Abstract
Objective
Changes of platelet distribution width (PDW) have been observed in women with unexplained recurrent pregnancy loss (URPL). However, relevant previous studies showed inconsistent results. We performed a meta-analysis to comprehensively evaluate the association between PDW and URPL.
Methods
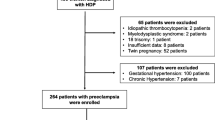
Observational studies reporting the difference of PDW between women with and without URPL were retrieved by searching PubMed, Embase, Web of Science, Wanfang, and CNKI. A random-effect model was used to pool the results by incorporating potential heterogeneity.
Results
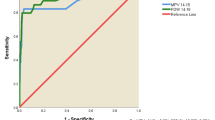
Eleven case-control studies with 1847 women with URPL and 2475 healthy women were included. Age was matched for all studies between cases and controls. Pooled results showed women with URPL had significantly increased level of PDW (mean difference [MD]: 1.54%, 95% CI: 1.04 to 2.03, p < 0.05; I2 =77%). Subgroup analysis showed consistent result for URPL defined as ≥ 2 (MD: 1.45%, p = 0.003) and ≥ 3 (MD: 1.61%, p < 0.001) failed clinical pregnancies, and in studies compared to women with normal pregnancy (MD: 2.02%, p < 0.001) and non-pregnant healthy women (MD: 1.34%, p < 0.001). Results of the meta-analysis also showed that increment of PDW was associated with higher odds of URPL (per 1 unit, odds ratio: 1.26, 95% CI: 1.17 to 1.35, p < 0.001; I2 = 0%).
Conclusions
Women with URPL had significantly increased levels of PDW compared to healthy women without URPL, which suggest that higher PDW may predict the risk of URPL.




Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RPL :
-
recurrent pregnancy loss
- URPL :
-
unexplained recurrent pregnancy loss
- NOS :
-
Newcastle-Ottawa Scale
- PDW :
-
platelet distribution width
References
Dimitriadis E, Menkhorst E, Saito S, Kutteh WH, Brosens JJ. Recurrent pregnancy loss. Nat Rev Dis Primers. 2020;6(1):98. https://doi.org/10.1038/s41572-020-00228-z.
Shahine L, Lathi R. Recurrent pregnancy loss: evaluation and treatment. Obstet Gynecol Clin North Am. 2015;42(1):117–34. https://doi.org/10.1016/j.ogc.2014.10.002.
Hong Li Y, Marren A. Recurrent pregnancy loss: a summary of international evidence-based guidelines and practice. Aust J Gen Pract. 2018;47(7):432–6. https://doi.org/10.31128/AJGP-01-18-4459.
Mashiach S. Recurrent pregnancy loss: causes, controversies, and treatment. Isr Med Assoc J. 2021;23(1):64–5.
Saravelos SH, Regan L. Unexplained recurrent pregnancy loss. Obstet Gynecol Clin North Am. 2014;41(1):157–66. https://doi.org/10.1016/j.ogc.2013.10.008.
Youssef A, van der Hoorn MLP, Dongen M, Visser J, Bloemenkamp K, van Lith J, et al. External validation of a frequently used prediction model for ongoing pregnancy in couples with unexplained recurrent pregnancy loss. Hum Reprod. 2022;37(3):393–9. https://doi.org/10.1093/humrep/deab2646454846.
Zullino S, Clemenza S, Mecacci F, Petraglia F. Low molecular weight heparins (LMWH) and implications along pregnancy: a focus on the placenta. Reprod Sci. 2022;29(5):1414–23. https://doi.org/10.1007/s43032-021-00678-0.
Kwak-Kim J, Yang KM, Gilman-Sachs A. Recurrent pregnancy loss: a disease of inflammation and coagulation. J Obstet Gynaecol Res. 2009;35(4):609–22. https://doi.org/10.1111/j.1447-0756.2009.01079.xJOG1079.
Vagdatli E, Gounari E, Lazaridou E, Katsibourlia E, Tsikopoulou F, Labrianou I. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. Hippokratia. 2010;14(1):28–32.
Leader A, Pereg D, Lishner M. Are platelet volume indices of clinical use? A multidisciplinary review. Ann Med. 2012;44(8):805–16. https://doi.org/10.3109/07853890.2011.653391.
Izzi B, Gialluisi A, Gianfagna F, Orlandi S, De Curtis A, Magnacca S, et al. Platelet distribution width is associated with P-selectin dependent platelet function: results from the Moli-family cohort study. Cells. 2021;10(10):2737. https://doi.org/10.3390/cells10102737.
Borkataky S, Jain R, Gupta R, Singh S, Krishan G, Gupta K, et al. Role of platelet volume indices in the differential diagnosis of thrombocytopenia: a simple and inexpensive method. Hematology. 2009;14(3):182–6. https://doi.org/10.1179/102453309X426182.
Lee E, Kim M, Jeon K, Lee J, Lee JS, Kim HS, et al. Mean platelet volume and platelet distribution width indicate that platelets remain small for most of heir lifespans in patients with essential thrombocythemia. Clin Lab. 2019;65(4) https://doi.org/10.7754/Clin.Lab.2018.180938.
Luzzatto G, de Franchis G, Fabris F, Gerunda GE, Girolami A. Increased proportion of giant platelets and platelet distribution width are better indicators of altered platelet homeostasis than mean platelet volume in liver cirrhosis. Folia Haematol Int Mag Klin Morphol Blutforsch. 1988;115(5):719–26.
Ntaios G, Papadopoulos A, Chatzinikolaou A, Saouli Z, Karalazou P, Kaiafa G, et al. Increased values of mean platelet volume and platelet size deviation width may provide a safe positive diagnosis of idiopathic thrombocytopenic purpura. Acta Haematol. 2008;119(3):173–7. https://doi.org/10.1159/000135658.
Ural U, Bayoglu Tekin Y, Balik G, Kir Sahin F, Colak S. Could platelet distribution width be a predictive marker for unexplained recurrent miscarriage? Arch Gynecol Obstet. 2014;290(2):233–6. https://doi.org/10.1007/s00404-014-3192-x.
Dundar O, Pektas MK, Bodur S, Bakir LV, Cetin A. Recurrent pregnancy loss is associated with increased red cell distribution width and platelet distribution width. J Obstet Gynaecol Res. 2015;41(4):551–8. https://doi.org/10.1111/jog.12600.
Li Q, Ma CY. Significance of Hcy, folic acid, PLT, MPV, and PDW detection in patients with recurrent spontaneous abortion. Int J Lab Med. 2017;38(5):613–4. https://doi.org/10.3969/j.issn.1673-4130.2017.05.015.
Zhang L, Ma Y, Zhu YN, Shen YF, Li S, Zhu B. Associations between RDW-CV, PDW, and NLR with unexplained recurrent miscarriage. Chin J Clin Lab Sci. 2018;36(6):432–4. https://doi.org/10.13602/j.cnki.jcls.2018.06.09.
Li XJ, Yi H, Huang YL, Liu ZY. Correlation analysis of recurrent abortion with thromboelastogram and platelet parameters. Chin J Clin Obstet Gynecol. 2020;21(6):634–5. https://doi.org/10.13390/j.issn.1672-1861.2020.06.026.
Wei ZP, Lin Z. Application value of combined detection of EmAb, CAC, and PDW in clinical diagnosis of recurrent miscarriage. J Mol Diagn Ther. 2021;13(6):977–80. https://doi.org/10.19930/j.cnki.jmdt.2021.06.032.
Zhao Y, He XT. Combined diangostic value of platelet distribution width with neutrophil-lymphocyte ratio for patients with recurrent miscarriage. Chin Remed Clin. 2021;21(12):2156–7. https://doi.org/10.11655/zgywylc2021.12.067.
Lu XJ, Liang JM, Shen LL, Bai YQ, Gao JX, Qin LX, et al. Anlysis for the diagnostic value of different detection methods for recurrent miscarriage. Chin J Lab Diagn. 2022;26(4):480–3. https://doi.org/10.3969/j.issn.1007-4287.2022.04.002.
Fonksiyonları T, İncebıyık A, Hacıvelioğlu S, Gencer M, Güngör A, Coşar E. Is there any relationship between platelet functions, red cell distribution width and recurrent pregnancy loss? J Clin Analytical Med. 2015;6(1):149–51. https://doi.org/10.4328/jcam.1879.
Erdem ZS, Cayir Y, Kosan Z, Erdem HB. Is there any relation between recurrent miscarriage and complete blood count values? A case-control study. Konuralp Medical Journal. 2020;12(1):39–43. https://doi.org/10.18521/ktd.518494.
Qian SJ, Li J, Shen XH. Diagnostic value and clinical significance of combined detection of PDW and NLR in patients with recurrent spontaneous abortion. Int J Lab Med. 2020;41(9):1101–4. https://doi.org/10.3969/j.issn.1673-4130.2020.09.019.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions version 6.2. The Cochrane Collaboration. 2021. www.training.cochrane.org/handbook. Accessed 10 Jan 2023
American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98(5):1103–11. https://doi.org/10.1016/j.fertnstert.2012.06.048.
Liu T, Guo X, Liao Y, Liu Y, Zhu Y, Chen X. Correlation between the presence of antinuclear antibodies and recurrent pregnancy loss: a mini review. Front Endocrinol. 2022;13:873286. https://doi.org/10.3389/fendo.2022.873286.
Scharf RE. Drugs that affect platelet function. Semin Thromb Hemost. 2012;38(8):865–83. https://doi.org/10.1055/s-0032-1328881.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 10 Jan 2023
Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. 2011. www.cochranehandbook.org. Accessed 10 Jan 2023
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Bick RL, Hoppensteadt D. Recurrent miscarriage syndrome and infertility due to blood coagulation protein/platelet defects: a review and update. Clin Appl Thromb Hemost. 2005;11(1):1–13. https://doi.org/10.1177/107602960501100101.
Kotani S, Kamada Y, Shimizu K, Sakamoto A, Nakatsuka M, Hiramatsu Y, et al. Increased plasma levels of platelet factor 4 and beta-thromboglobulin in women with recurrent pregnancy loss. Acta Med Okayama. 2020;74(2):115–22. https://doi.org/10.18926/AMO/58269.
Flood K, Peace A, Kent E, Tedesco T, Dicker P, Geary M, et al. Platelet reactivity and pregnancy loss. Am J Obstet Gynecol. 2010;203(3):281.e1–5. https://doi.org/10.1016/j.ajog.2010.06.023.
Vlachadis N, Tsamadias V, Siori M, Vrachnis N, Economou E. Association of the PECAM-1 (Leu125Val) and P-Selectin (Thr715Pro) gene polymorphisms with unexplained spontaneous miscarriages. Cureus. 2022;14(2):e21859. https://doi.org/10.7759/cureus.21859.
Dendana M, Hizem S, Magddoud K, Messaoudi S, Zammiti W, Nouira M, et al. Common polymorphisms in the P-selectin gene in women with recurrent spontaneous abortions. Gene. 2012;495(1):72–5. https://doi.org/10.1016/j.gene.2011.11.034.
Sansanayudh N, Numthavaj P, Muntham D, Yamwong S, McEvoy M, Attia J, et al. Prognostic effect of mean platelet volume in patients with coronary artery disease. A systematic review and meta-analysis. Thromb Haemost. 2015;114(6):1299–309. https://doi.org/10.1160/TH15-04-0280.
Zheng YY, Wang L, Shi Q. Mean platelet volume (MPV) and platelet distribution width (PDW) predict clinical outcome of acute ischemic stroke: a systematic review and meta-analysis. J Clin Neurosci. 2022;101:221–7. https://doi.org/10.1016/j.jocn.2022.05.019.
Funding
This study was supported by the program named “Application of aspirin or low molecular weight heparin in the treatment of unexplained recurrent early pregnancy failure” (2021MSXM173).
Author information
Authors and Affiliations
Contributions
Yan Shi and Dongmei Xu designed the study, performed literature search, study quality assessment, data collection, statistical analysis, and results interpretation. Yan Shi drafted the manuscript. Dongmei Xu critically revised the manuscript. Yan Shi and Dongmei Xu approved the submission of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, Y., Xu, D. Platelet distribution width and the risk of unexplained recurrent pregnancy loss: a meta-analysis. J Assist Reprod Genet 40, 1523–1531 (2023). https://doi.org/10.1007/s10815-023-02819-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02819-7