Abstract
The characteristic genetic abnormality of neuroendocrine neoplasms (NENs), a heterogeneous group of tumors found in various organs, remains to be identified. Here, based on the analysis of the splicing variants of an oncogene Focal Adhesion Kinase (FAK) in The Cancer Genome Atlas datasets that contain 9193 patients of 33 cancer subtypes, we found that Box 6/Box 7-containing FAK variants (FAK6/7) were observed in 7 (87.5%) of 8 pancreatic neuroendocrine carcinomas and 20 (11.76%) of 170 pancreatic ductal adenocarcinomas (PDACs). We tested FAK variants in 157 tumor samples collected from Chinese patients with pancreatic tumors, and found that FAK6/7 was positive in 34 (75.6%) of 45 pancreatic NENs, 19 (47.5%) of 40 pancreatic solid pseudopapillary neoplasms, and 2 (2.9%) of 69 PDACs. We further tested FAK splicing variants in breast neuroendocrine carcinoma (BrNECs), and found that FAK6/7 was positive in 14 (93.3%) of 15 BrNECs but 0 in 23 non-NEC breast cancers. We explored the underlying mechanisms and found that a splicing factor serine/arginine repetitive matrix protein 4 (SRRM4) was overexpressed in FAK6/7-positive pancreatic tumors and breast tumors, which promoted the formation of FAK6/7 in cells. These results suggested that FAK6/7 could be a biomarker of NENs and represent a potential therapeutic target for these orphan diseases.
Similar content being viewed by others
References
Jiao Y, Shi C, Edil BH, de Wilde RF, Klimstra DS, Maitra A, Schulick RD, Tang LH, Wolfgang CL, Choti MA, Velculescu VE, Diaz LA Jr, Vogelstein B, Kinzler KW, Hruban RH, Papadopoulos N. DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science 2011; 331(6021): 1199–1203
Sun H, Dai S, Xu J, Liu L, Yu J, Sun T. Primary neuroendocrine tumor of the breast: current understanding and future perspectives. Front Oncol 2022; 12: 848485
Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer. Lancet 2020; 395(10242): 2008–2020
Cives M, Strosberg JR. Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin 2018; 68(6): 471–487
Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, Washington KM, Carneiro F, Cree IA; WHO Classification of Tumours Editorial Board. The 2019 WHO classification of tumours of the digestive system. Histopathology 2020; 76(2): 182–188
Pokrzywa CJ, Abbott DE, Matkowskyj KA, Ronnekleiv-Kelly SM, Winslow ER, Weber SM, Fisher AV. Natural history and treatment trends in pancreatic cancer subtypes. J Gastrointest Surg 2019; 23(4): 768–778
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71(3): 209–249
Connor AA, Gallinger S. Pancreatic cancer evolution and heterogeneity: integrating omics and clinical data. Nat Rev Cancer 2022; 22(3): 131–142
Ishida H, Lam AK. Pancreatic neuroendocrine neoplasms: updates on genomic changes in inherited tumour syndromes and sporadic tumours based on WHO classification. Crit Rev Oncol Hematol 2022; 172: 103648
Sorbye H, Strosberg J, Baudin E, Klimstra DS, Yao JC. Gastroenteropancreatic high-grade neuroendocrine carcinoma. Cancer 2014; 120(18): 2814–2823
Dinarvand P, Lai J. Solid pseudopapillary neoplasm of the pancreas: a rare entity with unique features. Arch Pathol Lab Med 2017; 141(7): 990–995
Santini D, Poli F, Lega S. Solid-papillary tumors of the pancreas: histopathology. JOP 2006; 7(1): 131–136
La Rosa S, Bongiovanni M. Pancreatic solid pseudopapillary neoplasm: key pathologic and genetic features. Arch Pathol Lab Med 2020; 144(7): 829–837
Wang S, Zheng Y, Yang F, Zhu L, Zhu XQ, Wang ZF, Wu XL, Zhou CH, Yan JY, Hu BY, Kong B, Fu DL, Bruns C, Zhao Y, Qin LX, Dong QZ. The molecular biology of pancreatic adenocarcinoma: translational challenges and clinical perspectives. Signal Transduct Target Ther 2021; 6(1): 249
Qian Y, Gong Y, Fan Z, Luo G, Huang Q, Deng S, Cheng H, Jin K, Ni Q, Yu X, Liu C. Molecular alterations and targeted therapy in pancreatic ductal adenocarcinoma. J Hematol Oncol 2020; 13(1): 130
Fraenkel M, Kim MK, Faggiano A, Valk GD. Epidemiology of gastroenteropancreatic neuroendocrine tumours. Best Pract Res Clin Gastroenterol 2012; 26(6): 691–703
Gao C, Wang Y, Broaddus R, Sun L, Xue F, Zhang W. Exon 3 mutations of CTNNB1 drive tumorigenesis: a review. Oncotarget 2018; 9(4): 5492–5508
Omiyale AO. Solid pseudopapillary neoplasm of the pancreas. World J Hepatol 2021; 13(8): 896–903
Schaller MD. Cellular functions of FAK kinases: insight into molecular mechanisms and novel functions. J Cell Sci 2010; 123(7): 1007–1013
Sulzmaier FJ, Jean C, Schlaepfer DD. FAK in cancer: mechanistic findings and clinical applications. Nat Rev Cancer 2014; 14(9): 598–610
Jiang H, Hegde S, Knolhoff BL, Zhu Y, Herndon JM, Meyer MA, Nywening TM, Hawkins WG, Shapiro IM, Weaver DT, Pachter JA, Wang-Gillam A, DeNardo DG. Targeting focal adhesion kinase renders pancreatic cancers responsive to checkpoint immunotherapy. Nat Med 2016; 22(8): 851–860
Davidson C, Taggart D, Sims AH, Lonergan DW, Canel M, Serrels A. FAK promotes stromal PD-L2 expression associated with poor survival in pancreatic cancer. Br J Cancer 2022; 127(10): 1893–1905
Stokes JB, Adair SJ, Slack-Davis JK, Walters DM, Tilghman RW, Hershey ED, Lowrey B, Thomas KS, Bouton AH, Hwang RF, Stelow EB, Parsons JT, Bauer TW. Inhibition of focal adhesion kinase by PF-562,271 inhibits the growth and metastasis of pancreatic cancer concomitant with altering the tumor microenvironment. Mol Cancer Ther 2011; 10(11): 2135–2145
Francois RA, Maeng K, Nawab A, Kaye FJ, Hochwald SN, Zajac-Kaye M. Targeting focal adhesion kinase and resistance to mTOR inhibition in pancreatic neuroendocrine tumors. J Natl Cancer Inst 2015; 107(8): djv123
Zaghdoudi S, Decaup E, Belhabib I, Samain R, Cassant-Sourdy S, Rochotte J, Brunel A, Schlaepfer D, Cros J, Neuzillet C, Strehaiano M, Alard A, Tomasini R, Rajeeve V, Perraud A, Mathonnet M, Pearce OM, Martineau Y, Pyronnet S, Bousquet C, Jean C. FAK activity in cancer-associated fibroblasts is a prognostic marker and a druggable key metastatic player in pancreatic cancer. EMBO Mol Med 2020; 12(11): e12010
Roy-Luzarraga M, Reynolds LE, de Luxán-Delgado B, Maiques O, Wisniewski L, Newport E, Rajeeve V, Drake RJG, Gómez-Escudero J, Richards FM, Weller C, Dormann C, Meng YM, Vermeulen PB, Saur D, Sanz-Moreno V, Wong PP, Géraud C, Cutillas PR, Hodivala-Dilke K. Suppression of endothelial cell FAK expression reduces pancreatic ductal adenocarcinoma metastasis after gemcitabine treatment. Cancer Res 2022; 82(10): 1909–1925
Lander VE, Belle JI, Kingston NL, Herndon JM, Hogg GD, Liu X, Kang LI, Knolhoff BL, Bogner SJ, Baer JM, Zuo C, Borcherding NC, Lander DP, Mpoy C, Scott J, Zahner M, Rogers BE, Schwarz JK, Kim H, DeNardo DG. Stromal reprogramming by FAK inhibition overcomes radiation resistance to allow for immune priming and response to checkpoint blockade. Cancer Discov 2022; 12(12): 2774–2799
Murphy KJ, Reed DA, Vennin C, Conway JRW, Nobis M, Yin JX, Chambers CR, Pereira BA, Lee V, Filipe EC, Trpceski M, Ritchie S, Lucas MC, Warren SC, Skhinas JN, Magenau A, Metcalf XL, Stoehr J, Major G, Parkin A, Bidanel R, Lyons RJ, Zaratzian A, Tayao M, Da Silva A, Abdulkhalek L; Australian Pancreatic Genome Initiative (APGI); Australian Pancreatic Cancer Matrix Atlas (APMA); Gill AJ, Johns AL, Biankin AV, Samra J, Grimmond SM, Chou A, Goetz JG, Samuel MS, Lyons JG, Burgess A, Caldon CE, Horvath LG, Daly RJ, Gadegaard N, Wang Y, Sansom OJ, Morton JP, Cox TR, Pajic M, Herrmann D, Timpson P. Intravital imaging technology guides FAK-mediated priming in pancreatic cancer precision medicine according to Merlin status. Sci Adv 2021; 7(40): eabh0363
Zhang J, Francois R, Iyer R, Seshadri M, Zajac-Kaye M, Hochwald SN. Current understanding of the molecular biology of pancreatic neuroendocrine tumors. J Natl Cancer Inst 2013; 105(14): 1005–1017
Moen I, Gebre M, Alonso-Camino V, Chen D, Epstein D, McDonald DM. Anti-metastatic action of FAK inhibitor OXA-11 in combination with VEGFR-2 signaling blockade in pancreatic neuroendocrine tumors. Clin Exp Metastasis 2015; 32(8): 799–817
Stanley RF, Abdel-Wahab O. Dysregulation and therapeutic targeting of RNA splicing in cancer. Nat Cancer 2022; 3(5): 536–546
Burgaya F, Toutant M, Studler JM, Costa A, Le Bert M, Gelman M, Girault JA. Alternatively spliced focal adhesion kinase in rat brain with increased autophosphorylation activity. J Biol Chem 1997; 272(45): 28720–28725
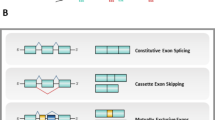
Corsi JM, Rouer E, Girault JA, Enslen H. Organization and post-transcriptional processing of focal adhesion kinase gene. BMC Genomics 2006; 7(1): 198
Devaud C, Tilkin-Mariamé AF, Vignolle-Vidoni A, Souleres P, Denadai-Souza A, Rolland C, Duthoit C, Blanpied C, Chabot S, Bouillé P, Lluel P, Vergnolle N, Racaud-Sultan C, Ferrand A. FAK alternative splice mRNA variants expression pattern in colorectal cancer. Int J Cancer 2019; 145(2): 494–502
Fang XQ, Liu XF, Yao L, Chen CQ, Gu ZD, Ni PH, Zheng XM, Fan QS. Somatic mutational analysis of FAK in breast cancer: a novel gain-of-function mutation due to deletion of exon 33. Biochem Biophys Res Commun 2014; 443(2): 363–369
Ignjatović VB, Janković Miljuš JR, Rončević JV, Tatić SB, Išić Denčić TM, Ɖorić IƉ, Šelemetjev SA. Focal adhesion kinase splicing and protein activation in papillary thyroid carcinoma progression. Histochem Cell Biol 2022; 157(2): 183–194
Zhou B, Wang GZ, Wen ZS, Zhou YC, Huang YC, Chen Y, Zhou GB. Somatic mutations and splicing variants of focal adhesion kinase in non-small cell lung cancer. J Natl Cancer Inst 2018; 110(2): 195–204
Wang Z, Jensen MA, Zenklusen JC. A practical guide to The Cancer Genome Atlas (TCGA). Methods Mol Biol 2016; 1418: 111–141
Ryan M, Wong WC, Brown R, Akbani R, Su X, Broom B, Melott J, Weinstein J. TCGASpliceSeq a compendium of alternative mRNA splicing in cancer. Nucleic Acids Res 2016; 44(D1): D1018–D1022
Ghandi M, Huang FW, Jané-Valbuena J, Kryukov GV, Lo CC, McDonald ER 3rd, Barretina J, Gelfand ET, Bielski CM, Li H, Hu K, Andreev-Drakhlin AY, Kim J, Hess JM, Haas BJ, Aguet F, Weir BA, Rothberg MV, Paolella BR, Lawrence MS, Akbani R, Lu Y, Tiv HL, Gokhale PC, de Weck A, Mansour AA, Oh C, Shih J, Hadi K, Rosen Y, Bistline J, Venkatesan K, Reddy A, Sonkin D, Liu M, Lehar J, Korn JM, Porter DA, Jones MD, Golji J, Caponigro G, Taylor JE, Dunning CM, Creech AL, Warren AC, McFarland JM, Zamanighomi M, Kauffmann A, Stransky N, Imielinski M, Maruvka YE, Cherniack AD, Tsherniak A, Vazquez F, Jaffe JD, Lane AA, Weinstock DM, Johannessen CM, Morrissey MP, Stegmeier F, Schlegel R, Hahn WC, Getz G, Mills GB, Boehm JS, Golub TR, Garraway LA, Sellers WR. Next-generation characterization of the Cancer Cell Line Encyclopedia. Nature 2019; 569(7757): 503–508
Shen W, Song Z, Zhong X, Huang M, Shen D, Gao P, Qian X, Wang M, He X, Wang T, Li S, Song X. Sangerbox: a comprehensive, interaction-friendly clinical bioinformatics analysis platform. iMeta 2022; 1(3): e36
Li T, Fan J, Wang B, Traugh N, Chen Q, Liu JS, Li B, Liu XS. TIMER: a web server for comprehensive analysis of tumor-infiltrating immune cells. Cancer Res 2017; 77(21): e108–e110
Lánczky A, Győrffy B. Web-based survival analysis tool tailored for medical research (KMplot): development and implementation. J Med Internet Res 2021; 23(7): e27633
Zhang C, Zhang J, Liang F, Guo H, Gao S, Yang F, Guo H, Wang G, Wang W, Zhou G. Innate immune checkpoint Siglec10 in cancers: mining of comprehensive omics data and validation in patient samples. Front Med 2022; 16(4): 596–609
Zhang D, Xu X, Ye Q. Metabolism and immunity in breast cancer. Front Med 2021; 15(2): 178–207
Seiler M, Peng S, Agrawal AA, Palacino J, Teng T, Zhu P, Smith PG; Cancer Genome Atlas Research Network; Buonamici S, Yu L. Somatic mutational landscape of splicing factor genes and their functional consequences across 33 cancer types. Cell Rep 2018; 23(1): 282–296.e4
Calarco JA, Superina S, O’Hanlon D, Gabut M, Raj B, Pan Q, Skalska U, Clarke L, Gelinas D, van der Kooy D, Zhen M, Ciruna B, Blencowe BJ. Regulation of vertebrate nervous system alternative splicing and development by an SR-related protein. Cell 2009; 138(5): 898–910
Torres-Méndez A, Bonnal S, Marquez Y, Roth J, Iglesias M, Permanyer J, Almudí I, O’Hanlon D, Guitart T, Soller M, Gingras AC, Gebauer F, Rentzsch F, Blencowe BJ, Valcárcel J, Irimia M. A novel protein domain in an ancestral splicing factor drove the evolution of neural microexons. Nat Ecol Evol 2019; 3(4): 691–701
Jensen KB, Dredge BK, Stefani G, Zhong R, Buckanovich RJ, Okano HJ, Yang YY, Darnell RB. Nova-1 regulates neuron-specific alternative splicing and is essential for neuronal viability. Neuron 2000; 25(2): 359–371
Ule J, Ule A, Spencer J, Williams A, Hu JS, Cline M, Wang H, Clark T, Fraser C, Ruggiu M, Zeeberg BR, Kane D, Weinstein JN, Blume J, Darnell RB. Nova regulates brain-specific splicing to shape the synapse. Nat Genet 2005; 37(8): 844–852
Raj B, Irimia M, Braunschweig U, Sterne-Weiler T, O’Hanlon D, Lin ZY, Chen GI, Easton LE, Ule J, Gingras AC, Eyras E, Blencowe BJ. A global regulatory mechanism for activating an exon network required for neurogenesis. Mol Cell 2014; 56(1): 90–103
Shih HP, Panlasigui D, Cirulli V, Sander M. ECM signaling regulates collective cellular dynamics to control pancreas branching morphogenesis. Cell Rep 2016; 14(2): 169–179
Rodriguez UA, Dahiya S, Raymond ML, Gao C, Martins-Cargill CP, Piganelli JD, Gittes GK, Hu J, Esni F. Focal adhesion kinase-mediated signaling controls the onset of pancreatic cell differentiation. Development 2022; 149(17): dev200761
Serrels A, Lund T, Serrels B, Byron A, McPherson RC, von Kriegsheim A, Gómez-Cuadrado L, Canel M, Muir M, Ring JE, Maniati E, Sims AH, Pachter JA, Brunton VG, Gilbert N, Anderton SM, Nibbs RJ, Frame MC. Nuclear FAK controls chemokine transcription, Tregs, and evasion of anti-tumor immunity. Cell 2015; 163(1): 160–173
Demircioglu F, Wang J, Candido J, Costa ASH, Casado P, de Luxan Delgado B, Reynolds LE, Gomez-Escudero J, Newport E, Rajeeve V, Baker AM, Roy-Luzarraga M, Graham TA, Foster J, Wang Y, Campbell JJ, Singh R, Zhang P, Schall TJ, Balkwill FR, Sosabowski J, Cutillas PR, Frezza C, Sancho P, Hodivala-Dilke K. Cancer associated fibroblast FAK regulates malignant cell metabolism. Nat Commun 2020; 11(1): 1290
Tavora B, Reynolds LE, Batista S, Demircioglu F, Fernandez I, Lechertier T, Lees DM, Wong PP, Alexopoulou A, Elia G, Clear A, Ledoux A, Hunter J, Perkins N, Gribben JG, Hodivala-Dilke KM. Endothelial-cell FAK targeting sensitizes tumours to DNA-damaging therapy. Nature 2014; 514(7520): 112–116
Rigiracciolo DC, Cirillo F, Talia M, Muglia L, Gutkind JS, Maggiolini M, Lappano R. Focal adhesion kinase fine tunes multifaced signals toward breast cancer progression. Cancers (Basel) 2021; 13(4): 645
Luo M, Fan H, Nagy T, Wei H, Wang C, Liu S, Wicha MS, Guan JL. Mammary epithelial-specific ablation of the focal adhesion kinase suppresses mammary tumorigenesis by affecting mammary cancer stem/progenitor cells. Cancer Res 2009; 69(2): 466–474
Llewellyn RA, Gutknecht MF, Thomas KS, Conaway MR, Bouton AH. Focal adhesion kinase (FAK) deficiency in mononuclear phagocytes alters murine breast tumor progression. Am J Cancer Res 2018; 8(4): 675–687
Gallego-Paez LM, Bordone MC, Leote AC, Saraiva-Agostinho N, Ascensão-Ferreira M, Barbosa-Morais NL. Alternative splicing: the pledge, the turn, and the prestige: the key role of alternative splicing in human biological systems. Hum Genet 2017; 136(9): 1015–1042
Ladomery M. Aberrant alternative splicing is another hallmark of cancer. Int J Cell Biol 2013; 2013: 463786
Quesnel-Vallières M, Irimia M, Cordes SP, Blencowe BJ. Essential roles for the splicing regulator nSR100/SRRM4 during nervous system development. Genes Dev 2015; 29(7): 746–759
Irimia M, Weatheritt RJ, Ellis JD, Parikshak NN, Gonatopoulos-Pournatzis T, Babor M, Quesnel-Vallières M, Tapial J, Raj B, O’Hanlon D, Barrios-Rodiles M, Sternberg MJ, Cordes SP, Roth FP, Wrana JL, Geschwind DH, Blencowe BJ. A highly conserved program of neuronal microexons is misregulated in autistic brains. Cell 2014; 159(7): 1511–1523
Head SA, Hernandez-Alias X, Yang JS, Ciampi L, Beltran-Sastre V, Torres-Méndez A, Irimia M, Schaefer MH, Serrano L. Silencing of SRRM4 suppresses microexon inclusion and promotes tumor growth across cancers. PLoS Biol 2021; 19(2): e3001138
Li Y, Donmez N, Sahinalp C, Xie N, Wang Y, Xue H, Mo F, Beltran H, Gleave M, Wang Y, Collins C, Dong X. SRRM4 drives neuroendocrine transdifferentiation of prostate adenocarcinoma under androgen receptor pathway inhibition. Eur Urol 2017; 71(1): 68–78
Zhang X, Coleman IM, Brown LG, True LD, Kollath L, Lucas JM, Lam HM, Dumpit R, Corey E, Chéry L, Lakely B, Higano CS, Montgomery B, Roudier M, Lange PH, Nelson PS, Vessella RL, Morrissey C. SRRM4 expression and the loss of REST activity may promote the emergence of the neuroendocrine phenotype in castration-resistant prostate cancer. Clin Cancer Res 2015; 21(20): 4698–4708
Gan Y, Li Y, Long Z, Lee AR, Xie N, Lovnicki JM, Tang Y, Chen X, Huang J, Dong X. Roles of alternative RNA splicing of the Bif-1 gene by SRRM4 during the development of treatment-induced neuroendocrine prostate cancer. EBioMedicine 2018; 31: 267–275
Li Y, Xie N, Chen R, Lee AR, Lovnicki J, Morrison EA, Fazli L, Zhang Q, Musselman CA, Wang Y, Huang J, Gleave ME, Collins C, Dong X. RNA splicing of the BHC80 gene contributes to neuroendocrine prostate cancer progression. Eur Urol 2019; 76(2): 157–166
Zuccato C, Tartari M, Crotti A, Goffredo D, Valenza M, Conti L, Cataudella T, Leavitt BR, Hayden MR, Timmusk T, Rigamonti D, Cattaneo E. Huntingtin interacts with REST/NRSF to modulate the transcription of NRSE-controlled neuronal genes. Nat Genet 2003; 35(1): 76–83
Shimojo M, Shudo Y, Ikeda M, Kobashi T, Ito S. The small cell lung cancer-specific isoform of RE1-silencing transcription factor (REST) is regulated by neural-specific Ser/Arg repeat-related protein of 100 kDa (nSR100). Mol Cancer Res 2013; 11(10): 1258–1268
Acknowledgements
This work was supported by the Key Project of the National Natural Science Foundation of China (No. 81830093), the National Key Research and Development Program of China (Nos. 2020YFC2002705, 2020YFA0803300, and 2022YFA1103900), the CAMS Innovation Fund for Medical Sciences (CIFMS; Nos. 2022-RC310-05 and 2021-RC310-003), the CAMS Initiative for Innovative Medicine (Nos. 2021-I2M-1-014, 2022-I2M-2-001, and 2021-I2M-1-021), and the National Natural Science Foundation of China (Nos. 82073092 and 82273076).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest Dawei Xie, Zheng Wang, Beibei Sun, Liwei Qu, Musheng Zeng, Lin Feng, Mingzhou Guo, Jihui Hao, and Guizhen Wang declare that they have no conflict of interest. Guangbiao Zhou is the Executive Deputy Editor-in-Chief of Frontiers of Medicine, and he was excluded from the peer-review process and all editorial decisions related to the acceptance and publication of this article. Peer-review was handled independently by the other editors to minimise bias.
The study was approved by the research ethics committee of the Cancer Hospital, Chinese Academy of Medical Sciences and the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Additional informed consent was obtained from all patients, whose identifying information is included in this article.
Supplementary materials for
11684_2023_1009_MOESM1_ESM.pdf
High frequency of alternative splicing variants of the oncogene focal adhesive kinase in neuroendocrine tumors of pancreas and breast
Rights and permissions
About this article
Cite this article
Xie, D., Wang, Z., Sun, B. et al. High frequency of alternative splicing variants of the oncogene Focal Adhesion Kinase in neuroendocrine tumors of the pancreas and breast. Front. Med. 17, 907–923 (2023). https://doi.org/10.1007/s11684-023-1009-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11684-023-1009-7