Abstract
Background
Outcomes of rectal adenocarcinoma vary considerably. Composite “textbook oncologic outcome” (TOO) is a single metric that estimates optimal clinical performance for cancer surgery.
Methods
Patients with stage II/III rectal adenocarcinoma who underwent single-agent neoadjuvant chemoradiation and proctectomy within 5–12 weeks were identified in the National Cancer Database (NCDB). TOO was defined as achievement of negative distal and circumferential resection margin (CRM), retrieval of ≥ 12 nodes, no 90-day mortality, and length of stay (LOS) < 75th percentile of corresponding year’s range. Multivariable logistic regression was used to identify predictors of TOO.
Results
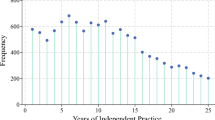
Among 318,225 patients, 8869 met selection criteria. Median age was 62 years (IQR 54–71), and 5550 (62.6%) were males. Low anterior resection was the most common procedure (LAR, 6,037 (68.1%) and 3084 (34.8%) were treated at a high-volume center (≥ 20 rectal resections/year). TOO was achieved in 3967 patients (44.7%). Several components of TOO were achieved commonly, including negative CRM (87.4%), no 90-day mortality (98.0%), no readmission (93.0%), and no prolonged hospitalization (78.8%). Logistic regression identified increasing age, non-private insurance, low-volume centers, open approach, Black race, Charlson score ≥ 3, and abdominoperineal resection (APR) as predictors of failure to achieve TOO. Over time, TOOs were attained more commonly which correlated with increased minimally invasive surgery (MIS) adoption. TOO achievement was associated with improved survival.
Conclusions
Rectal adenocarcinoma patients achieve TOO uncommonly. Treatment at high-volume centers and MIS approach were among modifiable factors associated with TOO in this study.




Similar content being viewed by others
References
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-64. doi:https://doi.org/10.3322/caac.21601.
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351(17):1731-40. doi:https://doi.org/10.1056/NEJMoa040694.
Heald RJ. The 'Holy Plane' of rectal surgery. J R Soc Med. 1988;81(9):503-8.
Ma B, Gao P, Wang H, Xu Q, Song Y, Huang X et al. What has preoperative radio(chemo)therapy brought to localized rectal cancer patients in terms of perioperative and long-term outcomes over the past decades? A systematic review and meta-analysis based on 41,121 patients. Int J Cancer. 2017;141(5):1052-65. doi:https://doi.org/10.1002/ijc.30805.
Dorrance HR, Docherty GM, O'Dwyer PJ. Effect of surgeon specialty interest on patient outcome after potentially curative colorectal cancer surgery. Dis Colon Rectum. 2000;43(4):492-8. doi:https://doi.org/10.1007/BF02237192.
Archampong D, Borowski D, Wille-Jorgensen P, Iversen LH. Workload and surgeon's specialty for outcome after colorectal cancer surgery. Cochrane Database Syst Rev. 2012(3):CD005391. doi:https://doi.org/10.1002/14651858.CD005391.pub3.
Khani MH, Smedh K. Centralization of rectal cancer surgery improves long-term survival. Colorectal Dis. 2010;12(9):874-9. doi:https://doi.org/10.1111/j.1463-1318.2009.02098.x.
Ricciardi R, Roberts PL, Read TE, Baxter NN, Marcello PW, Schoetz DJ. Who performs proctectomy for rectal cancer in the United States? Dis Colon Rectum. 2011;54(10):1210-5. doi:https://doi.org/10.1097/DCR.0b013e31822867a5.
Ricciardi R, Roberts PL, Read TE, Marcello PW, Schoetz DJ, Baxter NN. Variability in reconstructive procedures following rectal cancer surgery in the United States. Dis Colon Rectum. 2010;53(6):874-80. doi:https://doi.org/10.1007/DCR.0b013e3181cf6f58.
Huebner M, Hubner M, Cima RR, Larson DW. Timing of complications and length of stay after rectal cancer surgery. J Am Coll Surg. 2014;218(5):914-9. doi:https://doi.org/10.1016/j.jamcollsurg.2013.12.042.
Monson JR, Probst CP, Wexner SD, Remzi FH, Fleshman JW, Garcia-Aguilar J et al. Failure of evidence-based cancer care in the United States: the association between rectal cancer treatment, cancer center volume, and geography. Ann Surg. 2014;260(4):625–31; discussion 31–2. doi:https://doi.org/10.1097/SLA.0000000000000928.
Klos CL, Bordeianou LG, Sylla P, Chang Y, Berger DL. The prognostic value of lymph node ratio after neoadjuvant chemoradiation and rectal cancer surgery. Dis Colon Rectum. 2011;54(2):171-5. doi:https://doi.org/10.1007/DCR.0b013e3181fd677d.
Wibe A, Rendedal PR, Svensson E, Norstein J, Eide TJ, Myrvold HE et al. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002;89(3):327-34. doi:https://doi.org/10.1046/j.0007-1323.2001.02024.x.
Kolfschoten NE, Kievit J, Gooiker GA, van Leersum NJ, Snijders HS, Eddes EH et al. Focusing on desired outcomes of care after colon cancer resections; hospital variations in 'textbook outcome'. Eur J Surg Oncol. 2013;39(2):156-63. doi:https://doi.org/10.1016/j.ejso.2012.10.007.
Kulshrestha S, Bunn C, Patel PM, Sweigert PJ, Eguia E, Pawlik TM et al. Textbook oncologic outcome is associated with increased overall survival after esophagectomy. Surgery. 2020. doi:https://doi.org/10.1016/j.surg.2020.05.038.
Sweigert PJ, Eguia E, Baker MS, Link CM, Hyer JM, Paredes AZ et al. Assessment of Cancer Center Variation in Textbook Oncologic Outcomes Following Colectomy for Adenocarcinoma. J Gastrointest Surg. 2020. doi:https://doi.org/10.1007/s11605-020-04767-4.
Sweigert PJ, Eguia E, Baker MS, Paredes AZ, Tsilimigras DI, Dillhoff M et al. Assessment of textbook oncologic outcomes following pancreaticoduodenectomy for pancreatic adenocarcinoma. J Surg Oncol. 2020;121(6):936-44. doi:https://doi.org/10.1002/jso.25861.
Wexner SD, Berho ME. The Rationale for and Reality of the New National Accreditation Program for Rectal Cancer. Dis Colon Rectum. 2017;60(6):595-602. doi:https://doi.org/10.1097/DCR.0000000000000840.
Brady JT, Xu Z, Scarberry KB, Saad A, Fleming FJ, Remzi FH et al. Evaluating the Current Status of Rectal Cancer Care in the US: Where We Stand at the Start of the Commission on Cancer's National Accreditation Program for Rectal Cancer. J Am Coll Surg. 2018;226(5):881-90. doi:https://doi.org/10.1016/j.jamcollsurg.2018.01.057.
Bilimoria KY, Bentrem DJ, Ko CY, Ritchey J, Stewart AK, Winchester DP et al. Validation of the 6th edition AJCC Pancreatic Cancer Staging System: report from the National Cancer Database. Cancer. 2007;110(4):738–744. doi:https://doi.org/10.1002/cncr.22852.
Merkow RP, Rademaker AW, Bilimoria KY. Practical Guide to Surgical Data Sets: National Cancer Database (NCDB). JAMA Surg. 2018. doi:https://doi.org/10.1001/jamasurg.2018.0492.
Moris D, Cerullo M, Nussbaum DP, Blazer DG, 3rd. Textbook Outcomes Among Patients Undergoing Retroperitoneal Sarcoma Resection. Anticancer Res. 2020;40(4):2107-15. doi:https://doi.org/10.21873/anticanres.14169.
Merath K, Chen Q, Bagante F, Beal E, Akgul O, Dillhoff M et al. Textbook Outcomes Among Medicare Patients Undergoing Hepatopancreatic Surgery. Ann Surg. 2020;271(6):1116-23. doi:https://doi.org/10.1097/SLA.0000000000003105.
Sweigert PJ, Eguia E, Baker MS, Link CM, Hyer JM, Paredes AZ et al. Assessment of Cancer Center Variation in Textbook Oncologic Outcomes Following Colectomy for Adenocarcinoma. J Gastrointest Surg. 2021;25(3):775-85. doi:https://doi.org/10.1007/s11605-020-04767-4.
Marusch F, Koch A, Schmidt U, Pross M, Gastinger I, Lippert H. Hospital caseload and the results achieved in patients with rectal cancer. Br J Surg. 2001;88(10):1397-402. doi:https://doi.org/10.1046/j.0007-1323.2001.01873.x.
Rogers SO, Jr., Wolf RE, Zaslavsky AM, Wright WE, Ayanian JZ. Relation of surgeon and hospital volume to processes and outcomes of colorectal cancer surgery. Ann Surg. 2006;244(6):1003-11. doi:https://doi.org/10.1097/01.sla.0000231759.10432.a7.
van Gijn W, Gooiker GA, Wouters MW, Post PN, Tollenaar RA, van de Velde CJ. Volume and outcome in colorectal cancer surgery. Eur J Surg Oncol. 2010;36 Suppl 1:S55-63. doi:https://doi.org/10.1016/j.ejso.2010.06.027.
Damle RN, Macomber CW, Flahive JM, Davids JS, Sweeney WB, Sturrock PR et al. Surgeon volume and elective resection for colon cancer: an analysis of outcomes and use of laparoscopy. J Am Coll Surg. 2014;218(6):1223-30. doi:https://doi.org/10.1016/j.jamcollsurg.2014.01.057.
Koeter T, de Nes LCF, Wasowicz DK, Zimmerman DDE, Verhoeven RHA, Elferink MA et al. Hospital variation in sphincter-preservation rates in rectal cancer treatment: results of a population-based study in the Netherlands. BJS Open. 2021;5(4). doi:https://doi.org/10.1093/bjsopen/zrab065.
Rickles AS, Dietz DW, Chang GJ, Wexner SD, Berho ME, Remzi FH et al. High Rate of Positive Circumferential Resection Margins Following Rectal Cancer Surgery: A Call to Action. Ann Surg. 2015;262(6):891-8. doi:https://doi.org/10.1097/SLA.0000000000001391.
Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK et al. Rectal Cancer, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2018;16(7):874–901. doi:https://doi.org/10.6004/jnccn.2018.0061.
Bujko K, Glynne-Jones R, Bujko M. Does adjuvant fluoropyrimidine-based chemotherapy provide a benefit for patients with resected rectal cancer who have already received neoadjuvant radiochemotherapy? A systematic review of randomised trials. Ann Oncol. 2010;21(9):1743-50. doi:https://doi.org/10.1093/annonc/mdq054.
Valentini V, Aristei C, Glimelius B, Minsky BD, Beets-Tan R, Borras JM et al. Multidisciplinary Rectal Cancer Management: 2nd European Rectal Cancer Consensus Conference (EURECA-CC2). Radiother Oncol. 2009;92(2):148-63. doi:https://doi.org/10.1016/j.radonc.2009.06.027.
de Paula TR, Gorroochurn P, Kiran RP, Keller DS. Does Adjuvant Chemotherapy Improve Survival in T3N0 Rectal Cancer? An Evaluation of Use and Outcomes from the National Cancer Database (NCDB). J Gastrointest Surg. 2020;24(5):1188-91. doi:https://doi.org/10.1007/s11605-020-04541-6.
Breugom AJ, Swets M, Bosset JF, Collette L, Sainato A, Cionini L et al. Adjuvant chemotherapy after preoperative (chemo)radiotherapy and surgery for patients with rectal cancer: a systematic review and meta-analysis of individual patient data. Lancet Oncol. 2015;16(2):200-7. doi:https://doi.org/10.1016/S1470-2045(14)71199-4.
Biagi JJ, Raphael MJ, Mackillop WJ, Kong W, King WD, Booth CM. Association between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysis. JAMA. 2011;305(22):2335-42. doi:https://doi.org/10.1001/jama.2011.749.
Bosset JF, Calais G, Mineur L, Maingon P, Stojanovic-Rundic S, Bensadoun RJ et al. Fluorouracil-based adjuvant chemotherapy after preoperative chemoradiotherapy in rectal cancer: long-term results of the EORTC 22921 randomised study. Lancet Oncol. 2014;15(2):184-90. doi:https://doi.org/10.1016/S1470-2045(13)70599-0.
Glynne-Jones R, Counsell N, Quirke P, Mortensen N, Maraveyas A, Meadows HM et al. Chronicle: results of a randomised phase III trial in locally advanced rectal cancer after neoadjuvant chemoradiation randomising postoperative adjuvant capecitabine plus oxaliplatin (XELOX) versus control. Ann Oncol. 2014;25(7):1356-62. doi:https://doi.org/10.1093/annonc/mdu147.
Jimenez-Rodriguez RM, Rubio-Dorado-Manzanares M, Diaz-Pavon JM, Reyes-Diaz ML, Vazquez-Monchul JM, Garcia-Cabrera AM et al. Learning curve in robotic rectal cancer surgery: current state of affairs. Int J Colorectal Dis. 2016;31(12):1807-15. doi:https://doi.org/10.1007/s00384-016-2660-0.
Greenblatt DY, Rajamanickam V, Pugely AJ, Heise CP, Foley EF, Kennedy GD. Short-term outcomes after laparoscopic-assisted proctectomy for rectal cancer: results from the ACS NSQIP. J Am Coll Surg. 2011;212(5):844-54. doi:https://doi.org/10.1016/j.jamcollsurg.2011.01.005.
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. 2008(2):CD003432. doi:https://doi.org/10.1002/14651858.CD003432.pub2.
Sujatha-Bhaskar S, Jafari MD, Gahagan JV, Inaba CS, Koh CY, Mills SD et al. Defining the Role of Minimally Invasive Proctectomy for Locally Advanced Rectal Adenocarcinoma. Ann Surg. 2017;266(4):574-81. doi:https://doi.org/10.1097/SLA.0000000000002357.
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES et al. A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med. 2015;372(14):1324-32. doi:https://doi.org/10.1056/NEJMoa1414882.
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA et al. Disease-free Survival and Local Recurrence for Laparoscopic Resection Compared With Open Resection of Stage II to III Rectal Cancer: Follow-up Results of the ACOSOG Z6051 Randomized Controlled Trial. Ann Surg. 2019;269(4):589-95. doi:https://doi.org/10.1097/SLA.0000000000003002.
Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD et al. Disease-free Survival and Local Recurrence After Laparoscopic-assisted Resection or Open Resection for Rectal Cancer: The Australasian Laparoscopic Cancer of the Rectum Randomized Clinical Trial. Ann Surg. 2019;269(4):596-602. doi:https://doi.org/10.1097/SLA.0000000000003021.
Chioreso C, Del Vecchio N, Schweizer ML, Schlichting J, Gribovskaja-Rupp I, Charlton ME. Association Between Hospital and Surgeon Volume and Rectal Cancer Surgery Outcomes in Patients With Rectal Cancer Treated Since 2000: Systematic Literature Review and Meta-analysis. Dis Colon Rectum. 2018;61(11):1320-32. doi:https://doi.org/10.1097/DCR.0000000000001198.
Abbas MA, Chang GJ, Read TE, Rothenberger DA, Garcia-Aguilar J, Peters W et al. Optimizing rectal cancer management: analysis of current evidence. Dis Colon Rectum. 2014;57(2):252-9. doi:https://doi.org/10.1097/DCR.0000000000000020.
Morris AM, Wei Y, Birkmeyer NJ, Birkmeyer JD. Racial disparities in late survival after rectal cancer surgery. J Am Coll Surg. 2006;203(6):787-94. doi:https://doi.org/10.1016/j.jamcollsurg.2006.08.005.
Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL. Racial and Ethnic Disparities in Cancer Survival: The Contribution of Tumor, Sociodemographic, Institutional, and Neighborhood Characteristics. J Clin Oncol. 2018;36(1):25-33. doi:https://doi.org/10.1200/JCO.2017.74.2049.
Lee DY, Teng A, Pedersen RC, Tavangari FR, Attaluri V, McLemore EC et al. Racial and Socioeconomic Treatment Disparities in Adolescents and Young Adults with Stage II-III Rectal Cancer. Ann Surg Oncol. 2017;24(2):311-8. doi:https://doi.org/10.1245/s10434-016-5626-0.
Fields AC, Lu PW, Yoo J, Irani J, Goldberg JE, Bleday R et al. Treatment of stage I-III rectal cancer: Who is refusing surgery? J Surg Oncol. 2020;121(6):990-1000. doi:https://doi.org/10.1002/jso.25873.
Author information
Authors and Affiliations
Contributions
Study concepts: FD, SN.
Study design: SN, FD, SK.
Manuscript preparation: FD, SN.
Data acquisition: SN, FD.
Quality control of data algorithm: SK, GS, BW, MA.
Manuscript review: SN, FD, SK, GS.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Synopsis
Textbook outcomes of rectal adenocarcinoma in NCDB are achieved uncommonly. MIS and volume are modifiable factors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Naffouje, S.A., Ali, M.A., Kamarajah, S.K. et al. Assessment of Textbook Oncologic Outcomes Following Proctectomy for Rectal Cancer. J Gastrointest Surg 26, 1286–1297 (2022). https://doi.org/10.1007/s11605-021-05213-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05213-9