Abstract
Introduction
The intermittent intrapulmonary deflation (IID) technique is a recent airway clearance technique that intends to delay the onset of expiratory flow limitation (EFL) during exhalation. We showed in a previous study that IID increased the expiratory volume of COPD patients compared to quiet breathing and positive expiratory pressure (PEP) therapy. We hypothesized that it was due to the attenuation of the EFL.
Objectives
To verify the physiologic effects of IID and PEP techniques on EFL with a mechanical lung model.
Methods
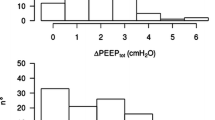
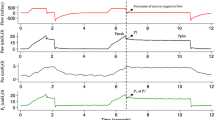
A mechanical lung model was created to assess the effects of IID and PEP techniques. The thorax was simulated by a plexiglas box in which an adult test lung was connected. A calibration syringe simulated the inspiratory phase. Later, with activation of the IID, the expiratory phase was driven by the deflation generated by the device. With PEP, the expiration occurred maintaining an expiratory pressure between 5 and 10 cmH2O. A pneumotachograph and a pressure transducer were placed in series for flow, volumes and pressure measurements.
Results
The model reproduced physiological characteristics of EFL. However, the deflation of the model was slowed by IID and PEP, and flow remained almost constant, so flow limitation was reduced.
Conclusion
The IID and PEP attenuate EFL and increase exhaled volume in the in vitro model.





Similar content being viewed by others
References
Tantucci C. Expiratory flow limitation definition, mechanisms, methods, and significance. Pulm Med. 2013;2013:749860.
Aarli BB, Calverley PM, Jensen RL, Dellaca R, Eagan TM, Bakke PS, et al. The association of tidal EFL with exercise performance, exacerbations, and death in COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2179–88.
Fry DL, Hyatt RE. Pulmonary mechanics. A unified analysis of the relationship between pressure, volume and gasflow in the lungs of normal and diseased human subjects. Am J Med. 1960;29:672–89.
The Global Strategy for Diagnosis MaPoC. Global Initiative for Chronic Obstructive Lung Disease (GOLD). 2023 [updated 2023. Available from: https://goldcopd.org/2023-gold-report-2/.
Pride NB, Permutt S, Riley RL, Bromberger-Barnea B. Determinants of maximal expiratory flow from the lungs. J Appl Physiol. 1967;23(5):646–62.
Orvoen-Frija E, Benoit M, Catto M, Chambouleyron M, Duguet A, Emeriau JP, et al. Chronic Obstructive Pulmonary Disease (COPD) in the elderly. Rev Mal Respir. 2010;27(8):855–73.
Global strategy for the. diagnosis, management, and prevention of chronic obstructive pulmonary disease (2020 report). 2020.
Tantucci C. Assessment and treatment of airflow obstruction in patients with chronic obstructive pulmonary disorder: a guide for the clinician. Expert Rev Respir Med. 2021;15(3):385–91.
Chiari S, Bassini S, Braghini A, Corda L, Boni E, Tantucci C. Tidal expiratory flow limitation at rest as a functional marker of pulmonary Emphysema in moderate-to-severe COPD. COPD. 2014;11(1):33–8.
Fagevik Olsen M, Lannefors L, Westerdahl E. Positive expiratory pressure - common clinical applications and physiological effects. Respir Med. 2015;109(3):297–307.
Clini E. Positive expiratory pressure techniques in respiratory patients: old evidence and new insights. Breathe. 2009;6(2):153–9.
Fagevik Olsen M, Westerdahl E. Positive expiratory pressure in patients with Chronic Obstructive Pulmonary disease–a systematic review. Respiration. 2009;77(1):110–8.
Myers TR. Positive expiratory pressure and oscillatory positive expiratory pressure therapies. Respir Care. 2007;52(10):1308–26. discussion 27.
Walicka-Serzysko K, Postek M, Jeneralska N, Cichocka A, Milczewska J, Sands D. ePS3.09 the effect of chest physiotherapy with the Simeox airway clearance technology in the treatment of cystic fibrosis pulmonary exacerbation - open-label study. J Cyst Fibros. 2019;18:46–S7.
Ribeiro Fonseca Franco, de Macedo J, Reychler G, Liistro G, Poncin W. Short-term effect of the intermittent intrapulmonary deflation technique on air trapping in patients with Chronic Obstructive Pulmonary Disease. Respiratory Care In press.
West JB. Pulmonary Pathophysiology. The Williams and Wilkins Company. 1978:p.227.
Giovannetti P, Morin L, Lafforgue O, Poncet S, Favier J, Reynaud-Gaubert M. Étude SIMETOL: évaluation de la tolérance et l’efficacité d’une procédure innovante de drainage bronchique assistée par Simeox® dans la mucoviscidose en alternative à La kinésithérapie respiratoire conventionnelle. Rev Mal Respir. 2019;36:A22.
Zach MS. The physiology of forced expiration. Paediatr Respir Rev. 2000;1(1):36–9.
O’Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2001;164(5):770–7.
Bellone A, Spagnolatti L, Massobrio M, Bellei E, Vinciguerra R, Barbieri A, et al. Short-term effects of expiration under positive pressure in patients with acute exacerbation of Chronic Obstructive Pulmonary Disease and mild acidosis requiring non-invasive positive pressure ventilation. Intensive Care Med. 2002;28(5):581–5.
Funding
The Simeox device was lent by the company PhysioAssist for the whole duration of this study. The company had no involvement in this study in any way.
Author information
Authors and Affiliations
Contributions
JRFFM and GL designed and drafted the study, analysed the data, and revised the manuscript. GR and WP provided critical revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
Ethics approval
The ancillary study mentioned was carried out in accordance with the Helsinki Declaration and approved by Comité d’Éthique Hospitalo-Facultaire Saint-Luc – UCL no. B403201940373 and registered at Clinical Trial as NCT04157972.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ribeiro Fonseca Franco de Macedo, J., Reychler, G., Poncin, W. et al. Effects of the intermittent intrapulmonary deflation technique on expiratory flow limitation: an in vitro study. J Clin Monit Comput 38, 69–75 (2024). https://doi.org/10.1007/s10877-023-01093-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01093-3