17918055
Salvador F et al (2021) Blastocystis sp. Carriage and Irritable Bowel Syndrome: Is the Association Already Established? Biology 10(4):340. https://doi.org/10.3390/biology10040340
Kuo HY et al (2008) Clinical significance of Blastocystis hominis: experience from a medical center in northern Taiwan. J Microbiol Immunol Infect 41(3):222–226. This reference does not have DOI. PMID: 18629417
Su FH et al (2009) Blastocystis hominis infection in long-term care facilities in Taiwan: prevalence and associated clinical factors. Parasitol Res 105(4):1007–1013. https://doi.org/10.1007/s00436-009-1509-7
Hussein EM et al (2008) Pathophysiological variability of different genotypes of human Blastocystis hominis Egyptian isolates in experimentally infected rats. Parasitol Res 102(5):853–860. https://doi.org/10.1007/s00436-007-0833-z
Stensvold CR, Clark CG (2016) Current status of Blastocystis: A personal view. Parasitol Int 65(6 Pt B):763–771. https://doi.org/10.1016/j.parint.2016.05.015
Andersen LO, Stensvold CR (2016) Blastocystis in health and disease: are we moving from a clinical to a public health perspective? J Clin Microbiol 54(3):524–528. https://doi.org/10.1128/jcm.02520-15
Roberts T et al (2014) Update on the pathogenic potential and treatment options for Blastocystis sp. Gut pathogens 6:17–17. https://doi.org/10.1186/1757-4749-6-17
Salvador F et al (2016) Epidemiological and clinical profile of adult patients with Blastocystis sp. infection in Barcelona, Spain. Parasit Vectors 9(1):548. https://doi.org/10.1186/s13071-016-1827-4
Parkar U et al (2007) Direct characterization of Blastocystis from faeces by PCR and evidence of zoonotic potential. Parasitology 134(Pt 3):359–367. https://doi.org/10.1017/s0031182006001582
Karimi P et al (2023) Molecular identification of Cryptosporidium, Giardia, and Blastocystis from stray and household cats and cat owners in Tehran. Iran Scientific Reports 13(1):1554. https://doi.org/10.1038/s41598-023-28768-w
Taghipour A et al (2023) Frequency, subtypes distribution, and risk factors of Blastocystis spp. in COVID-19 patients in Tehran, capital of Iran: a case-control study. New Microbes and New Infections 51:101063. https://doi.org/10.1016/j.nmni.2022.101063
Azizian M et al (2016) Contribution of Blastocystis hominis subtypes and associated inflammatory factors in development of irritable bowel syndrome. Parasitol Res 115(5):2003–2009. https://doi.org/10.1007/s00436-016-4942-4
Haghighi L et al (2020) Prevalence and subtype identification of Blastocystis isolated from human in Shiraz city, southern Iran. Clinical Epidemiology and Global Health 8(3):840–844. https://doi.org/10.1016/j.cegh.2020.02.010
Khademvatan S et al (2017) Blastocystis and irritable bowel syndrome: Frequency and subtypes from Iranian patients. Parasitol Int 66(2):142–145. https://doi.org/10.1016/j.parint.2017.01.005
Beiromvand M et al (2017) Comparative prevalence of blastocystis in patients with the irritable bowel syndrome and healthy individuals: a case control study. Jundishapur J Microbiol 10(6). https://doi.org/10.5812/jjm.13572
Soleimani Jevinani S et al (2023) Molecular epidemiology and subtyping of Blastocystis sp. and its subtypes in celiac patients; a case control study. Microbial Pathogenesis 179:106086. https://doi.org/10.1016/j.micpath.2023.106086
Mohemmi N et al (2015) The relationship between blastocystis hominis infection and Irritable Bowel Syndrome (IBS) and comparing direct wet mount, stool culture, Formalin-Ether and trichrome staining procedures for identifying organisms. Bimonthly J Hormozgan Univ Med Sci 19(2):77–84. This reference does not have DOI.
Stensvold CR, Clark CG (2020) Pre-empting Pandora’s box: Blastocystis subtypes revisited. Trends Parasitol 36(3):229–232. https://doi.org/10.1016/j.pt.2019.12.009
Maloney JG et al (2019) Zoonotic and genetically diverse subtypes of Blastocystis in US pre-weaned dairy heifer calves. Parasitol Res 118(2):575–582. https://doi.org/10.1007/s00436-018-6149-3
Clark CG et al (2013) Recent developments in Blastocystis research. Adv Parasitol 82:1–32. https://doi.org/10.1016/b978-0-12-407706-5.00001-0
Lacy BE et al (2016) Bowel disorders. Gastroenterology 150(6):1393-1407.e5. https://doi.org/10.1053/j.gastro.2016.02.031
Botschuijver S et al (2017) Intestinal fungal dysbiosis is associated with visceral hypersensitivity in patients with irritable bowel syndrome and rats. Gastroenterology 153(4):1026–1039. https://doi.org/10.1053/j.gastro.2017.06.004
Klem F et al (2017) Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: a systematic review and meta-analysis. Gastroenterology 152(5):1042-1054.e1. https://doi.org/10.1053/j.gastro.2016.12.039
Jimenez-Gonzalez DE et al (2012) Blastocystis infection is associated with irritable bowel syndrome in a Mexican patient population. Parasitol Res 110(3):1269–1275. https://doi.org/10.1007/s00436-011-2626-7
Yakoob J et al (2004) Irritable bowel syndrome: in search of an etiology: role of Blastocystis hominis. Am J Trop Med Hyg 70(4):383–385. https://doi.org/10.4269/ajtmh.2004.70.383
Krogsgaard LR et al (2015) The prevalence of intestinal parasites is not greater among individuals with irritable bowel syndrome: a population-based case-control study. Clin Gastroenterol Hepatol 13(3):507-513.e2. https://doi.org/10.1016/j.cgh.2014.07.065
Jahangiri P et al. (2012) Irritable Bowel Syndrome in Iran: SEPAHAN Systematic Review No. 1. Int J Prev Med 3(Suppl 1):S1–S9. This reference does not have DOI. PMID: 22826748
Najafi N et al (2016) Disseminated strongyloidiasis in an Iranian immunocompromised patient: a case report. Iran J Parasitol 11(2):279–283. This reference does not have DOI. PMID: 28096866
Mearin F, Rey E, Balboa A (2016) Functional and motor gastrointestinal disorders. Gastroenterol Hepatol 39(Suppl 1):3–13. https://doi.org/10.1016/s0210-5705(16)30169-8
Zman V, Khan KZ (1994) A comparison of direct microscopy with culture for the diagnosis of Blastocystis hominis. Southeast Asian J Trop Med Public Health 25(4):792–793. This reference does not have DOI. PMID: 7667737
Alfellani MA et al (2013) Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Trop 126(1):11–18. https://doi.org/10.1016/j.actatropica.2012.12.011
Roberts T et al (2011) Comparison of microscopy, culture, and conventional polymerase chain reaction for detection of blastocystis sp. in clinical stool samples. Am J Trop Med Hyg 84(2): 308–312. https://doi.org/10.4269/ajtmh.2011.10-0447
Shafiei Z et al (2020) Parasitic infections in irritable bowel syndrome patients: evidence to propose a possible link, based on a case–control study in the south of Iran. BMC Res Notes 13(1):264. https://doi.org/10.1186/s13104-020-05118-x
Wawrzyniak I et al (2013) Blastocystis, an unrecognized parasite: an overview of pathogenesis and diagnosis. Ther Adv Infect Dis 1(5):167–178. https://doi.org/10.1177/2049936113504754
Nourrisson C et al (2014) Blastocystis is associated with decrease of fecal microbiota protective bacteria: comparative analysis between patients with irritable bowel syndrome and control subjects. PLoS ONE 9(11):e111868. https://doi.org/10.1371/journal.pone.0111868
Cekin AH et al (2012) Blastocystosis in patients with gastrointestinal symptoms: a case-control study. BMC Gastroenterol 12:122. https://doi.org/10.1186/1471-230x-12-122
Ramirez-Miranda ME et al (2010) Parasites in Mexican patients with irritable bowel syndrome: a case-control study. Parasit Vectors 3:96. https://doi.org/10.1186/1756-3305-3-96
Das R et al (2016) Molecular Characterization and Subtyping of Blastocystis Species in Irritable Bowel Syndrome Patients from North India. PLoS ONE 11(1):e0147055. https://doi.org/10.1371/journal.pone.0147055
Surangsrirat S et al (2010) Assessment of the association between Blastocystis infection and irritable bowel syndrome. J Med Assoc Thai 93(Suppl 6):S119–S124. This reference does not have DOI. PMID: 21280524
Vargas-Sanchez GB et al (2015) Blastocystis isolates from patients with irritable bowel syndrome and from asymptomatic carriers exhibit similar parasitological loads, but significantly different generation times and genetic variability across multiple subtypes. PLoS ONE 10(4):e0124006. https://doi.org/10.1371/journal.pone.0124006
Cremonini F, Talley NJ (2005) Irritable bowel syndrome: epidemiology, natural history, health care seeking and emerging risk factors. Gastroenterol Clin North Am 34(2):189–204. https://doi.org/10.1016/j.gtc.2005.02.008
Park DW et al (2010) The differences in prevalence and sociodemographic characteristics of irritable bowel syndrome according to Rome II and Rome III. J Neurogastroenterol Motil 16(2):186–193. https://doi.org/10.5056/jnm.2010.16.2.186
Poirier P et al (2012) New insights into Blastocystis spp.: a potential link with irritable bowel syndrome. PLoS Pathog 8(3):e1002545. https://doi.org/10.1371/journal.ppat.1002545
Idris NS et al (2010) Intestinal parasitic infection of immunocompromised children with diarrhoea: clinical profile and therapeutic response. J Infect Dev Countries 4(05):309–317. https://doi.org/10.3855/jidc.275
Boorom KF et al (2008) Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection. Parasit Vectors 1(1):40. https://doi.org/10.1186/1756-3305-1-40
Yakoob J et al (2010) Irritable bowel syndrome: is it associated with genotypes of Blastocystis hominis. Parasitol Res 106(5):1033–1038. https://doi.org/10.1007/s00436-010-1761-x
Jantermtor S et al (2013) Subtype identification of Blastocystis spp. isolated from patients in a major hospital in northeastern Thailand. Parasitol Res 112(4):1781–1786. https://doi.org/10.1007/s00436-012-3218-x
Kesuma Y et al (2019) Blastocystis ST-1 is associated with Irritable Bowel Syndrome-diarrhoea (IBS-D) in Indonesian adolescences. Parasite Epidemiol Control 6:e00112. https://doi.org/10.1016/j.parepi.2019.e00112
Dogruman-Al F et al (2008) A possible link between subtype 2 and asymptomatic infections of Blastocystis hominis. Parasitol Res 103(3):685–689. https://doi.org/10.1007/s00436-008-1031-3
Stensvold CR, Alfellani M, Clark CG (2012) Levels of genetic diversity vary dramatically between Blastocystis subtypes. Infect Genet Evol 12(2):263–273. https://doi.org/10.1016/j.meegid.2011.11.002
Stanley SL (2003) Amoebiasis. The Lancet 361(9362):1025–1034. https://doi.org/10.1016/S0140-6736(03)12830-9
van der Veek PPJ et al (2005) Role of Tumor Necrosis Factor-α and Interleukin-10 Gene Polymorphisms in Irritable Bowel Syndrome. Official J Am Coll Gastroenterol | ACG 100(11):2510–2516. https://doi.org/10.1111/j.1572-0241.2005.00257.x
Abou Gamra MM et al (2011) The potential use of 29 kDa protein as a marker of pathogenicity and diagnosis of symptomatic infections with Blastocystis hominis. Parasitol Res 108(5):1139–1146. https://doi.org/10.1007/s00436-010-2156-8
Puthia MK et al (2006) Blastocystis ratti induces contact-independent apoptosis, F-actin rearrangement, and barrier function disruption in IEC-6 cells. Infect Immun 74(7):4114–4123. https://doi.org/10.1128/iai.00328-06
Cenac N et al (2007) Role for protease activity in visceral pain in irritable bowel syndrome. J Clin Invest 117(3):636–647. https://doi.org/10.1172/jci29255
Gecse K et al (2008) Increased faecal serine protease activity in diarrhoeic IBS patients: a colonic lumenal factor impairing colonic permeability and sensitivity. Gut 57(5):591–599. https://doi.org/10.1136/gut.2007.140210
Puthia MK et al (2005) Degradation of human secretory immunoglobulin A by Blastocystis. Parasitol Res 97(5):386–389. https://doi.org/10.1007/s00436-005-1461-0
Ozyurt M et al (2008) Molecular epidemiology of Blastocystis infections in Turkey. Parasitol Int 57(3):300–306. https://doi.org/10.1016/j.parint.2008.01.004
Engsbro AL et al (2014) Prevalence, incidence, and risk factors of intestinal parasites in Danish primary care patients with irritable bowel syndrome. Scand J Infect Dis 46(3):204–209. https://doi.org/10.3109/00365548.2013.861609
Forsell J et al (2012) Subtype analysis of Blastocystis isolates in Swedish patients. Eur J Clin Microbiol Infect Dis 31(7):1689–1696. https://doi.org/10.1007/s10096-011-1416-6
Petersen AM et al (2013) Active ulcerative colitis associated with low prevalence of Blastocystis and Dientamoeba fragilis infection. Scand J Gastroenterol 48(5):638–639. https://doi.org/10.3109/00365521.2013.780094
Acknowledgements
We would like to appreciate the assistance offered by the colleagues at Razi Hospital, Mazandaran University of Medical Science, Qaemshahr, Iran.
Funding
Vice Chancellor for Research and Technology, Hamadan University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors state that there is no conflict of interest.
Approval Statement
The current study was supported financially by Hamadan University of Medical Science, Project No. IR.UMSHA.REC.1400.857.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maghsood, A.H., Kayedimajd, S., Motavallihaghi, S. et al. Irritable Bowel Syndrome Associated with Blastocystis hominis or Without Relationship to It? A Case–Control Study and Minireview. Acta Parasit. 69, 639–647 (2024). https://doi.org/10.1007/s11686-023-00787-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11686-023-00787-7