Abstract
Introduction
Sleep-disordered breathing (SDB) in primary school children is a significant problem, yet its prevalence is not well known outside large urban settings. Information on the burden and risk factors of SDB in children could be used to improve resource allocation when providing care across a large country. The objectives of this study were to assess the prevalence of SDB among school-aged children comparing rural and urban settings, and to investigate associated risk factors.
Methods
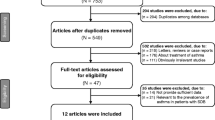
In this cross-sectional study, a random sample of primary school students in Turkey were selected from urban and rural areas and data were collected using the Pediatric Sleep Questionnaire, asthma, and allergic rhinitis questionnaires completed by the parents.
Results
Questionnaires were collected from a total of 139 schools from 58 provinces. A total of 11,013 students were contacted, and 9045 (73%) completed the study. There was no difference in the prevalence of SDB between rural and urban settings (16% vs. 15%, p = 0.612). Multivariate logistic regression analysis revealed that current wheezing, current rhinoconjunctivitis, being overweight, parental snoring, and current mold at home were significant risk factors for SDB in both rural and urban children. Current tobacco smoke exposure (OR = 1.48, 95%CI = 1.19–1.85), near roadway air pollution exposure (OR = 1.40, 95%CI = 1.108–1.791), and mold at home in the first year of life (OR = 1.68, 95%CI = 1.26–2.23) were associated with SDB in urban children. History of maternal/paternal adenotonsillectomy was a significant predictor of SDB in the rural setting (OR = 1.63, 95%CI = 1.12–2.39).
Conclusion
The prevalence of SDB is high in children living in both settings but associated risk factors may vary. Children residing in rural areas should also be screened for sleep-disordered breathing during routine health visits.

Similar content being viewed by others
References
Kaditis AG, Alonso Alvarez ML, Boudewyns A, Alexopoulos EI, Ersu R, Joosten K, Larramona H, Miano S, Narang I, Trang H, Tsaoussoglou M, Vandenbussche N, Villa MP, van Waardenburg D, Weber S, Verhulst S (2016) Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J 47(1):69–94. https://doi.org/10.1183/13993003.00385-2015
Gozal D, Kheirandish-Gozal L (2008) The multiple challenges of obstructive sleep apnea in children: morbidity and treatment. Curr Opin Pediatr 20(6):654–658. https://doi.org/10.1097/MOP.0b013e328316ec2d
Li AM, Sadeh A, Au CT, Goh DY, Mindell JA (2013) Prevalence of habitual snoring and its correlates in young children across the Asia Pacific. J Paediatr Child Health 49(2):E153–E159. https://doi.org/10.1111/jpc.12083
Ersu R, Arman AR, Save D, Karadag B, Karakoc F, Berkem M, Dagli E (2004) Prevalence of snoring and symptoms of sleep-disordered breathing in primary school children in Istanbul. Chest 126(1):19–24. https://doi.org/10.1378/chest.126.1.19
Ng DK, Kwok KL, Cheung JM, Leung SY, Chow PY, Wong WH, Chan CH, Ho JC (2005) Prevalence of sleep problems in Hong Kong primary school children: a community-based telephone survey. Chest 128(3):1315–1323. https://doi.org/10.1378/chest.128.3.1315
Petry C, Pereira MU, Pitrez PM, Jones MH, Stein RT (2008) The prevalence of symptoms of sleep-disordered breathing in Brazilian schoolchildren. J Pediatr 84(2):123–129. https://doi.org/10.2223/JPED.1770
Guo Y, Pan Z, Gao F, Wang Q, Pan S, Xu S, Hui Y, Li L, Qian L (2020) Characteristics and risk factors of children with sleep-disordered breathing in Wuxi, China. BMC Pediatrics 20(1):310. https://doi.org/10.1186/s12887-020-02207-5
Paduano S, Paduano FP, Aiello D, Barbara L, Zampogna S, Pujia R, Malara C, Cantile T, Ferrazzano GF (2019) OSAS in developing age: screening of a southern Italy population. Eur J Paediatr Dent 20(4):302–305. https://doi.org/10.23804/ejpd.2019.20.04.08
Boss EF, Smith DF, Ishman SL (2011) Racial/ethnic and socioeconomic disparities in the diagnosis and treatment of sleep-disordered breathing in children. Int J Pediatr Otorhinolaryngol 75(3):299–307. https://doi.org/10.1016/j.ijporl.2010.11.006
Kheirandish-Gozal L, Ghalebandi M, Salehi M, Salarifar MH, Gozal D (2014) Neighbourhood air quality and snoring in school-aged children. Eur Respir J 43(3):824–832. https://doi.org/10.1183/09031936.00113113
Braido F, Baiardini I, Lacedonia D, Facchini FM, Fanfulla F, Molinengo G, Canonica GW (2014) Italian Society of Respiratory Medicine (SIMeR). Sleep apnea risk in subjects with asthma with or without comorbid rhinitis. Respir Care 59(12):1851–1856. https://doi.org/10.4187/respcare.03084
Liu J, Wei C, Huang L, Wang W, Liang D, Lei Z, Wang F, Wang X, Hou X, Tang X (2014) Prevalence of signs and symptoms suggestive of obstructive sleep apnea syndrome in Guangxi, China. Sleep Breath 18(2):375–382. https://doi.org/10.1007/s11325-013-0896-2
Fagnano M, van Wijngaarden E, Connolly HV, Carno MA, Forbes-Jones E, Halterman JS (2009) Sleep-disordered breathing and behaviors of inner-city children with asthma. Pediatrics. 124(1):218–225. https://doi.org/10.1542/peds.2008-2525
Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, Schechter MS, Ward SD, Sheldon SH, Shiffman RN et al (2012) American Academy of Pediatrics. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 130(3):e714–e755. https://doi.org/10.1542/peds.2012-1671
Gokdemir Y, Ersu R (2016) Sleep disordered breathing in childhood. Eur Respir Rev 25(139):48–53. https://doi.org/10.1183/16000617.0081-2015
Yang QZ, Bu YQ, Dong SY, Fan SS, Wang LX (2009) Comparison of sleeping problems in school-age children between rural and urban communities in China. J Paediatr Child Health 45(7–8):414–418. https://doi.org/10.1111/j.1440-1754.2009.01530.x
Chervin RD, Hedger K, Dillon JE, Pituch KJ (2000) Validity and reliability of scales for sleep disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med 1(1):21–32. https://doi.org/10.1016/s1389-9457(99)00009-x
Schaeffer RL, Mendenhall W, Ott L (1990) Elementary survey sampling, fourth edition. Duxbury Press, Belmont. https://doi.org/10.1016/s1389-9457(99)00009-x
Aydinli HI, Ciftci S (2015) The changing rural-urban concepts and the legislation’s effects on the nature in Turkey [Turkish]. Electronic Journal of Social Sciences ISSN:1304–0278 14(54):192–200
Yüksel H, Söğüt A, Yılmaz O, Kutluay E (2011) Reliability and validity of the Turkish version of the pediatric sleep questionnaire: a tool for prediction of sleep related breathing disorder. Tuberk Toraks 59(3):236–241. https://doi.org/10.5578/tt.2467
Steering Committee ISAAC (1998) Phase II modules of the International Study of Asthma and Allergies in Childhood (ISAAC). Institute of Epidemiology and Social Medicine, University of Muenster, Muenster
Saraçlar Y, Kuyucu S, Tuncer A, Sekerel B, Saçkesen C, Kocaba C (2003) Prevalence of asthmatic phenotypes and bronchial hyperresponsiveness in Turkish schoolchildren: an International Study of Asthma and Allergies in Childhood (ISAAC) phase 2 study. Ann Allergy Asthma Immunol 91:477–484. https://doi.org/10.1016/S1081-1206(10)61517-7
ISAAC (2009) Home page. Available: http://isaac.auckland.ac.nz/ [accessed 20 Sept 2009]
Kalaycıoğlu S, Kardam F, Tüzün S, Ulusoy M (1998) Türkiye İçin Bir Sosyoekonomik Statü Geliştirme¸ Yönünde Yaklaşım ve Denemeler. Toplum ve Hekim 13:126–137 (Turkish)
Chervin RD, Weatherly RA, Garetz SL, Ruzicka DL, Giordani BJ, Hodges EK, Dillon JE, Guire KE (2007) Pediatric sleep questionnaire: prediction of sleep apnea and outcomes. Arch Otolaryngol Head Neck Surg 133(3):216–222. https://doi.org/10.1001/archotol.133.3.216
Mitchell RB, Garetz S, Moore RH, Rosen CL, Marcus CL, Katz ES, Arens R, Chervin RD, Paruthi S, Amin R, Elden L, Ellenberg SS, Redline S (2015) The use of clinical parameters to predict obstructive sleep apnea syndrome severity in children: the Childhood Adenotonsillectomy (CHAT) study randomized clinical trial. JAMA Otolaryngol Head Neck Surg 141(2):130–136. https://doi.org/10.1001/jamaoto.2014.3049
Harding R, Haszard JJ, Schaughency E, Drummond B, Galland B (2020) Parent report of children’s sleep disordered breathing symptoms and limited academic progress in reading, writing, and math. Sleep Med 65:105–112. https://doi.org/10.1016/j.sleep.2019.07.018
Bhattacharjee R, Kim J, Kheirandish-Gozal L, Gozal D (2011) Obesity and obstructive sleep apnea syndrome in children: a tale of inflammatory cascades. Pediatr Pulmonol 46(4):313–323. https://doi.org/10.1002/ppul.21370
Kannan JA, Brokamp C, Bernstein DI, LeMasters GK, Hershey GKK, Villareal MS, Lockey JE, Ryan PH (2017) Parental snoring and environmental pollutants, but not aeroallergen sensitization, are associated with childhood snoring in a birth cohort. Pediatr Allergy Immunol Pulmonol 30(1):31–38. https://doi.org/10.1089/ped.2016.0681
Rogers VE, Bollinger ME, Tulapurkar ME, Zhu S, Hasday JD, Pereira KD, Scharf SM (2018) Inflammatio and asthma control in children with comorbid obstructive sleep apnea. Pediatr Pulmonol 53(9):1200–1207. https://doi.org/10.1002/ppul.24074
Doganer YC, Rohrer JE, Aydogan U, Thurston MJ, Saglam K (2015) Tonsillectomy, adenoidectomy and adenotonsillectomy rates in school-aged children: relative contributions of socio-demographic and clinical features. Int J Pediatr Otorhinolaryngol 79(7):969–974. https://doi.org/10.1016/j.ijporl.2015.03.005
Özkırış M, Kapusuz Z, Saydam L (2013) The frequency of adenotonsillectomies in relation to socioeconomic status among primary school students in Yozgat province. Turk J Pediatr 55:74–77
Polat C, Demiroren K (2010) Frequency of the tonsillectomy and adenoidectomy in children in Elazig province, in the east of Turkey. Dicle Medical Journal 37(3):263–266
Sun K, Zhang Y, Tian Y, Jiang X (2018) Environmental tobacco smoke exposure and risk of habitual snoring in children: a meta-analysis. J Epidemiol Community Health 72(11):1064–1070. https://doi.org/10.1136/jech-2018-210820
Castro-Rodriguez JA, Brockmann PE, Marcus CL (2017) Relation between asthma and sleep disordered breathing in children: is the association causal? Paediatr Respir Rev 22:72–75. https://doi.org/10.1016/j.prrv.2016.08.010
Mitchell EA, Beasley R, Keil U, Montefort S, Odhiambo J, ISAAC Phase Three Study Group (2012) The association between tobacco and the risk of asthma, rhinoconjunctivitis and eczema in children and adolescents: analyses from phase three of the ISAAC programme. Thorax 67(11):941–949. https://doi.org/10.1136/thoraxjnl-2011-200901
Tsaoussoglou M, Lianou L, Maragozidis P, Hatzinikolaou S, Mavromati M, Orologas N, Panaghiotopoulou-Gartagani P, Rassidakis G, Balatsos NA, Chrousos G, Kaditis AG (2012) Cysteinyl leukotriene receptors in tonsillar B- and T-lymphocytes from children with obstructive sleep apnea. Sleep Med 13(7):879–885. https://doi.org/10.1016/j.sleep.2012.03.010
Gislason T, Bertelsen RJ, Real FG, Sigsgaard T, Franklin KA, Lindberg E, Janson C, Arnardottir ES, Hellgren J, Benediktsdottir B, Forsberg B, Johannessen A (2016) Self-reported exposure to traffic pollution in relation to daytime sleepiness and habitual snoring: a questionnaire study in seven North-European cities. Sleep Med 24:93–99. https://doi.org/10.1016/j.sleep.2016.08.007
Zanobetti A, Redline S, Schwartz J, Rosen D, Patel S, O’Connor GT, Lebowitz M, Coull BA, Gold DR (2016) Associations of PM10 with sleep and sleep-disordered breathing in adults from seven U.S. urban areas. Am J Respir Crit Care Med 18(6):819–825. https://doi.org/10.1016/j.sleep.2012.01.014
Brockmann PE, Bertrand P, Castro-Rodriguez JA (2014) Influence of asthma on sleep disordered breathing in children: a systematic review. Sleep Med Rev 18:393–397. https://doi.org/10.1016/j.smrv.2014.01.005
Wan GH, Li CS (1999) Indoor endotoxin and glucan in association with airway inflammation and systemic symptoms. Arch Environ Health 54:172–179. https://doi.org/10.1080/00039899909602256
Tiesler CM, Thiering E, Tischer C, Lehmann I, Schaaf B, von Berg A, Heinrich J (2015) Exposure to visible mold or dampness at home and sleep problems in children: results from the LISAplus study. Environ Res 137:357–363. https://doi.org/10.1016/j.envres.2014.11.023
Alexopoulos EI, Charitos G, Malakasioti G, Varlami V, Gourgoulianis K, Zintzaras E, Kaditis AG (2014) Parental history of adenotonsillectomy is associated with obstructive sleep apnea severity in children with snoring. J Pediatr 164(6):1352–1357. https://doi.org/10.1016/j.jpeds.2014.01.021
Lundkvist K, Sundquist K, Li X, Friberg D (2012) Familial risk of sleep-disordered breathing. Sleep Med 13(6):668–673. https://doi.org/10.1016/j.sleep.2012.01.014
Acknowledgments
This study was developed as an American Thoracic Society MECOR (Methods in Epidemiologic, Clinical, and Operations Research) TURKEY project.
Funding
This study was funded by research grants from the Turkish Thoracic Society and Turkish Ministry of Health. The study was granted by TUBITAK 1507 R&D projects. Grant number: 7121045.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gokdemir, Y., Civelek, E., Cakir, B. et al. Prevalence of sleep-disordered breathing and associated risk factors in primary school children in urban and rural environments. Sleep Breath 25, 915–922 (2021). https://doi.org/10.1007/s11325-020-02206-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02206-x