Abstract
Background
Sleep-disordered breathing (SDB) may lead to poor asthma control in children.
Objective
To identify risk factors of SDB in children with asthma and assess its impact on asthma control.
Methods
In this cross-sectional study, we collected data of outpatients with asthma at the Children’s Hospital of Chongqing Medical University from June 2020 to August 2021. The Pediatric Sleep Questionnaire—Sleep-Related Breathing Disorder and the age-appropriate asthma control tests Childhood Asthma Control Test and Test for Respiratory and Asthma Control in Kids were completed.
Results
We enrolled 397 children with a male-to-female ratio of 1.7:1 and a mean age of 5.70 ± 2.53 years. The prevalence of SDB was 21.6%. Allergic rhinitis (odds ratio OR = 3.316), chronic tonsillitis (OR = 2.246), gastroesophageal reflux (OR = 7.518), adenoid hypertrophy (OR = 3.479), recurrent respiratory infections (OR = 2.195), and a family history of snoring (OR = 2.048) were risk factors for the development of combined SDB in children with asthma (p < 0.05). Asthma was poorly controlled in 19.6% of the children. SDB (OR = 2.391) and irregular medication use (OR = 2.571) were risk factors for poor asthma control (p < 0.05).
Conclusions
Allergic rhinitis, chronic tonsillitis, gastroesophageal reflux, adenoid hypertrophy, recurrent respiratory infections, and a family history of snoring were independent risk factors for the development of SDB in children with asthma. SDB and irregular medication use were independent risk factors for poor asthma control.
Similar content being viewed by others
Introduction
Asthma is a common lower airway respiratory disease, characterized by chronic airway inflammation and hyperresponsiveness. The prevalence of asthma has increased by over 50% every decade in China [1,2,3]. Approximately 4.2% of the population over 4 years of age suffers from asthma. Despite evidence-based assessment and treatment guidelines, asthma is not well-controlled in over 20% of children [4], posing an enormous economic and mental health burden on children and their caregivers. Further, poorly controlled asthma is a leading cause of emergency treatment, hospitalization, and death of children.
Sleep disordered breathing ( SDB ) is a series of diseases that interfere with normal ventilation and sleep structure, including central sleep apnea syndrome, obstructive sleep apnea syndrome (OSAS), sleep-related hypopnea disorder, etc. Its clinical manifestations are snoring, apnea, mouth breathing, sleep insecurity, daytime sleepiness, and inattentive concentration. The incidence of primary snoring was 1.5–27.6% [5]. The incidence of OSAS was 1.2–5.7% [6]. The most common cause of SDB in children is adenoid tonsillar hypertrophy, which can be treated by adenotonsillectomy [7].
SDB and asthma are upper and lower airway inflammatory diseases, respectively. According to the united airway disease hypothesis [8], upper and lower airway inflammations often co-exist, and upper airway disease may influence the severity and clinical control of lower airway disease. Thus, SDB is a risk factor for asthma [9,10,11,12]. In addition, adenotonsillectomy can improve asthma symptoms [13,14,15]. Although risk factors of SDB in children with asthma have been explored, studies are warranted on combined SDB and other risk factors in children with poorly controlled asthma to help achieve asthma control.
The aim of this study was to determine the correlation between SDB and asthma control level and asthma severity, and analyze the risk factors of asthma combined with SDB in order to identify co affected children earlier and provide more clinical treatment strategies for poorly controlled asthma.
Materials and methods
Study subjects
Children aged 0–18 years with asthma were enrolled from June 2020 to August 2021 from the asthma outpatient clinic at the Children’s Hospital of Chongqing Medical University, which is the third-largest children’s hospital in China and mainly serves children in southwest China. Inclusion criteria were: (1) a diagnosis of asthma based on the criteria from the Global Initiative for Asthma (GINA), 2020; and (2) a follow-up duration > 1 month. Exclusion criteria were: (1) a history of chronic lung disease, such as bronchiectasis; (2) a history of adenoidectomy or tonsillectomy; (3) presence of other chronic underlying diseases (e.g., heart disease; chronic lung disease in preterm infants; cerebral palsy; neuromuscular disease; genetic metabolic diseases, such as diabetes mellitus; glycogen accumulation disease; chromosomal disorders, such as trisomy 21 syndrome); (4) presence of craniofacial anomalies; and (5) incomplete questionnaires.
Data collection
The patients or their guardians completed the Pediatric Sleep Questionnaire—Sleep-Related Breathing Disorder (PSQ-SRBD). The patients underwent an age-appropriate asthma control test and the pulmonary function test if they were able to perform. The patients’ demographic characteristics, medical history (including concomitant atopic diseases), physical findings, PSQ-SRBD findings, asthma control test results, and allergic history were collected.
Research methodology
Anthropometric indicators
Trained technicians measured the patients’ height and weight using standardized protocols and calibrated equipment. According to the standardized growth values and curves for the body weight for length and body mass index (BMI) of Chinese children < 7 years of age [16], “obese” was defined as a body weight for length > P97 in children < 2 years of age and BMI > P95 in children ≥ 2 years of age.
Spirometry
The pulmonary function test was performed for children who could undergo it, using the MasterScreen Paed spirometer (Jaeger, Germany). The test’s operation, quality control, and determination of results (nature, type, and severity of disease) followed the Guidelines for Children’s Pulmonary Function Series (II): Lung Volume and Ventilatory Function [17]. The children stood upright, and a nasal clip was used. They completed the respiratory maneuvers under the technician’s guidance 3–8 times. The best performance value was regarded as the test result.
Skin prick test
An allergen skin prick solution (Beijing Xinhua Macro-Union Pharmaceutical Ltd. Corp.) was used to detect inhaled allergens, including house dust mites, dust mites, cat feathers, dog feathers, cotton wool, cockroach, birch pollen, corn pollen, cigarette smoke, Artemisia vulgaris, yeasts, penicillium, and edible allergens, including peanut, milk, egg, mango, apple, soybean, scallop, beef, shrimp, and crab. Histamine and saline were used as positive and negative controls, respectively. A wheal diameter ≥ 3 mm was considered as a positive reaction [18].
PSQ-SRBD
The PSQ is a screening questionnaire recommended by the American Academy of Pediatrics in the 2012 OSAS guidelines [6]. It is a valid, reliable, convenient, and feasible questionnaire covering sleep snoring, sleepiness, and hyperactivity [7, 19]. A PSQ-SRBD score > 0.33 suggests a high risk of SDB. The study subjects were divided into SDB-positive (score > 0.33) and SDB-negative (score ≤ 0.33) groups.
Asthma control in children
The Childhood Asthma Control Test (c-ACT) is a questionnaire recommended for children ≥ 4 years of age by GINA to assess asthma control in the past 4 weeks [20, 21]. The Test for Respiratory and Asthma Control in Kids (TRACK) is an assessment tool for asthma control in children < 5 years of age that was developed by American scholars in 2007 and modified for international use [22].
In this study, the official Chinese versions of TRACK and c-ACT were used for children < 4 and ≥ 4 years of age, respectively. The children and their guardians answered the questions in their respective sections separately, and the sum of scores was used for analyses. Well- and poorly controlled asthma groups were defined as a TRACK score ≥ 80 or c-ACT score ≥ 20 and a TRACK score < 80 or c-ACT score < 20, respectively.
Irregular medication use
In this study, Irregular medication use refers to poor medication adherence and incorrect inhalation methods, such as a lack of a suitable fog storage tank, incorrect inhalation speed and force, and air leakage during inhalation of medication.
Asthma severity in children
In this study, the severity of asthma was divided into mild intermittent, mild persistent, moderate persistent, and severe persistent according to The Routine for Prevention and Treatment of Bronchial Asthma in Children (for trial) [23].
Statistical analysis
Statistical analyses were performed using SPSS 21.0. Numeral data are expressed as number (%), with the differences between groups compared using the χ2 or Fisher’s exact test. Normally distributed data were compared using the independent-samples t-test, while non-normally distributed data were compared using the nonparametric test. The multiple logistic regression analysis was performed to predict risk factors for asthma with SDB and poor asthma control. The strength of association is expressed as the odds ratio (OR) and 95% confidence interval (CI). A p-value < 0.05 was considered to be statistically significant.
Results
Study population
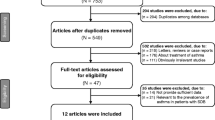
Of a total of 486 children, 89 were excluded according to the exclusion criteria. Finally, a total of 397 children were enrolled, including 252 (63.5%) boys and 145 (36.5%) girls, with a male-to-female ratio of 1.74:1, and an average age of 5.70 ± 2.53 years. Table 1 shows the demographic and clinical characteristics of the patients.
Clinical features of SDB
According to PSQ-SRBD findings, 86 (21.6%) children had a high risk of SDB. Table 2 shows the demographic and clinical characteristics of children with and without a high risk of SDB. The two groups differed significantly in prevalence of allergic rhinitis, chronic tonsillitis, gastroesophageal reflux (GER), allergic skin disease, allergy, adenoid hypertrophy, tonsil hypertrophy, and family snoring history (p < 0.05) but did not differ significantly in age, sex, nationality, residence, birth history, breastfeeding duration, or BMI (Table 2).
The multifactorial binary logistic regression analysis revealed that allergic rhinitis (OR = 3.316, 95% CI: 1.721–6.389), GER (OR = 7.518, 95% CI: 1.905–29.664), chronic tonsillitis (OR = 2.246, 95% CI: 1.075–4.693), adenoid hypertrophy (OR = 3.479, 95% CI: 1.708–7.085), recurrent respiratory infections (OR = 2.195, 95% CI: 1.207–3.988), and family snoring history (OR = 2.048, 95% CI: 1.097–3.825) were risk factors for asthma in children with SDB (p < 0.05; Table 3).
Asthma control
According to c-ACT and TRACK results, asthma was poorly controlled in 78 (19.6%) children. There were 107 (26.9%) children did not take medicine regularly for asthma control, in which 65 (60.7%) children missed doses. In the univariate analysis, the well- and poorly controlled asthma groups did not differ significantly in terms of sex, BMI, obesity, allergic rhinitis, chronic tonsillitis, allergic skin disease, allergy, or passive-smoking status (Table 4) but differed significantly in terms of SDB and irregular medication use. Moreover, the prevalence of SDB was higher in the poorly controlled asthma control than in the well-controlled asthma group (34.6% vs. 18.5%; p < 0.05).
In the binary logistics regression analysis, after correcting for mixed factors, such as age, sex, BMI, allergic rhinitis, and allergy, SDB (OR = 2.391, 95% CI: 1.302–4.393) and irregular medication use (OR = 2.571, 95% CI: 1.498–4.414) were independent risk factors for poor asthma control (Table 5).
Asthma severity
The rank sum test showed that there was a difference in the severity of asthma between the SDB positive group and the SDB negative group ( p < 0.05 ). Children in the SDB positive group have more severe asthma(Table 6).
Discussion
In this study, asthma was more common in boys, with a male-to-female ratio of 1.74:1, slightly higher than that of 1.5:1 reported in the third epidemiological report on childhood asthma in mainland China [3]. Asthma is often associated with one or more comorbidities. In this study, allergic rhinitis was the most common complication, with a prevalence of approximately 53.6%, consistent with previous reports [24, 25]. Allergic reaction is the main pathogenic factor of asthma. In this study, the prevalence of allergy in children with asthma was 59.6%.
In this study, the prevalence of a high risk of SDB in children with asthma was consistent with previous studies [10, 26, 27], significantly higher than that of SDB in children without asthma (12%) reported in a multicenter epidemiological study in China [28]. This result suggested that children with asthma are more prone to SDB. Asthma is a risk factor for SDB [26, 29,30,31], probably because of altered sleep architecture and increased respiratory muscle effort in children with asthma, which may aggravate upper airway collapse. Further, the systemic inflammatory response plays a role. Asthma may promote the release of various inflammatory factors, promoting the proliferation of lymphoid tissues in the upper airways, thus aggravating upper airway obstruction. In addition, long-term use of glucocorticoids in children with asthma may contribute to redistribution of fat around the pharynx and reduced local muscle contractile properties, leading to upper airway collapse, thus triggering and aggravating SDB and even OSAS [32, 33].
In this study, the univariate and multivariate analysis results of the PSQ-SRBD findings of SDB-positive and SDB-negative children with asthma revealed that allergic rhinitis, GER, chronic tonsillitis, adenoid hypertrophy, recurrent respiratory infections, and a family history of snoring were independent risk factors for SDB in children with asthma. Compared to children without allergic rhinitis, the risk of SDB was higher in those with allergic rhinitis. This result indicated that allergic rhinitis was a risk factor for SDB in children with asthma, consistent with a previous report [34]. The reason may be that the nasal cavity is the main breathing route during sleep. As the primary clinical manifestation of allergic rhinitis, nasal obstruction increases airway resistance and may lead to mouth breathing, sleep fragmentation, and excessive fatigue, thus causing SDB [35,36,37]. In addition, the immune response to antigens and other inflammatory stimuli in children with rhinitis causes lymphocyte hypertrophy. It stimulates tonsil and adenoid hyperplasia, which leads to obstruction of the nasopharyngeal and oropharyngeal passages and causes SDB [38, 39].
GER is a physiological process of retrograde entry of gastric contents into the esophagus due to relaxation of the lower esophageal sphincter. During wakefulness, it often occurs after meals and is rapidly cleared by swallowing, while during sleep, it occurs upon awakening. When it occurs in children, the throat is closed to prevent asphyxia, leading to apnea, thereby increasing the risk of SDB [40]. Co-existing GER increases the prevalence of SDB, and its treatment can improve SDB symptoms [41,42,43]. The adenoid is a lymphatic tissue located at the junction of the parietal and posterior walls of the nasopharynx and is part of the inner pharyngeal lymphatic ring. Adenoid hypertrophy is a leading risk factor for SDB [44, 45]. The adenoid size is associated with the severity of SDB [46,47,48]. Our findings also suggest that adenoid hypertrophyis a risk factor for SDB.
The tonsil is the first line of defense of human immune organs and is susceptible to bacterial and viral attacks. Chronic tonsillitis and SDB can coexist [49]. Sarmiento et al. [50] confirmed that B-cell hyperplasia and hypertrophy caused by OSAS result from chronic tonsillitis. Our findings also supported that chronic tonsillitis is a risk factor for SDB. In addition, LingShen et al. found that OSAS in children was closely associated with upper respiratory tract infections [47], consistent with our results, probably because they can increase inflammatory factors and promote tonsillar hypertrophy, thus causing or aggravating SDB.
In the present study, the family history of snoring was a risk factor for SDB, consistent with a previous report [37]. This finding suggested that family characteristics, such as body fat distribution and craniofacial features, may be involved in the pathogenesis of SDB [51].
Epidemiological studies have shown that asthma is increasing in prevalence yearly and has become a severe public health concern. In Chinese children, asthma is not well-controlled overall. In this study, 19.6% of children had poorly controlled asthma, lower than the rate reported from Turkey (39.5%) [27] but higher than that reported from South Korea (9.1%) [10]. The univariate and multivariate analyses of children with poorly controlled asthma showed that SDB and irregular medication use were independent risk factors for poor asthma control.
This study found that SDB was associated with not only poor asthma control, but also asthma severity, consistent with previous studies [9, 11, 12, 27, 52]. This may be because SDB can change the oropharyngeal reflex and increase intrathoracic negative pressure and airway vagus nerve tension, resulting in bronchial contraction, thus aggravating asthma. Local and systemic inflammatory responses are also involved [36]. Children with SDB repeatedly snore, leading to intermittent vibrations of the upper airways and soft tissue damage, resulting in local inflammation and edema. According to the united airway disease hypothesis, repeated snoring can theoretically lead to lower airway inflammation and worsening of asthma [53].
In the present study, 26.9% of children did not adhere to the prescribed medication for asthma control. The risk of poor asthma control was 1.571 times higher in children who did not take the prescribed medication regularly than those who did, suggesting that poor medication compliance is a critical factor affecting asthma control, consistent with previous reports [54,55,56]. Therefore, in clinical practice, individualized interventions should be undertaken to improve treatment compliance by changing the cognition of children and parents.
The strengths of this study include the reports of the prevalence and risk factors of SDB in children with asthma. Further, this was the first study on SDB and asthma control in China. However, this study has some limitations. First, this was a single-center, small-scale, cross-sectional observational study, which might be associated with selection bias and recall bias. In the future, prospective and cohort studies should be performed to validate that treating SDB can improve asthma control. Second, the risk of SDB was determined by PSQ-SRBD instead of objective tools (e.g., polysomnography), thus we could not make a definite diagnosis of SDB and could not determine the SDB subtypes, such as OSA and central sleep apnea (CSA).
Conclusions
In summary, SDB is closely related to childhood asthma, and the combination of SDB may affect the severity and clinical control of asthma. We found that allergic rhinitis, chronic tonsillitis, gastroesophageal reflux, adenoid hypertrophy, recurrent respiratory tract infection, family snoring history are independent risk factors for SDB in children with asthma. Therefore, in clinical practice, for asthmatic children combined with these risk factors, it is recommended to screen SDB routinely in order to provide better treatment strategies for asthma control.
Data availability
The data that support the findings of this study are not openly available because they are human data and are available from the corresponding author upon reasonable request.
References
National Pediatric Asthma Collaborative Group. A survey on the prevalence of asthma among children in urban areas of China. Chin J Pediatr. 2003;41:123–7.
National Collaborative Group for Childhood Asthma Prevention and Control. A survey on the prevalence of bronchial asthma among 900,000 children aged 0–14 years in China. Chin J Tuberculosis. 1993;16:Z1.
The National Cooperative Group on Childhood Asthma, Institute of Environmental Health and Related Prod. The third epidemiological survey of asthma in Chinese urban children. Chin J Pediatr. 2013;51:729–35.
Editorial Board of Chinese Journal of Pediatrics, Respiratory Group of the Chinese Medical Association, Pediatricians Branch of the Chinese Medical Association, Pediatric Respiratory Specialty Committee of the Chinese Medical Association. Recommendations for standardized diagnosis and treatment of bronchial asthma in children (2020 edition). Chin J Pediatr. 2020;09:708–17.
Hunter SJ, Gozal D, Smith DL, Philby MF, Kaylegian J, Kheirandish-Gozal L. Effect of sleep-disordered breathing severity on cognitive performance measures in a large community cohort of young school-aged children. Am J Respir Crit Care Med. 2016;194:739–47. https://doi.org/10.1164/rccm.201510-2099OC.
Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, Schechter MS, Sheldon SH, Spruyt K, Ward SD, Lehmann C, Shiffman RN, American Academy of P. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130:576–84. https://doi.org/10.1542/peds.2012-1671.
Working Group of Chinese Guideline for the Diagnosis and Treatment of Childhood OSA, Subspecialty Group of Pediatrics, Society of Otorhinolaryngology Head and Neck Surgery, Chinese Medical Association, Subspecialty Group of Respiratory Diseases, Society of Pediatrics, Chinese Medical Association, Society of Pediatric Surgery, Chinese Medical Association, Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery. Chinese guideline for the diagnosis and treatment of childhood obstructive sleep apnea (2020). Chin J Evidence-Based Med. 2020;20:883–900.
Fasano MB. Combined airways: impact of upper airway on lower airway. Curr Opin Otolaryngol Head Neck Surg. 2010;18:15–20. https://doi.org/10.1097/MOO.0b013e328334aa0e.
Li L, Xu Z, Jin X, Yan C, Jiang F, Tong S, Shen X, Li S. Sleep-disordered breathing and asthma: evidence from a large multicentric epidemiological study in China. Respir Res. 2015;16:56. https://doi.org/10.1186/s12931-015-0215-5.
Sheen YH, Choi SH, Jang SJ, Baek JH, Jee HM, Kim MA, Chae KY, Han MY. Poor sleep quality has an adverse effect on childhood asthma control and lung function measures. Pediatr Int. 2017;59:917–22. https://doi.org/10.1111/ped.13312.
Ross KR, Storfer-Isser A, Hart MA, Kibler AM, Rueschman M, Rosen CL, Kercsmar CM, Redline S. Sleep-disordered breathing is associated with asthma severity in children. J Pediatr. 2012;160:736–42. https://doi.org/10.1016/j.jpeds.2011.10.008.
Gunnlaugsson S, Abul MH, Wright L, Petty CR, Permaul P, Gold DR, Gaffin JM, Phipatanakul W. Associations of snoring and asthma morbidity in the school inner-city asthma study. J Allergy Clin Immunol Pract. 2021;9:3679–e36853671. https://doi.org/10.1016/j.jaip.2021.05.022.
Bhattacharjee R, Choi BH, Gozal D, Mokhlesi B. Association of adenotonsillectomy with asthma outcomes in children: a longitudinal database analysis. PLoS Med. 2014;11:e1001753. https://doi.org/10.1371/journal.pmed.1001753.
Goldstein NA, Thomas MS, Yu Y, Weaver DE, Watanabe I, Dimopoulos A, Wasserman J, Ahmad SQ, Ednick M, Vastola AP, Weedon J. The impact of adenotonsillectomy on pediatric asthma. Pediatr Pulmonol. 2019;54:20–6. https://doi.org/10.1002/ppul.24207.
Mayor S. Adenotonsillectomy reduces acute asthma exacerbations in children, study shows. BMJ. 2014;349:g6575. https://doi.org/10.1136/bmj.g6575.
Li F, Zong XN. Growth standard values and standardized growth curves of body weight and body mass index for length/height in Chinese children under seven years of age. Chin J Pediatr. 2009;04:281–5.
Pulmonary Function Collaborative Group of the Respiratory Group of the Paediatrics Branch of the Chinese Medical Association. Editorial Board of the Chinese Journal of practical pediatrics. (2016) Guideline series on pulmonary function in children(ii):lung volume and ventilation function. Chin J Appl Clin Pediatr 31:744–50.
Host A, Andrae S, Charkin S, Diaz-Vazquez C, Dreborg S, Eigenmann PA, Friedrichs F, Grinsted P, Lack G, Meylan G, Miglioranzi P, Muraro A, Nieto A, Niggemann B, Pascual C, Pouech MG, Rance F, Rietschel E, Wickman M. Allergy testing in children: why, who, when and how? Allergy. 2003;58:559–69. https://doi.org/10.1034/j.1398-9995.2003.00238.x.
Li XD, Tai J, Xu ZF, Peng XX, Feng GS, Zhang YM, Zhang J, Guo YL, Xiao YF. Reliability and validity assessment of the simplified Chinese version of the children’s sleep questionnaire applied to screening children with obstructive sleep apnea syndrome in beijing. Chin J Otolaryngology-Head Neck Surg. 2016;51:812–8.
Voorend-van Bergen S, Vaessen-Verberne AA, de Jongste JC, Pijnenburg MW. Asthma control questionnaires in the management of asthma in children: a review. Pediatr Pulmonol. 2015;50:202–8. https://doi.org/10.1002/ppul.23098.
Tosca MA, Schiavetti I, Ciprandi G, ControL’Asma Study G. The challenge of asthma control grading in clinical practice. Respir Investig. 2021;59:683–5. https://doi.org/10.1016/j.resinv.2021.06.001.
Kaya A, Erkocoglu M, Akan A, Vezir E, Azkur D, Ozcan C, Civelek E, Toyran M, Ginis T, Misirlioglu ED, Kocabas CN. Track as a complementary tool to gina and naepp guidelines for assessing asthma control in pre-school children. J Asthma. 2014;51:530–5. https://doi.org/10.3109/02770903.2014.887729.
The Subspecialty Group of Respiratory Diseases, The Pediatric Society, Chinese Medical Association and The Editorial Board, Chinese Journal of Pediatrics, Chinese Medical Association,Chen Yuzhi. (2002) The routine for prevention and treatment of bronchial asthma in children (for trial). Chinese Journal of Pediatrics, 2004,42(02): 100–106. https://doi.org/10.3760/cma.j.issn.0578-1310.2004.02.107.
Kou W, Li X, Yao H, Wei P. Meta-analysis of the comorbidity rate of allergic rhinitis and asthma in Chinese children. Int J Pediatr Otorhinolaryngol. 2018;107:131–4. https://doi.org/10.1016/j.ijporl.2018.02.001.
Kumar P, Singh G, Goyal JP, Khera D, Singh K. Association of common comorbidities with asthma in children: a cross-sectional study. Sudan J Paediatr. 2019;19:88–92. https://doi.org/10.24911/SJP.106-1544873451.
Goldstein NA, Aronin C, Kantrowitz B, Hershcopf R, Fishkin S, Lee H, Weaver DE, Yip C, Liaw C, Saadia TA, Abramowitz J, Weedon J. The prevalence of sleep-disordered breathing in children with asthma and its behavioral effects. Pediatr Pulmonol. 2015;50:1128–36. https://doi.org/10.1002/ppul.23120.
Ginis T, Akcan FA, Capanoglu M, Toyran M, Ersu R, Kocabas CN, Civelek E. The frequency of sleep-disordered breathing in children with asthma and its effects on asthma control. J Asthma. 2017;54:403–10. https://doi.org/10.1080/02770903.2016.1220012.
Li S, Jin X, Yan C, Wu S, Jiang F, Shen X. Habitual snoring in school-aged children: environmental and biological predictors. Respir Res. 2010;11:144. https://doi.org/10.1186/1465-9921-11-144.
Ding L, Xiao L, Chen C, Yao HB, Su SP. Meta-analysis of the correlation between wheezing, asthma and sleep breathing disorders in children. Chin J Clin Immun Metaplasia. 2021;15:398–404.
Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159:1527–32. https://doi.org/10.1164/ajrccm.159.5.9809079.
Zandieh SO, Cespedes A, Ciarleglio A, Bourgeois W, Rapoport DM, Bruzzese JM. Asthma and subjective sleep disordered breathing in a large cohort of urban adolescents. J Asthma. 2017;54:62–8. https://doi.org/10.1080/02770903.2016.1188942.
Prasad B, Nyenhuis SM, Imayama I, Siddiqi A, Teodorescu M. Asthma and obstructive sleep apnea overlap: what has the evidence taught us? Am J Respir Crit Care Med. 2020;201:1345–57. https://doi.org/10.1164/rccm.201810-1838TR.
Trivedi M, ElMallah M, Bailey E, Kremer T, Rhein LM. Pediatric obstructive sleep apnea and asthma: clinical implications. Pediatr Ann. 2017;46:e332–5. https://doi.org/10.3928/19382359-20170815-03.
Nguyen-Hoang Y, Nguyen-Thi-Dieu T, Duong-Quy S. Study of the clinical and functional characteristics of asthmatic children with obstructive sleep apnea. J Asthma Allergy. 2017;10:285–92. https://doi.org/10.2147/JAA.S147005.
Kimple AJ, Ishman SL. Allergy and sleep-disordered breathing. Curr Opin Otolaryngol Head Neck Surg. 2013;21:277–81. https://doi.org/10.1097/MOO.0b013e32835ff132.
Rogers VE, Bollinger ME, Tulapurkar ME, Zhu S, Hasday JD, Pereira KD, Scharf SM. Inflammation and asthma control in children with comorbid obstructive sleep apnea. Pediatr Pulmonol. 2018;53:1200–7. https://doi.org/10.1002/ppul.24074.
Gokdemir Y, Civelek E, Cakir B, Demir A, Kocabas CN, Ikizoglu NB, Karakoc F, Karadag B, Ersu R. Prevalence of sleep-disordered breathing and associated risk factors in primary school children in urban and rural environments. Sleep Breath. 2021;25:915–22. https://doi.org/10.1007/s11325-020-02206-x.
D’Elia C, Gozal D, Bruni O, Goudouris E, Meira ECM. Allergic rhinitis and sleep disorders in children - coexistence and reciprocal interactions. J Pediatr (Rio J). 2021. https://doi.org/10.1016/j.jped.2021.11.010.
Dogru M, Evcimik MF, Calim OF. Does adenoid hypertrophy affect disease severity in children with allergic rhinitis? Eur Arch Otorhinolaryngol. 2017;274:209–13. https://doi.org/10.1007/s00405-016-4196-x.
Konstantinopoulou S, Sideris GA, DelRosso LM. The role of co-morbidities. Curr Probl Pediatr Adolesc Health Care. 2016;46:7–10. https://doi.org/10.1016/j.cppeds.2015.10.010.
Machado R, Woodley FW, Skaggs B, Di Lorenzo C, Splaingard M, Mousa H. Gastroesophageal reflux causing sleep interruptions in infants. J Pediatr Gastroenterol Nutr. 2013;56:431–5. https://doi.org/10.1097/MPG.0b013e31827f02f2.
Wasilewska J, Semeniuk J, Cudowska B, Klukowski M, Debkowska K, Kaczmarski M. Respiratory response to Proton pump inhibitor treatment in children with obstructive sleep apnea syndrome and gastroesophageal reflux disease. Sleep Med. 2012;13:824–30. https://doi.org/10.1016/j.sleep.2012.04.016.
Kang B, Anderson CT, Arimura S et al. OUP accepted manuscriptJ. The Plant cell,2022.
Liu DB, Qiu SY, Zhong JW et al. (2008) Diagnosis and treatment of obstructive sleep apnea hypopnea syndrome in children with risk factors. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 43:924–928.
Xu Z, Jiaqing A, Yuchuan L, Shen K. A case-control study of obstructive sleep apnea-hypopnea syndrome in obese and nonobese Chinese children. Chest. 2008;133:684–9. https://doi.org/10.1378/chest.07-1611.
Brooks LJ, Stephens BM, Bacevice AM. Adenoid size is related to severity but not the number of episodes of obstructive apnea in children. J Pediatr. 1998;132:682–6. https://doi.org/10.1016/s0022-3476(98)70360-9.
Shen L, Lin Z, Lin X, Yang Z. Risk factors associated with obstructive sleep apnea-hypopnea syndrome in Chinese children: a single center retrospective case-control study. PLoS ONE. 2018;13:e0203695. https://doi.org/10.1371/journal.pone.0203695.
Tagaya M, Nakata S, Yasuma F, Miyazaki S, Sasaki F, Morinaga M, Suzuki K, Otake H, Nakashima T. Relationship between adenoid size and severity of obstructive sleep apnea in preschool children. Int J Pediatr Otorhinolaryngol. 2012;76:1827–30. https://doi.org/10.1016/j.ijporl.2012.09.010.
Ehsan Z, Glynn EF, Hoffman MA, Ingram DG, Al-Shawwa B. Small sleepers, big data: leveraging big data to explore sleep-disordered breathing in infants and young children. Sleep. 2021;44. https://doi.org/10.1093/sleep/zsaa176.
Sarmiento Varon L, De Rosa J, Rodriguez R, Fernandez PM, Billordo LA, Baz P, Beccaglia G, Spada N, Mendoza FT, Barberis CM, Vay C, Arabolaza ME, Paoli B, Arana EI. Role of tonsillar chronic inflammation and commensal bacteria in the pathogenesis of pediatric osa. Front Immunol. 2021;12:648064. https://doi.org/10.3389/fimmu.2021.648064.
Alexopoulos EI, Charitos G, Malakasioti G, Varlami V, Gourgoulianis K, Zintzaras E, Kaditis AG. Parental history of adenotonsillectomy is associated with obstructive sleep apnea severity in children with snoring. J Pediatr. 2014;164:1352–7. https://doi.org/10.1016/j.jpeds.2014.01.021.
Luyster FS, Teodorescu M, Bleecker E, Busse W, Calhoun W, Castro M, Chung KF, Erzurum S, Israel E, Strollo PJ, Wenzel SE. Sleep quality and asthma control and quality of life in non-severe and severe asthma. Sleep Breath. 2012;16:1129–37. https://doi.org/10.1007/s11325-011-0616-8.
Bjermer L. Time for a paradigm shift in asthma treatment: from relieving bronchospasm to controlling systemic inflammation. J Allergy Clin Immunol. 2007;120:1269–75. https://doi.org/10.1016/j.jaci.2007.09.017.
Arcoleo KJ, McGovern C, Kaur K, Halterman JS, Mammen J, Crean H, Rastogi D, Feldman JM. Longitudinal patterns of Mexican and Puerto Rican children’s asthma controller medication adherence and acute healthcare use. Ann Am Thorac Soc. 2019;16:715–23. https://doi.org/10.1513/AnnalsATS.201807-462OC.
Jentzsch NS, Camargos P, Sarinho ES, Bousquet J. Adherence rate to beclomethasone dipropionate and the level of asthma control. Respir Med. 2012;106:338–43. https://doi.org/10.1016/j.rmed.2011.12.001.
Klok T, Kaptein AA, Duiverman EJ, Brand PL. It’s the adherence, stupid (that determines asthma control in preschool children)! Eur Respir J. 2014;43:783–91. https://doi.org/10.1183/09031936.00054613.
Acknowledgements
The authors would like to thank all the reviewers who participated in the review.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
Ling Ding and Donghong Peng conceived and designed the protocol; Minghui Tao and Yanping Zhang collected data; Minghui Tao analyzed the data and wrote the paper.All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by The Children’s Hospital of Chongqing Medical University. Written informed consent from each parent was retrieved. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tao, M., Zhang, Y., Ding, L. et al. Risk factors of sleep-disordered breathing and poor asthma control in children with asthma. BMC Pediatr 24, 288 (2024). https://doi.org/10.1186/s12887-024-04762-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04762-7