Abstract
Collagen membranes with high robustness and a defined stable biodegradation are of a great interest for dental surgery. Electrophoretic deposition (EPD) is a perspective candidate technology for their production, and in this article, the authors demonstrated the capabilities of its modification, a semipermeable barrier-assisted EPD (SBA-EPD). The SBA-EPD process was carried out at 60 V for 1,2, or 3 cycles 20 min each, after which the obtained membranes were crosslinked with 0.625% genipin. SBA-EPD allowed for the fabrication of membranes with high collagen packing density (0.0012 g/mm3) and high robustness, which depended on the number of SBA-EPD cycles. The highest Young’s modulus, tensile strength, and strain at failure values of non-crosslinked samples corresponded to 3-cycle deposition (15.11 ± 1.78 MPa, 4.2 ± 1.6 MPa, 60 ± 12%, respectively). However, crosslinking diminished the statistical difference of these parameters among membranes of different deposition cycles (reaching for 3-cycle deposition 64 ± 5 MPa, 9.5 ± 1.1 MPa, 23.7 ± 2.0%, respectively). On day 21 after subcutaneous implantation, the non-crosslinked membranes showed a significant degree of resorption higher than that of crosslinked ones by 3.5 times in absolute values. As well, crosslinked membranes elicited a greater peri-implant pro-fibrotic and giant cell response. Overall, the mechanical characteristics of SBA-EPD membranes were mostly superior to commercially available products used for dental applications, while their biodegradation timeframes fitted the optimal window. The authors hope that their research will attract the attention to SBA-EPD as an emerging and perspective technology for the production of robust and defect-free collagen membranes for dental surgery.
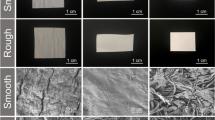
Graphical abstract








Similar content being viewed by others
References
Wang Y, Wang Z, Dong Y (2023) Collagen-based biomaterials for tissue engineering. ACS Biomater Sci Eng 9:1132–1150. https://doi.org/10.1021/acsbiomaterials.2c00730
Shekhter AB, Fayzullin AL, Vukolova MN, Rudenko TG, Osipycheva VD, Litvitsky PF (2017) Medical applications of collagen and collagen-based materials. Curr Med Chem 26:506–516
Patino MG, Neiders ME, Andreana S, Noble B, Cohen RE (2002) Collagen as an implantable material in medicine and dentistry. J Oral Implantol 28:220–225
Rastogi S, Modi M, Sathian B (2009) The efficacy of collagen membrane as a biodegradable wound dressing material for surgical defects of oral mucosa: a prospective study. J Oral Maxillofac Surg 67:1600–1606. https://doi.org/10.1016/j.joms.2008.12.020
Frolova A, Aksenova N, Novikov I, Maslakova A, Gafarova E, Efremov Y, Bikmulina P, Elagin V, Istranova E, Kurkov A, Shekhter A, Kotova S, Zagaynova E, Timashev P (2021) A collagen basketweave from the giant squid mantle as a robust scaffold for tissue engineering. Mar Drugs 19:679. https://doi.org/10.3390/md19120679
Hoshiba T, Lu H, Kawazoe N, Chen G (2010) Decellularized matrices for tissue engineering. Expert Opin Biol Ther 10:1. https://doi.org/10.1517/14712598.2010.534079
Grebenik EA, Gafarova ER, Istranov LP, Istranova EV, Ma X, Xu J, Guo W, Atala A, Timashev PS (2020) Mammalian pericardium-based bioprosthetic materials in xenotransplantation and tissue engineering. Biotechnol J. https://doi.org/10.1002/biot.201900334
Liao J, Xu B, Zhang R, Fan Y, Xie H, Li X (2020) Applications of decellularized materials in tissue engineering: advantages, drawbacks and current improvements, and future perspectives. J Mater Chem B 8:10023–10049. https://doi.org/10.1039/d0tb01534b
Fayzullin A, Vladimirov G, Kuryanova A, Gafarova E, Tkachev S, Kosheleva N, Istranova E, Istranov L, Efremov Y, Novikov I, Bikmulina P, Puzakov K, Petrov P, Vyazankin I, Nedorubov A, Khlebnikova T, Kapustina V, Trubnikov P, Minaev N, Kurkov A, Royuk V, Mikhailov V, Parshin D, Solovieva A, Lipina M, Lychagin A, Timashev P, Svistunov A, Fomin V, Shpichka A (2022) A defined road to tracheal reconstruction: laser structuring and cell support for rapid clinic translation. Stem Cell Res Ther 1:1–22. https://doi.org/10.1186/s13287-022-02997-8
Galiano F, Briceño K, Marino T, Molino A, Christensen KV, Figoli A (2018) Advances in biopolymer-based membrane preparation and applications. J Memb Sci 564:562–586. https://doi.org/10.1016/j.memsci.2018.07.059
Weadock K, Olson RM, Silver FH (1983) Evaluation of collagen crosslinking techniques. Biomater Med Devices Artif Organs 11:293–318. https://doi.org/10.3109/10731198309118815
Chen X, Zhou L, Xu H, Yamamoto M, Shinoda M, Kishimoto M, Tanaka T, Yamane H (2020) Effect of the application of a dehydrothermal treatment on the structure and the mechanical properties of collagen film. Materials (Basel) 13:377. https://doi.org/10.3390/ma13020377
Wess TJ, Orgel JP (2000) Changes in collagen structure: Drying, dehydrothermal treatment and relation to long term deterioration. Thermochim Acta 365:119–128. https://doi.org/10.1016/S0040-6031(00)00619-5
Penkova R, Goshev I, Gorinstein S, Nedkov P (1999) Stability of collagen during denaturation. J Protein Chem 18:397–401. https://doi.org/10.1023/A:1020632424142
Hayashi T, Nagai Y (1973) Effect in of pH on the stability of collagen molecule solution. J Biochem 73:999–1006
Li Z, Bin Xie M, Li Y, Ma Y, Li JS, Dai FY (2016) Recent progress in tissue engineering and regenerative medicine. J Biomater Tissue Eng 6:3263. https://doi.org/10.1166/jbt.2016.1510
Kane RJ, Weiss-Bilka HE, Meagher MJ, Liu Y, Gargac JA, Niebur GL, Wagner DR, Roeder RK (2015) Hydroxyapatite reinforced collagen scaffolds with improved architecture and mechanical properties. Acta Biomater 17:16–25. https://doi.org/10.1016/j.actbio.2015.01.031
Wortmann M, Frese N, Sabantina L, Petkau R, Kinzel F, Gölzhäuser A, Moritzer E, Hüsgen B, Ehrmann A (2019) New polymers for needleless electrospinning from low-toxic solvents. Nanomaterials 9:52. https://doi.org/10.3390/nano9010052
Luo X, Guo Z, He P, Chen T, Li L, Ding S, Li H (2018) Study on structure, mechanical property and cell cytocompatibility of electrospun collagen nanofibers crosslinked by common agents. Int J Biol Macromol 113:476–486. https://doi.org/10.1016/j.ijbiomac.2018.01.179
Li J, Wu S, Kim E, Yan K, Liu H, Liu C, Dong H, Qu X, Shi X, Shen J, Bentley WE, Payne GF (2019) Electrobiofabrication: electrically based fabrication with biologically derived materials. Biofabrication 11:032002. https://doi.org/10.1088/1758-5090/ab06ea
Besra L, Liu M (2007) A review on fundamentals and applications of electrophoretic deposition (EPD). Prog Mater Sci 52:1–61. https://doi.org/10.1016/j.pmatsci.2006.07.001
Sikkema R, Baker K, Zhitomirsky I (2020) Electrophoretic deposition of polymers and proteins for biomedical applications. Adv Colloid Interface Sci 284:102272. https://doi.org/10.1016/j.cis.2020.102272
Barrett DJ, Linley MD, Best SM, Cameron RE (2019) Fabrication of free standing collagen membranes by pulsed-electrophoretic deposition. Biofabrication 11:045017. https://doi.org/10.1088/1758-5090/ab331d
Cheng X, Gurkan UA, Dehen CJ, Tate MP, Hillhouse HW, Simpson GJ, Akkus O (2008) An electrochemical fabrication process for the assembly of anisotropically oriented collagen bundles. Biomaterials 29:3278–3288. https://doi.org/10.1016/j.biomaterials.2008.04.028
Uquillas JA, Akkus O (2012) Modeling the electromobility of type-i collagen molecules in the electrochemical fabrication of dense and aligned tissue constructs. Ann Biomed Eng 40:1641–1653. https://doi.org/10.1007/s10439-012-0528-1
Fiegenbaum F, Martini EM, De Souza MO, Becker MR, De Souza RF (2013) Hydrogen production by water electrolysis using tetra-alkyl-ammonium- sulfonic acid ionic liquid electrolytes. J Power Sources 243:822–825. https://doi.org/10.1016/j.jpowsour.2013.06.077
Nguyen T-UTU, Shojaee M, Bashur CA, Kishore V (2019) Electrochemical fabrication of a biomimetic elastin-containing bi-layered scaffold for vascular tissue engineering. Biofabrication 11:15007. https://doi.org/10.1088/1758-5090/aaeab0
Lei M, Qu X, Liu H, Liu Y, Wang S, Wu S, Bentley WE, Payne GF, Liu C (2019) Programmable electrofabrication of porous janus films with tunable janus balance for anisotropic cell guidance and tissue regeneration. Adv Funct Mater 29:1900065. https://doi.org/10.1002/adfm.201900065
Uchikoshi T, Ozawa K, Hatton BD, Sakka Y (2001) Dense, bubble-free ceramic deposits from aqueous suspensions by electrophoretic deposition. J Mater Res 16:321–324. https://doi.org/10.1557/JMR.2001.0048
Liu X, Jiang Y, He H, Ping W (2014) Hydrogen peroxide-induced degradation of type I collagen fibers of tilapia skin. Food Struct 2:41–48. https://doi.org/10.1016/j.foostr.2014.08.001
Valdes D, Tellez J, Keenan K (2019) Effect of hydrogen peroxide on collagen. FASEB J 33:783–785. https://doi.org/10.1096/fasebj.2019.33.1_supplement.783.5
Nashchekina YA, Starostina AA, Trusova NA, Sirotkina MY, Lihachev AI, Nashchekin AV (2020) Molecular and fibrillar structure collagen analysis by FTIR spectroscopy. J Phys Conf Ser. https://doi.org/10.1088/1742-6596/1697/1/012053
Artman D, Flanagan TB (1972) Desorption of hydrogen from palladium and palladium-silver alloys followed by differential scanning calorimetry. Can J Chem 50:1321–1324. https://doi.org/10.1139/v72-207
Millet P, Srour M, Faure R, Durand R (2001) A study of the hydrogen absorption and desorption reactions in palladium electrodes using the potential step method. Electrochem Commun 3:478–482. https://doi.org/10.1016/S1388-2481(01)00190-4
Schofield ER (2022) Perspective on the criticality of palladium in organic synthesis. Johnson Matthey Technol Rev. https://doi.org/10.1595/205651323x16698159435925
Tabellion J, Clasen R (2004) Electrophoretic deposition from aqueous suspensions for near-shape manufacturing of advanced ceramics and glasses—applications. J Mater Sci 39:803–811. https://doi.org/10.1023/B:JMSC.0000012907.52051.fb
Ordung M, Lehmann J, Ziegler G (2004) Fabrication of fibre reinforced green bodies by electrophoretic deposition of silicon powder from aqueous suspensions. J Mater Sci. https://doi.org/10.1023/B:JMSC.0000012918.84125.39
Li WW, Wang HY, Zhang YQ (2017) A novel chitosan hydrogel membrane by an improved electrophoretic deposition and its characteristics in vitro and in vivo. Mater Sci Eng C 74:287–297. https://doi.org/10.1016/j.msec.2016.12.005
Wang HY, Zhang YQ (2014) Processing and characterisation of a novel electropolymerized silk fibroin hydrogel membrane. Sci Rep 4:6182. https://doi.org/10.1038/srep06182
Elizabeth CR, Michelle BS, James BD, Matthew L (2021) Collagen biomaterials and methods for manufacturing collagen biomaterials. https://lens.org/187-755-293-988-267
Nocera AD, Comín R, Salvatierra NA, Cid MP (2018) Development of 3D printed fibrillar collagen scaffold for tissue engineering. Biomed Microdevices 20:1–13. https://doi.org/10.1007/s10544-018-0270-z
Nečas D, Klapetek P (2012) Gwyddion: an open-source software for SPM data analysis. Cent Eur J Phys 10:152023. https://doi.org/10.2478/s11534-011-0096-2
Efremov YM, Wang WH, Hardy SD, Geahlen RL, Raman A (2017) Measuring nanoscale viscoelastic parameters of cells directly from AFM force-displacement curves. Sci Rep 7:1–14. https://doi.org/10.1038/s41598-017-01784-3
Bikmulina P, Kosheleva N, Efremov Y, Antoshin A, Heydari Z, Kapustina V, Royuk V, Mikhaylov V, Fomin V, Vosough M, Timashev P, Rochev Y, Shpichka A (2022) 3D or not 3D: a guide to assess cell viability in 3D cell systems. Soft Matter 18:2222–2233. https://doi.org/10.1039/d2sm00018k
Gorkun AA, Shpichka AI, Zurina IM, Koroleva AV, Kosheleva NV, Nikishin DA, Butnaru DV, Timashev PS, Repin VS, Saburina IN (2018) Angiogenic potential of spheroids from umbilical cord and adipose-derived multipotent mesenchymal stromal cells within fibrin gel. Biomed Mater 13:044108. https://doi.org/10.1088/1748-605X/aac22d
Shpichka A, Koroleva A, Kuznetsova D, Dmitriev RI, Timashev P (2017) Fabrication and handling of 3D scaffolds based on polymers and decellularized tissues. Adv Exp Med Biol 1035:71–81. https://doi.org/10.1007/978-3-319-67358-5_5
Coïc M, Placet V, Jacquet E, Meyer C (2010) Propriétés mécaniques des membranes de collagne. Rev Stomatol Chir Maxillofac 111:286–290. https://doi.org/10.1016/j.stomax.2010.10.006
Raz P, Brosh T, Ronen G, Tal H ()2019 Tensile properties of three selected collagen membranes. Biomed Res Int. https://doi.org/10.1155/2019/5163603
Salvatore L, Gallo N, Aiello D, Lunetti P, Barca A, Blasi L, Madaghiele M, Bettini S, Giancane G, Hasan M, Borovkov V, Natali ML, Campa L, Valli L, Capobianco L, Napoli A, Sannino A (2020) An insight on type I collagen from horse tendon for the manufacture of implantable devices. Int J Biol Macromol 154:291–306. https://doi.org/10.1016/j.ijbiomac.2020.03.082
Yang S, Shi X, Li X, Wang J, Wang Y, Luo Y (2019) Oriented collagen fiber membranes formed through counter-rotating extrusion and their application in tendon regeneration. Biomaterials 207:61–75. https://doi.org/10.1016/j.biomaterials.2019.03.041
Cassel JM, Kanagy JR (1949) Studies on the purification of collagen. J Res Nat Bur Stand 1934(42):557–565. https://doi.org/10.6028/jres.042.047
De Campos Vidal B, Mello MLS (2011) Collagen type I amide I band infrared spectroscopy. Micron 42:283–289. https://doi.org/10.1016/j.micron.2010.09.010
Santos MH, Silva RM, Dumont VC, Neves JS, Mansur HS, Heneine LGD (2013) Extraction and characterization of highly purified collagen from bovine pericardium for potential bioengineering applications. Mater Sci Eng C 33:790–800. https://doi.org/10.1016/j.msec.2012.11.003
Wan Y, Gao Y, Shao J, Tumarbekova A, Zhang D, Zhu J (2021) Effects of ultrasound and thermal treatment on the ultrastructure of collagen fibers from bovine tendon using atomic force microscopy. Food Chem 347:128985. https://doi.org/10.1016/j.foodchem.2020.128985
Zeugolis DI, Paul RG, Attenburrow G (2008) Factors influencing the properties of reconstituted collagen fibers prior to self-assembly: animal species and collagen extraction method. J Biomed Mater Res Part A 86:892–904. https://doi.org/10.1002/jbm.a.31694
Maache-Rezzoug Z, Rezzoug SA, Allaf K (2002) Development of a new drying process—dehydration by cyclical pressure drops (D.D.S.): application to the collagen gel. Dry Technol 20:109–129. https://doi.org/10.1081/DRT-120001369
Li S-T, Chen H-C, Lee NS, Ringshia R, Yuen D, (2013) A Comparative study of zimmer biomend and biomend extend membranes made at two different manufacturing facilities, pp 1–5
Crapo PM, Gilbert TW, Badylak SF (2011) An overview of tissue and whole organ decellularization processes. Biomaterials 32:3233–3243. https://doi.org/10.1016/j.biomaterials.2011.01.057
Arkhangelsky E, Steubing B, Ben-Dov E, Kushmaro A, Gitis V (2008) Influence of pH and ionic strength on transmission of plasmid DNA through ultrafiltration membranes. Desalination 227:111–119. https://doi.org/10.1016/j.desal.2007.07.017
Gao T, Zhang W, Wang Y, Yang G (2019) DNA compaction and charge neutralization regulated by divalent ions in very low pH solution. Polymers (Basel) 11:337. https://doi.org/10.3390/polym11020337
Kumar VA, Caves JM, Haller CA, Dai E, Liu L, Grainger S, Chaikof EL (2013) Collagen-based substrates with tunable strength for soft tissue engineering. Biomater Sci 1:1193–1202. https://doi.org/10.1039/c3bm60129c
Gigante A, Cesari E, Busilacchi A, Manzotti S, Kyriakidou K, Greco F, Di Primio R, Mattioli-Belmonte M (2009) Collagen I membranes for tendon repair: Effect of collagen fiber orientation on cell behavior. J Orthop Res 27:826–832. https://doi.org/10.1002/jor.20812
Hadi MF, Barocas VH (2013) Microscale fiber network alignment affects macroscale failure behavior in simulated collagen tissue analogs. J Biomech Eng 135:411. https://doi.org/10.1115/1.4023411
Lai VK, Frey CR, Kerandi AM, Lake SP, Tranquillo RT, Barocas VH (2012) Microstructural and mechanical differences between digested collagen-fibrin co-gels and pure collagen and fibrin gels. Acta Biomater 8:4031–4042. https://doi.org/10.1016/j.actbio.2012.07.010
Uquillas JA, Kishore V, Akkus O (2011) Effects of phosphate-buffered saline concentration and incubation time on the mechanical and structural properties of electrochemically aligned collagen threads. Biomed Mater 6:035008. https://doi.org/10.1088/1748-6041/6/3/035008
Grebenik EA, Istranov LP, Istranova EV, Churbanov SN, Shavkuta BS, Dmitriev RI, Veryasova NN, Kotova SL, Kurkov AV, Shekhter AB, Timashev PS (2019) Chemical cross-linking of xenopericardial biomeshes: A bottom-up study of structural and functional correlations. Xenotransplantation 26:e12506. https://doi.org/10.1111/xen.12506
Pavoni JMF, dos Santos NZ, May IC, Pollo LD, Tessaro IC (2021) Impact of acid type and glutaraldehyde crosslinking in the physicochemical and mechanical properties and biodegradability of chitosan films. Polym Bull 78:981–1000. https://doi.org/10.1007/s00289-020-03140-4
Goktas S, Dmytryk JJ, McFetridge PS (2011) Biomechanical behavior of oral soft tissues. J Periodontol 82:1178–1186. https://doi.org/10.1902/jop.2011.100573
Kozaniti FK, Deligianni DD, Georgiou MD, Portan DV (2022) the role of substrate topography and stiffness on MSC cells functions: key material properties for biomimetic bone tissue engineering. Biomimetics 7:7. https://doi.org/10.3390/biomimetics7010007
Gough JE, Scotchford CA, Downes S (2002) Cytotoxicity of glutaraldehyde crosslinked collagen/poly(vinyl alcohol) films is by the mechanism of apoptosis. J Biomed Mater Res 61:121–130. https://doi.org/10.1002/jbm.10145
Fessel G, Cadby J, Wunderli S, Van Weeren R, Snedeker JG (2014) Dose- and time-dependent effects of genipin crosslinking on cell viability and tissue mechanics—toward clinical application for tendon repair. Acta Biomater 10:1897–1906. https://doi.org/10.1016/j.actbio.2013.12.048
Zhang X, Chen X, Yang T, Zhang N, Dong L, Ma S, Liu X, Zhou M, Li B (2014) The effects of different crossing-linking conditions of genipin on type I collagen scaffolds: an in vitro evaluation. Cell Tissue Bank 15:531–541. https://doi.org/10.1007/s10561-014-9423-3
Pek YS, Wan ACA, Ying JY (2010) The effect of matrix stiffness on mesenchymal stem cell differentiation in a 3D thixotropic gel. Biomaterials 31:385–391. https://doi.org/10.1016/j.biomaterials.2009.09.057
Navarrete RO, Lee EM, Smith K, Hyzy SL, Doroudi M, Williams JK, Gall K, Boyan BD, Schwartz Z (2017) Substrate stiffness controls osteoblastic and chondrocytic differentiation of mesenchymal stem cells without exogenous stimuli. PLoS ONE 12:e0170312. https://doi.org/10.1371/journal.pone.0170312
Hopp I, Michelmore A, Smith LE, Robinson DE, Bachhuka A, Mierczynska A, Vasilev K (2013) The influence of substrate stiffness gradients on primary human dermal fibroblasts. Biomaterials 34:5070–5077. https://doi.org/10.1016/j.biomaterials.2013.03.075
Vázquez-Victorio G, Peto-Gutiérrez C, Díaz-Bello B, Cano-Jorge M, Pérez-Calixto D, Jiménez-Escobar A, Espinosa-Matías S, Lara Martínez R, Courson R, Malaquin L, Zamarrón-Hernández D, Hautefeuille M (2019) Building a microfluidic cell culture platform with stiffness control using Loctite 3525 glue. Lab Chip 19:3512–3525. https://doi.org/10.1039/c9lc00649d
Enea D, Henson F, Kew S, Wardale J, Getgood A, Brooks R, Rushton N (2011) Extruded collagen fibres for tissue engineering applications: effect of crosslinking method on mechanical and biological properties. J Mater Sci Mater Med 22:1569–1578. https://doi.org/10.1007/s10856-011-4336-1
Grover CN, Gwynne JH, Pugh N, Hamaia S, Farndale RW, Best SM, Cameron RE (2012) Crosslinking and composition influence the surface properties, mechanical stiffness and cell reactivity of collagen-based films. Acta Biomater 8:3080–3090. https://doi.org/10.1016/j.actbio.2012.05.006
Nair M, Johal RK, Hamaia SW, Best SM, Cameron RE (2020) Tunable bioactivity and mechanics of collagen-based tissue engineering constructs: a comparison of EDC-NHS, genipin and TG2 crosslinkers. Biomaterials 254:120109. https://doi.org/10.1016/j.biomaterials.2020.120109
Zbigniew R, Robert M, Johann J (2003) Multilayer collagen matrix for tissue reconstruction. https://lens.org/094-989-331-971-58X
Aprile P, Letourneur D, Simon-Yarza T (2020) Membranes for guided bone regeneration: a road from bench to bedside. Adv Healthc Mater 9:2000707. https://doi.org/10.1002/adhm.202000707
Al-Maawi S, Vorakulpipat C, Orlowska A, Zrnc TA, Sader RA, James Kirkpatrick C, Ghanaati S (2018) In vivo implantation of a bovine-derived collagen membrane leads to changes in the physiological cellular pattern of wound healing by the induction of multinucleated giant cells: an adverse reaction? Front Bioeng Biotechnol 6:104. https://doi.org/10.3389/fbioe.2018.00104
Barbeck M, Lorenz J, Kubesch A, Bohm N, Booms P, Choukroun J, Sader R, Kirkpatrick CJ, Ghanaati S (2015) Porcine dermis-derived collagen membranes induce implantation bed vascularization via multinucleated giant cells: a physiological reaction? J Oral Implantol 41:e238–e251. https://doi.org/10.1563/aaid-joi-D-14-00274
Fayzullin A, Churbanov S, Ignatieva N, Zakharkina O, Tokarev M, Mudryak D, Khristidis Y, Balyasin M, Kurkov A, Golubeva EN, Aksenova NA, Dyuzheva T, Timashev P, Guller A, Shekhter A (2021) Local delivery of pirfenidone by pla implants modifies foreign body reaction and prevents fibrosis. Biomedicines 9:853. https://doi.org/10.3390/biomedicines9080853
Delgado LM, Bayon Y, Pandit A, Zeugolis DI (2015) To cross-link or not to cross-link? cross-linking associated foreign body response of collagen-based devices. Tissue Eng Part B Rev 21:298–313. https://doi.org/10.1089/ten.teb.2014.0290
Moses O, Vitrial D, Aboodi G, Sculean A, Tal H, Kozlovsky A, Artzi Z, Weinreb M, Nemcovsky CE (2008) Biodegradation of three different collagen membranes in the rat calvarium: a comparative study. J Periodontol 79:905–911. https://doi.org/10.1902/jop.2008.070361
Charulatha V, Rajaram A (1997) Crosslinking density and resorption of dimethyl suberimidate-treated collagen. J Biomed Mater Res 36:478–486. https://doi.org/10.1002/(SICI)1097-4636(19970915)36:4%3c478::AID-JBM5%3e3.0.CO;2-B
Behfarnia P, Khorasani M, Birang R, Abbas F (2012) Histological and histomorphometric analysis of animal experimental dehiscence defect treated with three bio absorbable GTR collagen membrane. Dent Res J (Isfahan) 9:574. https://doi.org/10.4103/1735-3327.104876
Duskova M, Leamerova E, Sosna B, Gojis O (2006) Guided tissue regeneration, barrier membranes and reconstruction of the cleft maxillary alveolus. J Craniofac Surg 17:1153–1160. https://doi.org/10.1097/01.scs.0000236435.90097.7b
Rothamel D, Schwarz F, Sager M, Herten M, Sculean A, Becker J (2005) Biodegradation of differently crosslinked collagen membranes: an experimental study in the rat. Clin Oral Implants Res 16:369–378. https://doi.org/10.1111/j.1600-0501.2005.01108.x
Acknowledgements
The authors would like to thank Anastasia Kurenkova for the help with the proper statistical analysis of the registered data and Viktoria Chernikovich for drawing graphical abstract. The study was carried out using the unique scientific facility Transgenebank. This study was financially supported by the RSF Grant No. 23-15-00481 (membrane production, physicochemical characterization, animal experiments). Research at Sechenov University in the part of the cell experiments and mechanical characterization was funded by the Ministry of Science and Higher Education of the Russian Federation under the grant agreement No. 075-15-2021-596.
Author information
Authors and Affiliations
Contributions
AA, OD, LM, CL, and PT outlined the manuscript. EI and AM prepared and characterized the properties of the collagen suspension. OD and LM performed and described the process of SBA-EPD. YE and ASo measured the membranes’ physicochemical parameters and revealed their crosslinking-related changes. PB, NK, ASh performed the cell experiments and interpreted their results. MK carried out the SEM analysis of the membranes and cells. AF, DB carried out the animal experiments and the subsequent histomorphometric analysis. AA, OD, LM, PB, AF, SK, ASo, AM, MK, ES, YE, XQ, SE, CL, and PT contributed to the discussion. AA and OD drafted the manuscript with editing and revision support from ASh, XQ, LM, ES, PB, AF, EI, NK, SK, DB, SE, CL, and PT. AA and PT coordinated the manuscript preparation. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was approved by the Local Ethical Committee at the Sechenov University (Moscow, Russia). The experiments on animals were conducted in the vivarium at the Sechenov University in accordance with the European Convention (Strasbourg, 1986) and the World Medical Association Declaration of Helsinki on the human treatment of animals (2000).
Additional information
Handling Editor: Christopher Blanford.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Antoshin, A., Dubinin, O., Miao, L. et al. Semipermeable barrier-assisted electrophoretic deposition of robust collagen membranes. J Mater Sci 58, 9675–9697 (2023). https://doi.org/10.1007/s10853-023-08641-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-023-08641-x