Abstract
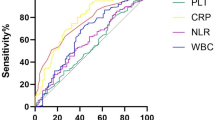
Systemic inflammatory response is closely related to the pathogenesis and prognosis in critical patients. Recently, systemic immune-inflammation index (SII), an indicator of systemic inflammatory response, was proved to predict the outcome in cancerous and non-cancerous diseases. The aim of this study is to investigate the association between SII on admission and 6-month outcome in patients with aneurysmal subarachnoid hemorrhage (aSAH). The clinical data and prognosis of 76 patients with aSAH were analyzed. The 6-month outcome was assessed by the modified Rankin scale(mRS). The unfavorable outcome was defined as mRS score ≥ 3. In addition, multivariate analysis was conducted to investigate factors independently associated with the favorable outcome. Receiver operating characteristic (ROC) curve analysis was undertaken to identify the best cut-off value of SII for the discriminate between favorable and unfavorable outcome in these patients. Thirty-six patients (47.4%) in our study had an unfavorable outcome (mRS ≥ 3) at 6 months, and twenty-four (66.7%) of them were in the high-SII group. A significantly higher SII on admission was observed in patients with unfavorable functional outcome at 6 months. Binary logistic regression analysis showed that there was an independent association between SII on admission and 6-month clinical outcome (adjusted OR = 4.499, 95%CI: 1.242–16.295, P < 0.05). The AUC of the SII for predicting unfavorable outcome was 0.692 (95% CI: 0.571–0.814, P < 0.05). Systemic immune-inflammation index (SII) could be a novel independent prognostic factor for aSAH patients at the early stage of the disease.


Similar content being viewed by others
Data availability
The data used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- AUC:
-
Area under the curve
- ANC:
-
Absolute neutrophil counts
- ALC:
-
Absolute lymphocyte counts
- CT:
-
Computerized tomography
- CTA:
-
Computerized tomography angiography
- CNS:
-
Central nervous system
- CI:
-
Confidence interval
- DND:
-
Delayed neurological dysfunction
- DSA:
-
Digital subtraction angiography
- H–H grade:
-
Hunt and Hess grade
- IA:
-
Intracranial aneurysm
- mRS:
-
Modified Rankin scale
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OR:
-
Odds ratios
- PLR:
-
Platelet-to-lymphocyte ratio
- PNI:
-
Prognostic nutrition index
- PLT:
-
Platelet
- PLC:
-
Platelet counts
- ROC:
-
Receiver operating characteristics
- SII:
-
Systemic immune-inflammation index
- SD:
-
Standard deviation
- WBC:
-
White blood cells
- WFNS grade:
-
World Federation of Neurosurgical Societies grade
References
Al-Mufti F, Amuluru K, Damodara N et al (2019) Admission neutrophil-lymphocyte ratio predicts delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. J Neurointerv Surg 11(11):1135–1140. https://doi.org/10.1136/neurintsurg-2019-014759
Al-Mufti F, Misiolek K, Roh D et al (2019) White blood cell count improves prediction of delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Neurosurgery 84(2):397–403. https://doi.org/10.1093/neuros/nyy045
Aronowski J, Zhao X (2011) Molecular pathophysiology of cerebral hemorrhage: secondary brain injury. Stroke 42(6):1781–1786. https://doi.org/10.1161/strokeaha.110.596718
Broderick J, Brott T, Duldner J, Tomsick T, Leach AJS (1994) Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke 25(7):1342–1347. https://doi.org/10.1161/01.str.25.7.1342
Budohoski K, Guilfoyle M, Helmy A et al (2014) The pathophysiology and treatment of delayed cerebral ischaemia following subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 85(12):1343–1353. https://doi.org/10.1136/jnnp-2014-307711
Chou S, Feske S, Atherton J et al (2012) Early elevation of serum tumor necrosis factor-α is associated with poor outcome in subarachnoid hemorrhage. J Investig Med 60(7):1054–1058. https://doi.org/10.2310/JIM.0b013e3182686932
Chou S, Feske S, Simmons S et al (2011) Elevated peripheral neutrophils and matrix metalloproteinase 9 as biomarkers of functional outcome following subarachnoid hemorrhage. Transl Stroke Res 2(4):600–607. https://doi.org/10.1007/s12975-011-0117-x
Fassbender K, Hodapp B, Rossol S et al (2001) Inflammatory cytokines in subarachnoid haemorrhage: association with abnormal blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry 70(4):534–537. https://doi.org/10.1136/jnnp.70.4.534
Frontera JA, Provencio JJ, Sehba FA et al (2017) The role of platelet activation and inflammation in early brain injury following subarachnoid hemorrhage. Neurocrit Care 26(1):48–57. https://doi.org/10.1007/s12028-016-0292-4
Fujii M, Yan J, Rolland W et al (2013) Early brain injury, an evolving frontier in subarachnoid hemorrhage research. Transl Stroke Res 4(4):432–446. https://doi.org/10.1007/s12975-013-0257-2
Geng Y, Shao Y, Zhu D, et al (2016) Systemic immune-inflammation index predicts prognosis of patients with esophageal squamous cell carcinoma: a propensity score-matched analysis. Scientific reports 6(39482). https://doi.org/10.1038/srep39482
Geraghty J, Testai FJCar (2017) Delayed cerebral ischemia after subarachnoid hemorrhage: beyond vasospasm and towards a multifactorial pathophysiology. Curr Atheroscler Rep 19(12):50 https://doi.org/10.1007/s11883-017-0690-x
Ghali M, Srinivasan V, Johnson J et al (2018) Therapeutically targeting platelet-derived growth factor-mediated signaling underlying the pathogenesis of subarachnoid hemorrhage-related vasospasm. J Stroke Cerebrovas Dis Official J Nat Stroke Assoc 27(9):2289–2295. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.02.017
Gomes Dos Santos A, de Carvalho R, de Morais A, et al (2021) Role of neutrophil-lymphocyte ratio as a predictive factor of glioma tumor grade: a systematic review. Crit Rev Oncol Hematol 163(103372) https://doi.org/10.1016/j.critrevonc.2021.103372
Hou D, Wang C, Luo Y, et al. (2020) Systemic immune-inflammation index (sii) but not platelet-albumin-bilirubin (palbi) grade is associated with severity of acute ischemic stroke (ais). Int J Neurosci:1–6 https://doi.org/10.1080/00207454.2020.1784166
Hu B, Yang X, Xu Y et al (2014) Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res Official J Am Assoc Cancer Res 20(23):6212–6222. https://doi.org/10.1158/1078-0432.Ccr-14-0442
Jabbarli R, Pierscianek D, Darkwah Oppong M et al (2020) Laboratory biomarkers of delayed cerebral ischemia after subarachnoid hemorrhage: a systematic review. Neurosurg Rev 43(3):825–833. https://doi.org/10.1007/s10143-018-1037-y
Jomrich G, Paireder M, Kristo I et al (2021) High systemic immune-inflammation index is an adverse prognostic factor for patients with gastroesophageal adenocarcinoma. Ann Surg Oncol 273(3):532–541. https://doi.org/10.1097/sla.0000000000003370
Kasius K, Frijns C, Algra A, Rinkel GJCd (2010) Association of platelet and leukocyte counts with delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. Cerebrovasc Dis 29(6):576–583. https://doi.org/10.1159/000306645
Lattanzi S, Brigo F, Trinka E et al (2019) Neutrophil-to-lymphocyte ratio in acute cerebral hemorrhage: a system review. Transl Stroke Res 10(2):137–145. https://doi.org/10.1007/s12975-018-0649-4
Li P, Mao L, Liu X et al (2014) Essential role of program death 1-ligand 1 in regulatory t-cell-afforded protection against blood-brain barrier damage after stroke. Stroke 45(3):857–864. https://doi.org/10.1161/strokeaha.113.004100
Liang R, Chen N, Li M et al (2018) Significance of systemic immune-inflammation index in the differential diagnosis of high- and low-grade gliomas. Clin Neurol Neurosurg 164:50–52. https://doi.org/10.1016/j.clineuro.2017.11.011
Liang R, Li J, Tang X, Liu Y (2019) The prognostic role of preoperative systemic immune-inflammation index and albumin/globulin ratio in patients with newly diagnosed high-grade glioma. Clin Neurol Neurosurg 184(105397) https://doi.org/10.1016/j.clineuro.2019.105397
Lucke-Wold B, Logsdon A, Manoranjan B et al (2016) Aneurysmal subarachnoid hemorrhage and neuroinflammation: a comprehensive review. Int J Mol Sci 17(4):497. https://doi.org/10.3390/ijms17040497
Macdonald RL, Schweizer TA (2017) Spontaneous subarachnoid haemorrhage. Lancet (London, England) 389(10069):655–666. https://doi.org/10.1016/s0140-6736(16)30668-7
McMahon C, Hopkins S, Vail A et al (2013) Inflammation as a predictor for delayed cerebral ischemia after aneurysmal subarachnoid haemorrhage. J Neurointerv Surg 5(6):512–517. https://doi.org/10.1136/neurintsurg-2012-010386
Nóbrega Lima Rodrigues de Morais A, Ribeiro Baylão VM, Martins Silva T, et al (2021) Is neutrophil-lymphocyte ratio a useful tool for predicting outcome in subarachnoid hemorrhage? A systematic review. Neurosurg Rev https://doi.org/10.1007/s10143-021-01484-7
Olsen MH, Lilja-Cyron A, Bache S, Eskesen V, Møller K (2019) [Aneurysmal subarachnoid haemorrhage]. Ugeskrift for laeger 181(31)
Saand A, Yu F, Chen J et al (2019) Systemic inflammation in hemorrhagic strokes - a novel neurological sign and therapeutic target? J Cereb Blood Flow Metab 39(6):959–988. https://doi.org/10.1177/0271678x19841443
Sarrafzadeh A, Schlenk F, Meisel A et al (2011) Immunodepression after aneurysmal subarachnoid hemorrhage. Stroke 42(1):53–58. https://doi.org/10.1161/strokeaha.110.594705
Srinivasan A, Aggarwal A, Gaudihalli S et al (2016) Impact of early leukocytosis and elevated high-sensitivity c-reactive protein on delayed cerebral ischemia and neurologic outcome after subarachnoid hemorrhage. World Neurosurg 90:91–95. https://doi.org/10.1016/j.wneu.2016.02.049
Swirski F, Nahrendorf MJS (2013) Leukocyte behavior in atherosclerosis, myocardial infarction, and heart failure. Science (New York, NY) 339(6116):161–166. https://doi.org/10.1126/science.1230719
Tao C, Wang J, Hu X et al (2017) Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage. Neurocrit Care 26(3):393–401. https://doi.org/10.1007/s12028-016-0332-0
Terpolilli N, Brem C, Bühler D, Plesnila NJS (2015) Are we barking up the wrong vessels? Cereb Microcircul After Subarach Hemorrh Stroke 46(10):3014–3019. https://doi.org/10.1161/strokeaha.115.006353
Trifan G, Testai FD (2020) Systemic immune-inflammation (sii) index predicts poor outcome after spontaneous supratentorial intracerebral hemorrhage. J Stroke Cerebrovasc Dis Official J Nat Stroke Assoc 29(9):105057. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105057
van der Willik KD, Fani L, Rizopoulos D et al (2019) Balance between innate versus adaptive immune system and the risk of dementia: a population-based cohort study. J Neuroinflammation 16(1):68. https://doi.org/10.1186/s12974-019-1454-z
Vogelgesang A, Grunwald U, Langner S et al (2008) Analysis of lymphocyte subsets in patients with stroke and their influence on infection after stroke. Stroke 39(1):237–241. https://doi.org/10.1161/strokeaha.107.493635
Wu Y, He Q, Wei Y et al (2019) The association of neutrophil-to-lymphocyte ratio and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: possible involvement of cerebral blood perfusion. Neuropsychiat Dis Treatment 15:1001–1007. https://doi.org/10.2147/ndt.S190477
Xu W, Wang D, Zheng X, Ou Q, Huang L (2018) Sex-dependent association of preoperative hematologic markers with glioma grade and progression. J Neurooncol 137(2):279–287. https://doi.org/10.1007/s11060-017-2714-3
Funding
This work was supported by the Kuanren Talents Program of the Second Affiliated Hospital of Chongqing Medical University (No. 201959), Chongqing Science and Health Joint Project (No. 2020GDRC006), and Venture and Innovation Support Program for Chongqing Overseas Returnees (No. CX2019156).
Author information
Authors and Affiliations
Contributions
Author contributions to the study and manuscript preparation include the following: Conception and design: Fushu Luo, Yuanyou Li, Zongyi Xie. Acquisition of data: Yuanyou Li, Mingjiang Sun. Analysis and interpretation of data: Fushu Luo, Yuanyou Li, Yuantong Zhao. Drafting the article: Fushu Luo, Yuanyou Li. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript for publication on behalf of all authors: Zongyi Xie. Study supervision: Zongyi Xie.
Corresponding author
Ethics declarations
Ethics approval
This study has been approved by the Ethics Committee of the Second Affiliated Hospital of Chongqing Medical University (No.34).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, F., Li, Y., Zhao, Y. et al. Systemic immune-inflammation index predicts the outcome after aneurysmal subarachnoid hemorrhage. Neurosurg Rev 45, 1607–1615 (2022). https://doi.org/10.1007/s10143-021-01681-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01681-4