Abstract
Background
The prognostic impact of HER2-low on overall survival (OS) and disease-free survival (DFS) in patients with resectable breast cancer (BC) remains controversial, partly resulting from the hormone receptor (HR) status.
Objective
To investigate the prognostic impact of HER2-low in different HR subgroups.
Patients and Methods
We retrospectively retrieved medical records of treatment-naive primary HER2-low and HER2-zero BC patients who were diagnosed with invasive ductal carcinoma and underwent surgery in the Cancer Hospital of the Chinese Academy of Medical Sciences from January 2009 to September 2017 (n = 7371). We compared the clinicopathologic features and performed Cox regression and landmark survival analyses to explore the prognostic impact of HER2-low on survival outcomes during distinct post-surgery intervals—36 months, 60 months, and 120 months.
Results
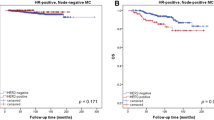
HER2-low BC, compared to HER2-zero BC, exhibited less aggressive clinicopathologic features, such as smaller invasion size, lower grade, increased nerve invasion, higher HR positivity, and a higher proportion of low-Ki67 cases. In the HR-positive subgroup, HER2-low demonstrated improved OS (p = 0.046) and DFS (p = 0.026) within 60 months. Conversely, HER2-low displayed worse DFS (p = 0.046) in the HR-negative subgroup after 36 months from surgery. The findings remained robust in uni- and multi-variable Cox models.
Conclusions
HER2-low BCs manifested less aggressive clinicopathologic features than the HER2-zero cases. The prognostic impact of HER2-low in resectable BCs exhibits variability contingent upon the patients’ HR status.





Similar content being viewed by others
Reference
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–49.
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32.
Howlader N, Cronin KA, Kurian AW, Andridge R. Differences in breast cancer survival by molecular subtypes in the United States. Cancer Epidemiol Biomark Prev. 2018;27:619–26.
Yu K, Lee CH, Tan PH, Tan P. Conservation of breast cancer molecular subtypes and transcriptional patterns of tumor progression across distinct ethnic populations. Clin Cancer Res. 2004;10:5508–17.
Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LAG, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106:dju055.
Paquet ER, Hallett MT. Absolute assignment of breast cancer intrinsic molecular subtype. J Natl Cancer Inst. 2015;107:357.
Mullan PB, Millikan RC. Molecular subtyping of breast cancer: opportunities for new therapeutic approaches. Cell Mol Life Sci. 2007;64:3219–32.
Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N Engl J Med. 2020;382:597–609.
Swain SM, Miles D, Kim S-B, Im Y-H, Im S-A, Semiglazov V, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. Lancet Oncol. 2020;21:519–30.
Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367:1783–91.
Modi S, Saura C, Yamashita T, Park YH, Kim S-B, Tamura K, et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2020;382:610–21.
Fan P, Xu K. Antibody-drug conjugates in breast cancer: marching from HER2-overexpression into HER2-low. Biochim Biophys Acta Rev Cancer. 2023;1878: 188849.
Yaghoobi V, Martinez-Morilla S, Liu Y, Charette L, Rimm DL, Harigopal M. Advances in quantitative immunohistochemistry and their contribution to breast cancer. Expert Rev Mol Diagn. 2020;20:509–22.
Rakha EA, Tan PH. Immunohistochemistry in Breast Cancer: Practice Points and Pitfalls. Pathobiol J Immunopathol Mol Cell Biol. 2022;89:261–2.
Vuong D, Simpson PT, Green B, Cummings MC, Lakhani SR. Molecular classification of breast cancer. Virchows Arch Int J Pathol. 2014;465:1–14.
Allred DC, Carlson RW, Berry DA, Burstein HJ, Edge SB, Goldstein LJ, et al. NCCN task force report: estrogen receptor and progesterone receptor testing in breast cancer by immunohistochemistry. J Natl Compr Cancer Netw JNCCN. 2009;7(Suppl 6):S1–21.
Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387:9–20.
Modi S, Park H, Murthy RK, Iwata H, Tamura K, Tsurutani J, et al. antitumor activity and safety of trastuzumab deruxtecan in patients with HER2-low-expressing advanced breast cancer: results from a phase Ib study. J Clin Oncol. 2020;38:1887–96.
Mutai R, Barkan T, Moore A, Sarfaty M, Shochat T, Yerushalmi R, et al. Prognostic impact of HER2-low expression in hormone receptor positive early breast cancer. Breast. 2021;60:62–9.
Denkert C, Seither F, Schneeweiss A, Link T, Blohmer J-U, Just M, et al. Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol. 2021;22:1151–61.
Yang M, Sun J, Liu L, Kong X, Lin D, Zhou H, et al. Clinicopathological characteristics of HER2-low breast cancer: a retrospective study. Sci Rep. 2023;13:12382.
Zheng L, Zhang Y, Wang Z, Wang H, Hao C, Li C, et al. Comparisons of clinical characteristics, prognosis, epidemiological factors, and genetic susceptibility between HER2-low and HER2-zero breast cancer among Chinese females. Cancer Med. 2023;12(14):14937–48.
Schettini F, Chic N, Brasó-Maristany F, Paré L, Pascual T, Conte B, et al. Clinical, pathological, and PAM50 gene expression features of HER2-low breast cancer. NPJ Breast Cancer. 2021;7:1.
Horisawa N, Adachi Y, Takatsuka D, Nozawa K, Endo Y, Ozaki Y, et al. The frequency of low HER2 expression in breast cancer and a comparison of prognosis between patients with HER2-low and HER2-negative breast cancer by HR status. Breast Cancer. 2022;29:234–41.
Tarantino P, Jin Q, Tayob N, Jeselsohn RM, Schnitt SJ, Vincuilla J, et al. Prognostic and biologic significance of ERBB2-low expression in early-stage breast cancer. JAMA Oncol. 2022;8:1177–83.
Guven DC, Kaya MB, Fedai B, Ozden M, Yildirim HC, Kosemehmetoglu K, et al. HER2-low breast cancer could be associated with an increased risk of brain metastasis. Int J Clin Oncol. 2022;27:332–9.
Li J-J, Yu Y, Ge J. HER2-low-positive and response to NACT and prognosis in HER2-negative non-metastatic BC. Breast Cancer. 2023;30:364–78.
Schalper KA, Kumar S, Hui P, Rimm DL, Gershkovich P. A retrospective population-based comparison of HER2 immunohistochemistry and fluorescence in situ hybridization in breast carcinomas: impact of 2007 American Society of Clinical Oncology/College of American Pathologists criteria. Arch Pathol Lab Med. 2014;138:213–9.
Almstedt K, Heimes A-S, Kappenberg F, Battista MJ, Lehr H-A, Krajnak S, et al. Long-term prognostic significance of HER2-low and HER2-zero in node-negative breast cancer. Eur J Cancer. 2022;173:10–9.
Li Y, Abudureheiyimu N, Mo H, Guan X, Lin S, Wang Z, et al. In real life, low-level HER2 Expression may be associated with better outcome in HER2-negative breast cancer: a study of the National Cancer Center. China Front Oncol. 2021;11: 774577.
Wolff AC, Hammond MEH, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013.
McNamara MG, Lopes A, Wasan H, Malka D, Goldstein D, Shannon J, et al. Landmark survival analysis and impact of anatomic site of origin in prospective clinical trials of biliary tract cancer. J Hepatol. 2020;73:1109–17.
de Boniface J, Szulkin R, Johansson ALV. Survival after breast conservation vs mastectomy adjusted for comorbidity and socioeconomic status: a Swedish National 6-year follow-up of 48 986 women. JAMA Surg. 2021;156:628–37.
Xin L, Wu Q, Zhan C, Qin H, Xiang H, Xu L, et al. Multicenter study of the clinicopathological features and recurrence risk prediction model of early-stage breast cancer with low-positive human epidermal growth factor receptor 2 expression in China (Chinese Society of Breast Surgery 021). Chin Med J (Engl). 2022;135:697–706.
Won HS, Ahn J, Kim Y, Kim JS, Song J-Y, Kim H-K, et al. Clinical significance of HER2-low expression in early breast cancer: a nationwide study from the Korean Breast Cancer Society. Breast Cancer Res. 2022;24:22.
Yang C, Zhang X, Chen Y, Li P, Zhang J, Xu A, et al. Survival differences between HER2-0 and HER2-low-expressing breast cancer—a meta-analysis of early breast cancer patients. Crit Rev Oncol Hematol. 2023;185: 103962.
Ergun Y, Ucar G, Akagunduz B. Comparison of HER2-zero and HER2-low in terms of clinicopathological factors and survival in early-stage breast cancer: a systematic review and meta-analysis. Cancer Treat Rev. 2023;115: 102538.
Liu C-G, Li Y-F, Ma T-Y, Lv M, Lv Z-D, Wang Y-Y, et al. Clinicopathological characteristics and prognosis of early-stage HER2 low-expression breast cancer: a single-center retrospective study. Front Oncol. 2023;13:1130734.
Xu H, Han Y, Wu Y, Wang Y, Li Q, Zhang P, et al. Clinicopathological characteristics and prognosis of HER2-low early-stage breast cancer: a single-institution experience. Front Oncol. 2022;12: 906011.
Peiffer DS, Zhao F, Chen N, Hahn OM, Nanda R, Olopade OI, et al. Clinicopathologic characteristics and prognosis of ERBB2-Low breast cancer among patients in the national cancer database. JAMA Oncol. 2023;9:500–10.
Fernandez AI, Liu M, Bellizzi A, Brock J, Fadare O, Hanley K, et al. Examination of low ERBB2 protein expression in breast cancer tissue. JAMA Oncol. 2022;8:1–4.
Rüschoff J, Friedrich M, Nagelmeier I, Kirchner M, Andresen LM, Salomon K, et al. Comparison of HercepTestTM mAb pharmDx (Dako Omnis, GE001) with Ventana PATHWAY anti-HER-2/neu (4B5) in breast cancer: correlation with HER2 amplification and HER2 low status. Virchows Arch Int J Pathol. 2022;481:685–94.
Robbins CJ, Fernandez AI, Han G, Wong S, Harigopal M, Podoll M, et al. Multi-institutional Assessment of Pathologist Scoring HER2 Immunohistochemistry. Mod Pathol. 2023;36: 100032.
Mayr D, Heim S, Werhan C, Zeindl-Eberhart E, Kirchner T. Comprehensive immunohistochemical analysis of Her-2/neu oncoprotein overexpression in breast cancer: HercepTest (Dako) for manual testing and Her-2/neuTest 4B5 (Ventana) for Ventana BenchMark automatic staining system with correlation to results of fluorescence in situ hybridization (FISH). Virchows Arch Int J Pathol. 2009;454:241–8.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was funded by the CAMS Innovation Fund for Medical Sciences (CIFMS, ID Number: 2021-I2M-1-014) and the Beijing Hope Run Special Fund of Cancer Foundation of China (ID Number: LC2022A02).
Competing Interests
Qichen Dai, Kexin Feng, Gang Liu, Han Cheng, Xiangyu Tong, Xiang Wang, Lin Feng, and Yipeng Wang declare they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics Approval & Consent to Participate
This study was constructed as a retrospective design, obtaining data from previous medical records. Our study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline and obtained a waiver of informed consent due to the retrospective design. This study was approved by the National GCP Center for Anticancer Drugs, The Independent Ethics Committee (Approval Number: 23/350-4092).
Consent for Publication
Not applicable.
Availability of Data and Material
The datasets generated during and/or analyzed during the current study are not publicly available due to the confidentiality regulations concerning patient personal information by our institutional ethics committee but are available in an anonymized form from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author’s Contributions
XW, LF and YW contributed to the conception, supervision, and funding of the study. QD, KF and GL carried out the data retrieval, collection, and analyses. QD wrote the original draft. HC and XT were responsible for the critical revision of the manuscript or important intellectual content. GL managed the resources and interpretation. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dai, Q., Feng, K., Liu, G. et al. Prognostic Impact of HER2-Low and HER2-Zero in Resectable Breast Cancer with Different Hormone Receptor Status: A Landmark Analysis of Real-World Data from the National Cancer Center of China. Targ Oncol 19, 81–93 (2024). https://doi.org/10.1007/s11523-023-01030-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-023-01030-z