Abstract
Background
Currently, there is a disagreement between guidelines regarding platelet count cut-off values as a sign of maternal organ damage in pre-eclampsia; the American College of Obstetricians and Gynecologists guidelines state a cut-off value of < 100 × 109/L; however, the International Society for the Study of Hypertension in Pregnancy guidelines specify a cut-off of < 150 × 109/L. We evaluated the effect of mild thrombocytopenia: platelet count < 150 × 109/L and ≥ 100 × 109/L on clinical features of pre-eclampsia to examine whether mild thrombocytopenia reflects maternal organ damage in pre-eclampsia.
Methods
A total of 264 women were enrolled in this study. Participants were divided into three groups based on platelet count levels at delivery: normal, ≥ 150 × 109/L; mild thrombocytopenia, < 150 × 109/L and ≥ 100 × 109/L; and severe thrombocytopenia, < 100 × 109/L. Risk of severe hypertension, utero-placental dysfunction, maternal organ damage, preterm delivery, and neonatal intensive care unit admission were analyzed based on platelet count levels. Estimated relative risk was calculated with a Poisson regression analysis with a robust error.
Results
Platelet counts indicated normal levels in 189 patients, mild thrombocytopenia in 51 patients, and severe thrombocytopenia in 24 patients. The estimated relative risks of severe thrombocytopenia were 4.46 [95 % confidence interval, 2.59–7.68] for maternal organ damage except for thrombocytopenia, 1.61 [1.06–2.45] for preterm delivery < 34 gestational weeks, and 1.35 [1.06–1.73] for neonatal intensive care unit admission. On the other hand, the estimated relative risks of mild thrombocytopenia were 0.97 [0.41–2.26] for maternal organ damage except for thrombocytopenia, 0.91 [0.62–1.35] for preterm delivery < 34 gestational weeks, and 0.97 [0.76–1.24] for neonatal intensive care unit admission.
Conclusions
Mild thrombocytopenia was not associated with severe features of pre-eclampsia and would not be suitable as a sign of maternal organ damage.
Similar content being viewed by others
Background
Hypertensive disorders of pregnancy (HDP) can cause hypertension and maternal organ damage due to endothelial dysfunction [1, 2]. Among patients with HDP, women who develop maternal organ damage in addition to hypertension are diagnosed with pre-eclampsia, even if they do not develop proteinuria. Coagulation disorders are considered a sign of maternal organ damage in preeclamptic patients [1, 2]. Thrombocytopenia is the most frequently detected coagulation disorder in pre-eclampsia and likely occurs as a result of the injured endothelium activating platelets, leading to elevated consumption of platelets [3, 4]. Pre-eclampsia is the most common cause of thrombocytopenia with evidence of thrombotic microangiopathy in the second and third trimester of pregnancy [5].
Severe thrombocytopenia: platelet count (PC) < 100 × 109/L is a sign of severe pre-eclampsia, and termination of pregnancy should be considered [1]. However, the clinical significance of mild thrombocytopenia (≥ 100 × 109/L and < 150 × 109/L) in pre-eclampsia remains controversial. The International Society for the Study of Hypertension in Pregnancy (ISSHP) guidelines state PC levels < 150 × 109/L as a sign of maternal organ damage, whereas the American College of Obstetricians and Gynecologists guidelines state a cut-off value of < 100 × 109/L [1, 2]. Although termination of pregnancy must be considered in the context of gestational age and other clinical and laboratory results in combination with PC levels, the classification of HDP is affected by whether mild thrombocytopenia is included as a sign of maternal organ damage. Therefore, the discrepancy in PC cut-off values between the two major guidelines makes it difficult to compare studies based on these different guidelines. Actually, a sign of maternal organ damage, including thrombocytopenia (< 150 × 109/L), was included in the criteria of classification of HDP in May 2018 in Japan and it increased the number of women who were diagnosed with pre-eclampsia [6]. To assess whether mild thrombocytopenia reflects maternal organ damage in patients with pre-eclampsia, we examined the impact of mild thrombocytopenia on the severity of pre-eclampsia and perinatal outcomes.
Methods
Study Design and Study Population
This retrospective cross-sectional study was conducted at Hokkaido University Hospital and Japan Community Health Care Organization Hokkaido Hospital, and medical records of women whose delivery happened between April 2010 and May 2019 in the two hospitals were reviewed. Women diagnosed with HDP were included, and the following exclusion criteria were applied in this study: <18 years old at delivery, transferred to other hospitals before delivery, thrombocytopenia not related to HDP, severe congenital anomaly in the baby, twin pregnancy, and insufficient data. Among the patients with HDP, women diagnosed with gestational hypertension and chronic hypertension were also excluded.
Data Collection
According to ISSHP and Japan Society for the Study of Hypertension in Pregnancy guidelines, pre-eclampsia was defined by the new onset of hypertension (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg) accompanied by proteinuria (protein/creatinine ratio ≥ 0.3) and/or a sign of maternal organ damage and utero-placental dysfunction, as listed in Table 1. The women with pre-eclampsia were categorized into three groups according to PC levels at delivery: normal, PC ≥ 150 × 109/L; mild thrombocytopenia, ≥ 100 × 109/L and < 150 × 109/L; and severe thrombocytopenia, < 100 × 109/L. We analyzed the prevalence of severe hypertension (systolic blood pressure ≥ 160 mmHg or diastolic blood pressure ≥ 110 mmHg), maternal organ damage, utero-placental dysfunction, and gestational age at the onset of pre-eclampsia, as well as the rate of neonatal intensive care unit (NICU) admission and preterm delivery < 34 gestational weeks (GW).
Statistical Analyse
Statistical analyses were conducted using Stata/SE version 15.1 (StataCorp). The normality of the data was analyzed by histogram in terms of skewness and kurtosis. Continuous data are reported as mean ± standard deviation. Categorical variables are expressed as frequency and percentage. Statistical significance was calculated using analysis of variance for continuous data, and Fisher’s exact test was used for categorical variables. Multiple comparison procedure was used with Bonferroni method for continuous data and Hochberg method for categorical data. Logistic regression analysis is often used to calculate adjusted odds ratio, which approximates the adjusted relative risk when the outcome prevalence is low. However, odds ratio overestimates relative risk for more common outcomes (> 10 %) [7]. Therefore, to calculate the estimated relative risk (eRR) and 95 % confidence interval (CI), we used a Poisson regression analysis with a robust error variance. Maternal age and PC levels were included as covariates to assess the eRR for severe hypertension, utero-placental dysfunction, and maternal organ damage except thrombocytopenia. In addition to maternal age and PC levels, we included severe hypertension, utero-placental dysfunction, and maternal organ damage except for thrombocytopenia as covariates to assess the eRR for preterm delivery < 34 GW and NICU admission.
Results
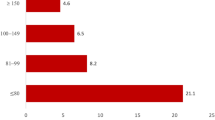
There were 436 women who were diagnosed with HDP during the study period, and 172 of them fulfilled the exclusion criteria and were not included in the analysis. Therefore, 264 women were evaluated in this study (Fig. 1). PC levels were normal in 189 patients, 51 had mild thrombocytopenia, and 24 had severe thrombocytopenia. Table 2 shows the clinical characteristics based on PC levels. The clinical characteristics were not different between the three groups. Table 3 presents the perinatal outcomes and clinical features of pre-eclampsia based on PC levels. GW at the onset of pre-eclampsia (severe thrombocytopenia: 29.7 ± 5.5, normal: 34.1 ± 4.4, p < 0.001, mild thrombocytopenia: 33.7 ± 3.8, p = 0.001) and the day of delivery (severe thrombocytopenia: 31.4 ± 5.2, normal: 35.1 ± 3.9, p < 0.001, mild thrombocytopenia: 34.9 ± 3.6, p = 0.001) were significantly earlier in patients with severe thrombocytopenia although the difference was not detected between the patients with normal PC and those with mild thrombocytopenia. The prevalence of preterm delivery < 34 GW (severe thrombocytopenia: 66.7 %, normal: 34.9 %, p = 0.011, mild thrombocytopenia: 35.3 %, p = 0.028), NICU admission (severe thrombocytopenia: 87.5 %, normal: 53.4 %, p = 0.005, mild thrombocytopenia: 56.9 %, p = 0.019), and maternal organ damage except for thrombocytopenia (severe thrombocytopenia: 54.2 %, normal: 12.2 %, p < 0.001, mild thrombocytopenia: 11.8 %, p < 0.001) were significantly higher in patients with severe thrombocytopenia although the difference was not detected between the patients with normal PC and those with mild thrombocytopenia. The prevalence of severe hypertension and utero-placental dysfunction were equivalent between the three groups.
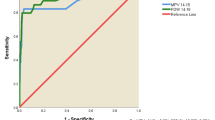
Table 4 shows the age-adjusted eRRs for severe hypertension, utero-placental dysfunction, and maternal organ damage except for thrombocytopenia. Mild and severe thrombocytopenia were not related to severe hypertension and utero-placental dysfunction. Although mild thrombocytopenia was not associated with maternal organ damage except for thrombocytopenia (eRR: 0.97, 95 % CI: 0.41–2.26), severe thrombocytopenia increased the risk of maternal organ damage except for thrombocytopenia (eRR: 4.46, 95 % CI: 2.59–7.68). Table 5 represents the adjusted eRRs for preterm delivery < 34 GW and NICU admission. While mild thrombocytopenia was not related to preterm delivery (eRR: 0.91, 95 % CI: 0.62–1.35) and NICU admission (eRR: 0.97, 95 % CI: 0.76–1.24), severe thrombocytopenia increased the risk of preterm delivery < 34 GW (eRR: 1.61, 95 % CI: 1.06–2.45) and NICU admission (eRR: 1.35, 95 % CI: 1.06–1.73).
Discussion
The results of the present study revealed that mild thrombocytopenia (≥ 100 × 109/L and < 150 × 109/L) is not a risk factor for developing severe features of pre-eclampsia, including severe hypertension, maternal organ damage, and utero-placental dysfunction. Although physicians decide the timing of delivery in patients with pre-eclampsia based on GW and various clinical aspects in addition to PC counts, the rates of preterm delivery and NICU admission may be affected by the levels of PC counts, because thrombocytopenia is included as a sign of maternal organ damage. However, preterm delivery and NICU admission rates in patients with mild thrombocytopenia were not different from the rates in patients with normal PC. On the other hand, severe thrombocytopenia was a risk factor of developing maternal organ damage, except for thrombocytopenia. Although the rates of preterm delivery and NICU admission were higher in patients with severe thrombocytopenia than in patients with normal PC, the results might have been biased because severe thrombocytopenia is an indicator of pregnancy termination [1]. However, the onset of pre-eclampsia, which is not biased by PC levels, was earlier in patients with severe thrombocytopenia than in patients with normal PC. Early onset of pre-eclampsia is associated with worse outcomes in both mother and baby [8]. These findings support that PC levels ≥ 100 × 109/L and < 150 × 109/L does not reflect a sign of maternal organ damage in pre-eclampsia.
Gestational thrombocytopenia (GT) is defined as PC levels < 150 × 109/L, with the exclusion of other possible diagnoses [5]. GT occurs in 4.4–11.6 % of pregnancies and accounts for almost 75 % of thrombocytopenia in pregnancy [9,10,11]. Since there are no available biomarkers to provide a definite diagnosis of GT, some cases of thrombocytopenia detected in patients with HDP may not reflect the disease progression and may be a result of GT. In addition, only 1–5 % women with GT develop PC levels < 100 × 109/L, and GT does not usually affect perinatal outcomes [5]. Therefore, this could explain why mild thrombocytopenia was not associated with worse perinatal outcomes in our study, as thrombocytopenia was not caused by pre-eclampsia.
Blood coagulation disorders, including thrombocytopenia, are a sign of maternal organ damage; therefore, patients with thrombocytopenia are considered as severe pre-eclampsia even with blood pressure levels < 160/110 mmHg and no other signs of maternal organ damage [1, 2]. If the majority of cases of mild thrombocytopenia are not associated with worse maternal and neonatal outcomes, using PC levels < 150 × 109/L as a cut-off value of a sign of maternal organ damage may increase unnecessary hospitalization and iatrogenic preterm delivery, particularly after 34 GW.
Pre-eclampsia is a progressive disease and PC levels may decrease as the disease progresses. Our findings indicate that mild thrombocytopenia is not a severe feature of pre-eclampsia; however, PC levels may decrease in patients with mild thrombocytopenia as pre-eclampsia progresses and become severe thrombocytopenia. Evaluation of the speed of PC decrease and the rate of PC decrease from the baseline will give further information to predict the deterioration of pre-eclampsia. Previous studies have reported that platelet indices, such as mean platelet volume and platelet distribution width, were associated with pre-eclampsia development and severity [12,13,14]. Analysis of platelet indices in addition to PC may help identify patients with mild thrombocytopenia in which PC levels will progressively decrease.
In Japan, thrombocytopenia was not included in the criteria of diagnosis and severity of pre-eclampsia until May 2018. The protocol for HDP patient management in Hokkaido University Hospital and Japan Community Health Care Organization Hokkaido Hospital was not changed after the Japanese criteria revision. Therefore, clinicians’ decisions would not have been affected the discrepancy in PC cut-off value in the present study.
This study has several limitations. This was a retrospective study; therefore, the timing of termination was decided based on the clinical decisions of the doctors in each hospital. Although serum biomarkers, such as the ratio of soluble fms-like tyrosine kinase to placental growth factor, are associated with development of pre-eclampsia [15], they were not widely available in Japan during the study period. Thus, we were unable to examine the association between mild thrombocytopenia and those biomarkers. Finally, low-dose aspirin is useful for prevention of pre-eclampsia in high-risk patients [16]. However, the rate of low-dose aspirin usage was very low in our study. Therefore, it is difficult to determine whether our findings are adaptable for patients using low-dose aspirin.
Conclusion
.
Despite these limitations, this study implies that mild thrombocytopenia in pre-eclampsia is not related with severe features of pre-eclampsia, and would not be suitable as a sign of maternal organ damage in patients with pre-eclampsia. PC levels < 100 × 109/L may be better cut-off value as a sign of maternal organ damage in pre-eclampsia.
Availability of data and materials
The datasets used and/or analysed during the current study will be available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- GT:
-
Gestational thrombocytopenia
- GW:
-
Gestational weeks
- HDP:
-
Hypertensive disorders of pregnancy
- NICU:
-
Neonatal intensive care unit
- eRR:
-
Estimated relative risk
- PC:
-
Platelet count
References
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–31.
Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy: ISSHP Classification, Diagnosis, and Management Recommendations for International Practice. Hypertension. 2018;72:24–43.
Juan P, Stefano G, Antonella S, Albana C. Platelets in pregnancy. J Prenat Med. 2011;5:90–2.
Thalor N, Singh K, Pujani M, Chauhan V, Agarwal C, Ahuja R. A correlation between platelet indices and pre-eclampsia. Hematol Transfus Cell Ther. 2019;41:129–33.
Cines DB, Levine LD. Thrombocytopenia in pregnancy. Blood. 2017;130:2271–7.
Mayama M, Morikawa M, Umazume T, Nakagawa K, Hosokawa A, Yamaguchi M, et al. Increase in the number of patients diagnosed using the new classification of hypertensive disorders of pregnancy in Japan. J Obstet Gynaecol Res. 2019;45:1118–26.
McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies ad clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–3.
Khodzhaeva ZS, Kogan YA, Shmakov RG, Klimenchenko NI, Akatyeva AS, Vavina OV. et al. Clinical and pathogenetic features of early- and late-onset pre-eclampsia. J Matern Fetal Neonatal Med. 2016;29:2980-6.
Practice bulletin no. 166: thrombocytopenia in pregnancy. Obstet Gynecol. 2016;128:e43–53.
Burrows RF, Kelton JG. Thrombocytopenia at delivery: A prospective survey of 6715 deliveries. Am J Obstet Gynecol. 1990;162:731–4.
Gernsheimer T, James AH, Stasi R. How I treat thrombocytopenia in pregnancy. Blood. 2013;121:38–47.
Freitas LG, Alpoim PN, Komatsuzaki F, Carvalho Md, Dusse LM. Pre-eclampsia: are platelet count and indices useful for its prognostic? Hematology. 2013;18:360–4.
Yang SW, Cho SH, Kwon HS, Sohn IS, Hwang HS. Significance of the platelet distribution width as a severity marker for the development of pre-eclampsia. Eur J Obstet Gynecol Reprod Biol. 2014;175:107–11.
AlSheeha MA, Alaboudi RS, Alghasham MA, Iqbal J, Adam I. Platelet count and platelet indices in women with pre-eclampsia. Vasc Health Risk Manag. 2016;12:477–80.
Zeisler H, Llurba E, Chantraine F, Vatish M, Staff AC, Sennström M. et al. Predictive value of the sFlt-1:PlGF ratio in women with suspected pre-eclampsia. N Engl J Med. 2016;374:13–22.
Rolnik DL, Wright D, Poon LC, O’Gorman N, Syngelaki A. et al. Aspirin versus placebo in pregnancies at high risk for preterm pre-eclampsia. N Engl J Med. 2017;377:613 – 22., de Paco Matallana C.
Acknowledgements
The authors would like to thank Enago (https://www.enago.jp) for the English language review.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All listed authors meet criteria for authorship. MM1 made substantial contributions to conceptualization, design of the work, and drafting the work. MM2 made substantial contributions to conceptualization, the acquisition, and the analysis. TY and TU made substantial contributions to interpretation of data. KN1 and KN2 made substantial contributions to the acquisition, and the analysis. YS and KC made substantial contributions to design of work. SK and HW made substantial contributions to drafting and revising work. All authors approved the submitted version, and agreed to be personally accountable for their contributions to the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of Hokkaido University Hospital (019–0070) and Japan Community Health Care Organization Hokkaido Hospital (2020-4). The committees did not require informed consent for this retrospective study. We put information of this study on Hokkaido University’s and Japan Community Health Care Organization Hokkaido Hospital’s home page with the opportunity to opt out.
Consent for publication
Not required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mayama, M., Morikawa, M., Yamada, T. et al. Mild thrombocytopenia indicating maternal organ damage in pre‐eclampsia: a cross‐sectional study. BMC Pregnancy Childbirth 21, 91 (2021). https://doi.org/10.1186/s12884-021-03564-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-021-03564-4