Abstract
Purpose
In this study we gathered and analyzed the available evidence regarding 17 different imaging modalities and performed network meta-analysis to find the most effective modality for the differentiation between brain tumor recurrence and post-treatment radiation effects.
Methods
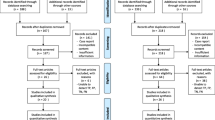
We conducted a comprehensive systematic search on PubMed and Embase. The quality of eligible studies was assessed using the Assessment of Multiple Systematic Reviews-2 (AMSTAR-2) instrument. For each meta-analysis, we recalculated the effect size, sensitivity, specificity, positive and negative likelihood ratios, and diagnostic odds ratio from the individual study data provided in the original meta-analysis using a random-effects model. Imaging technique comparisons were then assessed using NMA. Ranking was assessed using the multidimensional scaling approach and by visually assessing surface under the cumulative ranking curves.
Results
We identified 32 eligible studies. High confidence in the results was found in only one of them, with a substantial heterogeneity and small study effect in 21% and 9% of included meta-analysis respectively. Comparisons between MRS Cho/NAA, Cho/Cr, DWI, and DSC were most studied. Our analysis showed MRS (Cho/NAA) and 18F-DOPA PET displayed the highest sensitivity and negative likelihood ratios. 18-FET PET was ranked highest among the 17 studied techniques with statistical significance. APT MRI was the only non-nuclear imaging modality to rank higher than DSC, with statistical insignificance, however.
Conclusion
The evidence regarding which imaging modality is best for the differentiation between radiation necrosis and post-treatment radiation effects is still inconclusive. Using NMA, our analysis ranked FET PET to be the best for such a task based on the available evidence. APT MRI showed promising results as a non-nuclear alternative.






Similar content being viewed by others
Data Availability
The data used for the current study was compiled from existing studies that were found as detailed in the methods section and the search strategy. The condensed and final list is available from the corresponding author on reasonable request.
References
Bergqvist J, Iderberg H, Mesterton J, Bengtsson N, Wettermark B, Henriksson R (2017) Healthcare resource use, comorbidity, treatment and clinical outcomes for patients with primary intracranial tumors: a Swedish population-based register study. Acta Oncol 56(3):405–414. https://doi.org/10.1080/0284186X.2016.1257864
Suh JH (2010) Stereotactic radiosurgery for the management of brain metastases. N Engl J Med 362(12):1119–1127. https://doi.org/10.1056/NEJMct0806951
Burger PC, Mahley MS, Dudka L, Vogel FS (1979) The morphologic effects of radiation administered therapeutically for intracranial gliomas: a postmortem study of 25 cases. Cancer 44(4):1256–1272. https://doi.org/10.1002/1097-0142(197910)44:4%3c1256::aid-cncr2820440415%3e3.0.co;2-t
Kumar AJ, Leeds NE, Fuller GN, Van Tassel P, Maor MH, Sawaya RE, Levin VA (2000) Malignant gliomas: MR imaging spectrum of radiation therapy- and chemotherapy-induced necrosis of the brain after treatment. Radiology 217(2):377–384. https://doi.org/10.1148/radiology.217.2.r00nv36377
Marks JE, Baglan RJ, Prassad SC, Blank WF (1981) Cerebral radionecrosis: incidence and risk in relation to dose, time, fractionation and volume. Int J Radiat Oncol Biol Phys 7(2):243–252. https://doi.org/10.1016/0360-3016(81)90443-0
Zikou A, Sioka C, Alexiou GA, Fotopoulos A, Voulgaris S, Argyropoulou MI (2018) Radiation Necrosis, pseudoprogression, pseudoresponse, and tumor recurrence: imaging challenges for the evaluation of treated gliomas. Contrast Media Mol Imaging 2018:6828396. https://doi.org/10.1155/2018/6828396
Parvez K, Parvez A, Zadeh G (2014) The diagnosis and treatment of pseudoprogression, radiation necrosis and brain tumor recurrence. Int J Mol Sci 15(7):11832–11846. https://doi.org/10.3390/ijms150711832
Glantz MJ, Burger PC, Friedman AH, Radtke RA, Massey EW, Schold SC (1994) Treatment of radiation-induced nervous system injury with heparin and warfarin. Neurology 44(11):2020–2027. https://doi.org/10.1212/wnl.44.11.2020
Chuba PJ, Aronin P, Bhambhani K, Eichenhorn M, Zamarano L, Cianci P, Muhlbauer M, Porter AT, Fontanesi J (1997) Hyperbaric oxygen therapy for radiation-induced brain injury in children. Cancer 80(10):2005–2012. https://doi.org/10.1002/(sici)1097-0142(19971115)80:10%3c2005::aid-cncr19%3e3.0.co;2-0
Brandes AA, Tosoni A, Spagnolli F, Frezza G, Leonardi M, Calbucci F, Franceschi E (2008) Disease progression or pseudoprogression after concomitant radiochemotherapy treatment: pitfalls in neurooncology. Neuro Oncol 10(3):361–367. https://doi.org/10.1215/15228517-2008-008
Thust SC, van den Bent MJ, Smits M (2018) Pseudoprogression of brain tumors. J Magn Reson Imaging 48(3):571–589. https://doi.org/10.1002/jmri.26171
Kessler AT, Bhatt AA (2018) Brain tumour post-treatment imaging and treatment-related complications. Insights Imaging 9(6):1057–1075. https://doi.org/10.1007/s13244-018-0661-y
Yoon RG, Kim HS, Koh MJ, Shim WH, Jung SC, Kim SJ, Kim JH (2017) Differentiation of recurrent glioblastoma from delayed radiation necrosis by using voxel-based multiparametric analysis of MR imaging data. Radiology 285(1):206–213. https://doi.org/10.1148/radiol.2017161588
Park JE, Lee JY, Kim HS, Oh J-Y, Jung SC, Kim SJ, Keupp J, Oh M, Kim JS (2018) Amide proton transfer imaging seems to provide higher diagnostic performance in post-treatment high-grade gliomas than methionine positron emission tomography. Eur Radiol 28(8):3285–3295. https://doi.org/10.1007/s00330-018-5341-2
Shan Y, Chen X, Lin Y, Wang Y, Zhong S, Gong Y (2016) Value of magnetic resonance spectroscopy and perfusion-weighted imaging in distinguishing glioma recurrence from PTRE: a meta-analysis. Int J Clin Exp Med 9(6):10006–10017
Yu Y, Ma Y, Sun M, Jiang W, Yuan T, Tong D (2020) Meta-analysis of the diagnostic performance of diffusion magnetic resonance imaging with apparent diffusion coefficient measurements for differentiating glioma recurrence from pseudoprogression. Medicine (Baltimore) 99(23):e20270. https://doi.org/10.1097/md.0000000000020270
Chen K, Jiang XW, Deng LJ, She HL (2022) Differentiation between glioma recurrence and treatment effects using amide proton transfer imaging: a mini-Bayesian bivariate meta-analysis. Front Oncol 12:852076. https://doi.org/10.3389/fonc.2022.852076
Patel P, Baradaran H, Delgado D, Askin G, Christos P, John Tsiouris A, Gupta A (2017) MR perfusion-weighted imaging in the evaluation of high-grade gliomas after treatment: a systematic review and meta-analysis. Neuro Oncol 19(1):118–127. https://doi.org/10.1093/neuonc/now148
Alexiou GA, Tsiouris S, Kyritsis AP, Voulgaris S, Argyropoulou MI, Fotopoulos AD (2009) Glioma recurrence versus radiation necrosis: accuracy of current imaging modalities. J Neurooncol 95(1):1–11. https://doi.org/10.1007/s11060-009-9897-1
Chaimani A, Higgins JPT, Mavridis D, Spyridonos P, Salanti G (2013) Graphical tools for network meta-analysis in STATA. PLoS ONE 8(10):e76654. https://doi.org/10.1371/journal.pone.0076654
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Higgins JP, Thompson SG, Spiegelhalter DJ (2009) A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc 172(1):137–159. https://doi.org/10.1111/j.1467-985X.2008.00552.x
Lau J, Ioannidis JP, Schmid CH (1997) Quantitative synthesis in systematic reviews. Ann Intern Med 127(9):820–826. https://doi.org/10.7326/0003-4819-127-9-199711010-00008
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56(11):1129–1135. https://doi.org/10.1016/s0895-4356(03)00177-x
Nyaga VN, Arbyn M (2022) Metadta: a Stata command for meta-analysis and meta-regression of diagnostic test accuracy data – a tutorial. Archives of Public Health 80(1):95. https://doi.org/10.1186/s13690-021-00747-5
Salanti G (2012) Indirect and mixed-treatment comparison, network, or multiple-treatments meta-analysis: many names, many benefits, many concerns for the next generation evidence synthesis tool. Res Syn Meth 3:80–97
Donegan S, Williamson P, Gamble C, Tudur-Smith C (2010) Indirect comparisons: a review of reporting and methodological quality. PLoS ONE 5(11):e11054. https://doi.org/10.1371/journal.pone.0011054
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP (2014) Evaluating the quality of evidence from a network meta-analysis. PLoS ONE 9(7):e99682. https://doi.org/10.1371/journal.pone.0099682
Salanti G, Ades AE, Ioannidis JPA (2011) Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 64(2):163–171. https://doi.org/10.1016/j.jclinepi.2010.03.016
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Furuse M, Nonoguchi N, Yamada K, Shiga T, Combes JD, Ikeda N, Kawabata S, Kuroiwa T, Miyatake SI (2019) Radiological diagnosis of brain radiation necrosis after cranial irradiation for brain tumor: a systematic review. Radiat Oncol 14(1):28. https://doi.org/10.1186/s13014-019-1228-x
Singnurkar A, Poon R, Detsky J (2022) 18F-FET-PET imaging in high-grade gliomas and brain metastases: a systematic review and meta-analysis. J Neurooncol. https://doi.org/10.1007/s11060-022-04201-6
Tsakiris C, Siempis T, Alexiou GA, Zikou A, Sioka C, Voulgaris S, Argyropoulou MI (2020) Differentiation between true tumor progression of glioblastoma and pseudoprogression using diffusion-weighted imaging and perfusion-weighted imaging: systematic review and meta-analysis. World Neurosurg 144:e100–e109. https://doi.org/10.1016/j.wneu.2020.07.218
Taylor C, Ekert JO, Sefcikova V, Fersht N, Samandouras G (2022) Discriminators of pseudoprogression and true progression in high-grade gliomas: a systematic review and meta-analysis. Sci Rep 12(1):13258. https://doi.org/10.1038/s41598-022-16726-x
Kim SJ, Ryul SS (2019) Diagnostic value of radiolabeled amino acid PET for detection of pseudoprogression of brain tumor after treatment: a meta-analysis. Nucl Med Commun 40(9):965–972. https://doi.org/10.1097/mnm.0000000000001060
Li H, Duan Y, Liu N, Dong J, Liang Y, Ju R (2022) Value of DWI combined with magnetic resonance spectroscopy in the differential diagnosis between recurrent glioma and radiation injury: a meta-analysis. Int J Clin Pract 2022:1629570. https://doi.org/10.1155/2022/1629570
Suh CH, Kim HS, Jung SC, Choi CG, Kim SJ (2018) Comparison of MRI and PET as potential surrogate endpoints for treatment response after stereotactic radiosurgery in patients with brain metastasis. AJR Am J Roentgenol 211(6):1332–1341. https://doi.org/10.2214/ajr.18.19674
Yu J, Zheng J, Xu W, Weng J, Gao L, Tao L, Liang F, Zhang J (2018) Accuracy of (18)F-FDOPA positron emission tomography and (18)F-FET positron emission tomography for differentiating radiation necrosis from brain tumor recurrence. World Neurosurg 114:e1211–e1224. https://doi.org/10.1016/j.wneu.2018.03.179
Shah AH, Snelling B, Bregy A, Patel PR, Tememe D, Bhatia R, Sklar E, Komotar RJ (2013) Discriminating radiation necrosis from tumor progression in gliomas: a systematic review what is the best imaging modality? J Neurooncol 112(2):141–152. https://doi.org/10.1007/s11060-013-1059-9
Wan B, Wang S, Tu M, Wu B, Han P, Xu H (2017) The diagnostic performance of perfusion MRI for differentiating glioma recurrence from pseudoprogression: a meta-analysis. Medicine (Baltimore) 96(11):e6333. https://doi.org/10.1097/md.0000000000006333
Zhang H, Ma L, Shu C, Wang YB, Dong LQ (2015) Diagnostic accuracy of diffusion MRI with quantitative ADC measurements in differentiating glioma recurrence from radiation necrosis. J Neurol Sci 351(1–2):65–71. https://doi.org/10.1016/j.jns.2015.02.038
Zhang HM, Huo XB, Wang HL, Wang C (2022) Diagnostic Performance of dynamic susceptibility contrast-enhanced perfusion-weighted imaging in differentiating recurrence from radiation injury in postoperative glioma: a meta-analysis. J Comput Assist Tomogr 46(6):938–944. https://doi.org/10.1097/rct.0000000000001356
Deng SM, Zhang B, Wu YW, Zhang W, Chen YY (2013) Detection of glioma recurrence by 11C-methionine positron emission tomography and dynamic susceptibility contrast-enhanced magnetic resonance imaging: a meta-analysis. Nucl Med Commun 34(8):758–766. https://doi.org/10.1097/MNM.0b013e328361f598
Aseel A, McCarthy P, Mohammed A (2023) Brain magnetic resonance spectroscopy to differentiate recurrent neoplasm from radiation necrosis: a systematic review and meta-analysis. J Neuroimaging. https://doi.org/10.1111/jon.13080
van den Elshout R, Scheenen TWJ, Driessen CML, Smeenk RJ, Meijer FJA, Henssen D. Diffusion imaging could aid to differentiate between glioma progression and treatment-related abnormalities: a meta-analysis. Insights into Imaging 2022;13(1). doi: https://doi.org/10.1186/s13244-022-01295-4
Zhang J, Wang Y, Wang Y, Xiao H, Chen X, Lei Y, Feng Z, Ma X, Ma L (2022) Perfusion magnetic resonance imaging in the differentiation between glioma recurrence and pseudoprogression: a systematic review, meta-analysis and meta-regression. Quant Imaging Med Surg 12(10):4805–4822. https://doi.org/10.21037/qims-22-32
Zhang J, Song Y, He M, Ren Q, Zeng Y, Liu Z, Liu H, Xu J (2018) Diagnostic performance of increased signal intensity within the resection cavity on fluid-attenuated inversion recovery sequences for detection of progression in patients with glioma. World Neurosurg 110:434–441. https://doi.org/10.1016/j.wneu.2017.11.181
Li H, Deng L, Bai HX, Sun J, Cao Y, Tao Y, States LJ, Farwell MD, Zhang P, Xiao B, Yang L (2018) Diagnostic accuracy of amino acid and FDG-PET in differentiating brain metastasis recurrence from radionecrosis after radiotherapy: a systematic review and meta-analysis. AJNR Am J Neuroradiol 39(2):280–288. https://doi.org/10.3174/ajnr.A5472
Wang X, Hu X, Xie P, Li W, Li X, Ma L (2015) Comparison of magnetic resonance spectroscopy and positron emission tomography in detection of tumor recurrence in posttreatment of glioma: a diagnostic meta-analysis. Asia-Pac J Clin Oncol 11(2):97–105. https://doi.org/10.1111/ajco.12202
Belkić D, Belkić K (2012) A meta-analysis of studies using MR spectroscopy for evaluating suspicious lesions after radiation therapy of primary brain tumors. J Math Chem 50(9):2527–2557. https://doi.org/10.1007/s10910-012-0047-1
Caroline I, Rosenthal MA (2012) Imaging modalities in high-grade gliomas: pseudoprogression, recurrence, or necrosis? J Clin Neurosci 19(5):633–637. https://doi.org/10.1016/j.jocn.2011.10.003
Chuang MT (2018) Differentiating radiation-induced necrosis from recurrent brain tumor using MR perfusion and spectroscopy: Ameta-analysis. Neuroradiology 60(1):334–336
Li WF, Zhang YC, Niu C, Guo LP, Liang FL, Ling X, Niu X, Zhang M (2016) Comparison of magnetic resonance spectroscopy and diffusion weighted imaging in the differentiation of glioma recurrence from radiation necrosis: Meta-analysis. Int J Clin Exp Med 9(10):19480–19490
Qiu J, Tao ZC, Deng KX, Wang P, Chen CY, Xiao F, Luo Y, Yuan SY, Chen H, Huang H (2021) Diagnostic accuracy of dynamic contrast-enhanced magnetic resonance imaging for distinguishing pseudoprogression from glioma recurrence: a meta-analysis. Chin Med J (Engl) 134(21):2535–2543. https://doi.org/10.1097/cm9.0000000000001445
Gao L, Xu W, Li T, Zheng J, Chen G (2018) Accuracy of 11C-choline positron emission tomography in differentiating glioma recurrence from radiation necrosis: a systematic review and meta-analysis. Medicine (Baltimore) 97(29):e11556. https://doi.org/10.1097/md.0000000000011556
Cui M, Zorrilla-Veloz RI, Hu J, Guan B, Ma X (2021) Diagnostic accuracy of PET for differentiating true glioma progression from post treatment-related changes: a systematic review and meta-analysis. Front Neurol 12:671867. https://doi.org/10.3389/fneur.2021.671867
de Zwart PL, van Dijken BRJ, Holtman GA, Stormezand GN, Dierckx RAJO, Jan van Laar P, van der Hoorn A. Diagnostic Accuracy of PET Tracers for the Differentiation of Tumor Progression from Treatment-Related Changes in High-Grade Glioma: A Systematic Review and Metaanalysis. J Nucl Med 2020;61(4):498–504. doi: https://doi.org/10.2967/jnumed.119.233809
Li W, Ma L, Wang X, Sun J, Wang S, Hu X (2014) (11)C-choline PET/CT tumor recurrence detection and survival prediction in post-treatment patients with high-grade gliomas. Tumour Biol 35(12):12353–12360. https://doi.org/10.1007/s13277-014-2549-x
Shahideh M, Fallah A, Munoz DG, Loch MR (2012) Systematic review of primary intracranial glioblastoma multiforme with symptomatic spinal metastases, with two illustrative patients. J Clin Neurosci 19(8):1080–1086. https://doi.org/10.1016/j.jocn.2011.09.024
Cicone F, Minniti G, Romano A, Papa A, Scaringi C, Tavanti F, Bozzao A, Maurizi Enrici R, Scopinaro F (2015) Accuracy of F-DOPA PET and perfusion-MRI for differentiating radionecrotic from progressive brain metastases after radiosurgery. Eur J Nucl Med Mol Imaging 42(1):103–111. https://doi.org/10.1007/s00259-014-2886-4
Kano H, Kondziolka D, Lobato-Polo J, Zorro O, Flickinger JC, Lunsford LD (2010) T1/T2 matching to differentiate tumor growth from radiation effects after stereotactic radiosurgery. Neurosurgery 66(3):486–491; discussion 491–482. https://doi.org/10.1227/01.NEU.0000360391.35749.A5
Koh MJ, Kim HS, Choi CG, Kim SJ (2015) Which is the best advanced MR imaging protocol for predicting recurrent metastatic brain tumor following gamma-knife radiosurgery: focused on perfusion method. Neuroradiology 57(4):367–376. https://doi.org/10.1007/s00234-015-1485-9
Hustinx R, Pourdehnad M, Kaschten B, Alavi A (2005) PET imaging for differentiating recurrent brain tumor from radiation necrosis. Radiol Clin North Am 43(1):35–47. https://doi.org/10.1016/j.rcl.2004.09.009
Lohmann P, Kocher M, Ceccon G, Bauer EK, Stoffels G, Viswanathan S, Ruge MI, Neumaier B, Shah NJ, Fink GR, Langen K-J, Galldiks N (2018) Combined FET PET/MRI radiomics differentiates radiation injury from recurrent brain metastasis. Neuroimage Clin 20:537–542. https://doi.org/10.1016/j.nicl.2018.08.024
Yu J, Zheng J, Xu W, Weng J, Gao L, Tao L, Liang F, Zhang J (2018) Accuracy of 18F-FDOPA positron emission tomography and 18F-FET positron emission tomography for differentiating radiation necrosis from brain tumor recurrence. World Neurosurgery 114:e1211–e1224. https://doi.org/10.1016/j.wneu.2018.03.179
Otman H, Farce J, Meneret P, Palard-Novello X, Le Reste PJ, Lecouillard I, Vauleon E, Chanchou M, Carsin Nicol B, Bertaux M, Devillers A, Mariano-Goulart D, Cachin F, Girard A, Le Jeune F (2022) Delayed [18 F]-FDG PET imaging increases diagnostic performance and reproducibility to differentiate recurrence of brain metastases from radionecrosis. Clin Nucl Med 47(9):800–806. https://doi.org/10.1097/RLU.0000000000004305
Qiu J, Tao ZC, Deng KX, Wang P, Chen CY, Xiao F, Luo Y, Yuan SY, Chen H, Huang H (2021) Diagnostic accuracy of dynamic contrast-enhanced magnetic resonance imaging for distinguishing pseudoprogression from glioma recurrence: a meta-analysis. Chin Med J 134(21):2535–2543. https://doi.org/10.1097/CM9.0000000000001445
Zhang H, Ma L, Wang Q, Zheng X, Wu C, Xu BN (2014) Role of magnetic resonance spectroscopy for the differentiation of recurrent glioma from radiation necrosis: a systematic review and meta-analysis. Eur J Radiol 83(12):2181–2189. https://doi.org/10.1016/j.ejrad.2014.09.018
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Richard Dagher, Paloma da Silva de Santana, Mona Gad, Mohammad Amin Sadeghi and Licia P. Luna. The first draft of the manuscript was written by Richard Dagher and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dagher, R., Gad, M., da Silva de Santana, P. et al. Umbrella review and network meta-analysis of diagnostic imaging test accuracy studies in Differentiating between brain tumor progression versus pseudoprogression and radionecrosis. J Neurooncol 166, 1–15 (2024). https://doi.org/10.1007/s11060-023-04528-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04528-8