Abstract
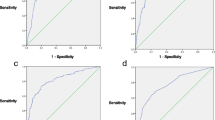
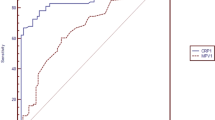
Neonatal early-onset sepsis (EOS) is associated with high morbidity and mortality. Accurate early diagnosis is crucial for prompt treatment and a better clinical outcome. We aimed to identify new biomarkers for the diagnosis of EOS. A total of 152 neonates with a risk of EOS were divided into an EOS group and a non-EOS group according to the conventional diagnostic criteria. Blood samples were collected within 0–24, 24–48, and 48–72 h after birth. Serum levels of progranulin (PGRN), interleukin (IL)-33, IL-17a, IL-23, IL-6, tumor necrosis factors α (TNF-α), interferon γ (IFN-γ), granulocyte-macrophage colony-stimulating factor (GM-CSF), procalcitonin (PCT), and C-reactive protein (CRP) were determined. PGRN levels were significantly elevated in the EOS neonates compared with the levels in the non-EOS neonates (1.53 vs. 0.77 ng/ml (median), P < 0.001), with an area under the receiver operating characteristic (ROC) curve (AUC) of 0.76 (P < 0.001). Compared with PGRN, IL-33, IL-17a, IL-23, IL-6, PCT, and CRP showed significant (AUC > 0.70) but slightly less predictive power for EOS within the same time range. Stepwise multivariate regression analysis identified PGRN, IL-33, and PCT as independent predictors of EOS. In addition, the combined measurements of PGRN, IL-33, and PCT showed significantly higher predictive power for EOS than any of the three markers alone. PGRN showed greater efficacy for predicting EOS than the traditional markers PCT and CRP as well as other potential markers tested in this study. PGRN may serve as an effective biomarker for the early diagnosis of EOS.



Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EOS:
-
early-onset sepsis
- PGRN:
-
progranulin
- IL-33:
-
interleukin 33
- IL-17a:
-
interleukin 17a
- IL-23:
-
interleukin 23
- IL-6:
-
interleukin 6
- TNF-α:
-
tumor necrosis factors α
- IFN-γ:
-
interferon γ
- GM-CSF:
-
granulocyte-macrophage colony-stimulating factor
- PCT:
-
procalcitonin
- CRP:
-
C-reactive protein
- AUC:
-
area under the curve
- CI:
-
confidence interval
References
Pierrakos C, Vincent JL (2010) Sepsis biomarkers: a review. Crit Care 14:R15. https://doi.org/10.1186/cc8872
Clark RH, Bloom BT, Spitzer AR, Gerstmann DR (2006) Empiric use of ampicillin and cefotaxime, compared with ampicillin and gentamicin, for neonates at risk for sepsis is associated with an increased risk of neonatal death. Pediatrics 117:67–74. https://doi.org/10.1542/peds.2005-0179
Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK Jr (2006) The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics 118:717–722. https://doi.org/10.1542/peds.2005-2677
Manzoni P, Mostert M, Galletto P, Gastaldo L, Gallo E, Agriesti G, Farina D (2009) Is thrombocytopenia suggestive of organism-specific response in neonatal sepsis? Pediatr Int 51:206–210. https://doi.org/10.1111/j.1442-200X.2008.02689.x
Chauhan N, Tiwari S, Jain U (2017) Potential biomarkers for effective screening of neonatal sepsis infections: an overview. Microb Pathog 107:234–242. https://doi.org/10.1016/j.micpath.2017.03.042
Gibot S, Bene MC, Noel R, Massin F, Guy J, Cravoisy A, Barraud D, De Carvalho BM, Quenot JP, Bollaert PE, Faure G, Charles PE (2012) Combination biomarkers to diagnose sepsis in the critically ill patient. Am J Respir Crit Care Med 186:65–71. https://doi.org/10.1164/rccm.201201-0037OC
Vouloumanou EK, Plessa E, Karageorgopoulos DE, Mantadakis E, Falagas ME (2011) Serum procalcitonin as a diagnostic marker for neonatal sepsis: a systematic review and meta-analysis. Intensive Care Med 37:747–762. https://doi.org/10.1007/s00134-011-2174-8
Yu Z, Liu J, Sun Q, Qiu Y, Han S, Guo X (2010) The accuracy of the procalcitonin test for the diagnosis of neonatal sepsis: a meta-analysis. Scand J Infect Dis 42:723–733. https://doi.org/10.3109/00365548.2010.489906
Jekarl DW, Kim JY, Lee S, Kim M, Kim Y, Han K, Woo SH, Lee WJ (2015) Diagnosis and evaluation of severity of sepsis via the use of biomarkers and profiles of 13 cytokines: a multiplex analysis. Clin Chem Lab Med 53:575–581. https://doi.org/10.1515/cclm-2014-0607
Jian J, Konopka J, Liu C (2013) Insights into the role of progranulin in immunity, infection, and inflammation. J Leukoc Biol 93:199–208. https://doi.org/10.1189/jlb.0812429
Song Z, Zhang X, Zhang L, Xu F, Tao X, Zhang H, Lin X, Kang L, Xiang Y, Lai X, Zhang Q, Huang K, Dai Y, Yin Y, Cao J (2016) Progranulin plays a central role in host defense during sepsis by promoting macrophage recruitment. Am J Respir Crit Care Med 194:1219–1232. https://doi.org/10.1164/rccm.201601-0056OC
Ince Z (2014) Diagnosis of neonatal sepsis: what the clinician expects, what the laboratory tells. Clin Biochem 47:754–755. https://doi.org/10.1016/j.clinbiochem.2014.05.045
Cuenca AG, Wynn JL, Moldawer LL, Levy O (2013) Role of innate immunity in neonatal infection. Am J Perinatol 30:105–112. https://doi.org/10.1055/s-0032-1333412
Kurt AN, Aygun AD, Godekmerdan A, Kurt A, Dogan Y, Yilmaz E (2007) Serum IL-1beta, IL-6, IL-8, and TNF-alpha levels in early diagnosis and management of neonatal sepsis. Mediators Inflamm 2007:31397. https://doi.org/10.1155/2007/31397
Martin H, Olander B, Norman M (2001) Reactive hyperemia and interleukin 6, interleukin 8, and tumor necrosis factor-alpha in the diagnosis of early-onset neonatal sepsis. Pediatrics 108:E61. https://doi.org/10.1542/peds.108.4.e61
Verani JR, McGee L, Schrag SJ (2010) Prevention of perinatal group B streptococcal disease--revised guidelines from CDC, 2010. MMWR Recomm Rep 59:1–36
Schlapbach LJ, Graf R, Woerner A, Fontana M, Zimmermann-Baer U, Glauser D, Giannoni E, Roger T, Muller C, Nelle M, Stocker M (2013) Pancreatic stone protein as a novel marker for neonatal sepsis. Intensive Care Med 39:754–763. https://doi.org/10.1007/s00134-012-2798-3
Turner D, Hammerman C, Rudensky B, Schlesinger Y, Goia C, Schimmel MS (2006) Procalcitonin in preterm infants during the first few days of life: introducing an age related nomogram. Arch Dis Child Fetal Neonatal Ed 91:F283–F286. https://doi.org/10.1136/adc.2005.085449
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161. https://doi.org/10.1016/s0140-6736(12)60560-1
Fattah MA, Omer AF, Asaif S, Manlulu R, Karar T, Ahmed A, Aljada A, Saleh AM, Qureshi S, Nasr A (2017) Utility of cytokine, adhesion molecule and acute phase proteins in early diagnosis of neonatal sepsis. J Nat Sci Biol Med 8:32–39. https://doi.org/10.4103/0976-9668.198362
Li S, Zhu FX, Zhao XJ, An YZ (2016) The immunoprotective activity of interleukin-33 in mouse model of cecal ligation and puncture-induced sepsis. Immunol Lett 169:1–7. https://doi.org/10.1016/j.imlet.2015.11.009
Alves-Filho JC, Sonego F, Souto FO, Freitas A, Verri WA Jr, Auxiliadora-Martins M, Basile-Filho A, McKenzie AN, Xu D, Cunha FQ, Liew FY (2010) Interleukin-33 attenuates sepsis by enhancing neutrophil influx to the site of infection. Nat Med 16:708–712. https://doi.org/10.1038/nm.2156
Li J, Zhang Y, Lou J, Zhu J, He M, Deng X, Cai Z (2012) Neutralisation of peritoneal IL-17A markedly improves the prognosis of severe septic mice by decreasing neutrophil infiltration and proinflammatory cytokines. PLoS One 7:e46506. https://doi.org/10.1371/journal.pone.0046506
Cauvi DM, Williams MR, Bermudez JA, Armijo G, De Maio A (2014) Elevated expression of IL-23/IL-17 pathway-related mediators correlates with exacerbation of pulmonary inflammation during polymicrobial sepsis. Shock 42:246–255. https://doi.org/10.1097/shk.0000000000000207
Miguel-Bayarri V, Casanoves-Laparra EB, Pallas-Beneyto L, Sancho-Chinesta S, Martin-Osorio LF, Tormo-Calandin C, Bautista-Rentero D (2012) Prognostic value of the biomarkers procalcitonin, interleukin-6 and C-reactive protein in severe sepsis. Med Intensiva 36:556–562. https://doi.org/10.1016/j.medin.2012.01.014
Franco DM, Arevalo-Rodriguez I, Figuls MR (2015) Interleukin-6 for diagnosis of sepsis in critically ill adult patients [M]. John Wiley & Sons, Ltd
Berner R, Niemeyer CM, Leititis JU, Funke A, Schwab C, Rau U, Richter K, Tawfeek MS, Clad A, Brandis M (1998) Plasma levels and gene expression of granulocyte colony-stimulating factor, tumor necrosis factor-alpha, interleukin (IL)-1beta, IL-6, IL-8, and soluble intercellular adhesion molecule-1 in neonatal early onset sepsis. Pediatr Res 44:469–477. https://doi.org/10.1203/00006450-199810000-00002
Ng PC, Cheng SH, Chui KM, Fok TF, Wong MY, Wong W, Wong RP, Cheung KL (1997) Diagnosis of late onset neonatal sepsis with cytokines, adhesion molecule, and C-reactive protein in preterm very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 77:F221–F227. https://doi.org/10.1136/fn.77.3.f221
Payen D, Faivre V, Miatello J, Leentjens J, Brumpt C, Tissieres P, Dupuis C, Pickkers P, Lukaszewicz AC (2019) Multicentric experience with interferon gamma therapy in sepsis induced immunosuppression. A case series. BMC Infect Dis 19:931. https://doi.org/10.1186/s12879-019-4526-x
Mathias B, Szpila BE, Moore FA, Efron PA, Moldawer LL (2015) A review of GM-CSF therapy in sepsis. Medicine (Baltimore) 94:e2044. https://doi.org/10.1097/md.0000000000002044
Makhoul IR, Yacoub A, Smolkin T, Sujov P, Kassis I, Sprecher H (2006) Values of C-reactive protein, procalcitonin, and Staphylococcus-specific PCR in neonatal late-onset sepsis. Acta Paediatr 95:1218–1223. https://doi.org/10.1080/08035250600554250
Chiesa C, Natale F, Pascone R, Osborn JF, Pacifico L, Bonci E, De Curtis M (2011) C reactive protein and procalcitonin: reference intervals for preterm and term newborns during the early neonatal period. Clin Chim Acta 412:1053–1059. https://doi.org/10.1016/j.cca.2011.02.020
Yang AP, Liu J, Yue LH, Wang HQ, Yang WJ, Yang GH (2016) Neutrophil CD64 combined with PCT, CRP and WBC improves the sensitivity for the early diagnosis of neonatal sepsis. Clin Chem Lab Med 54:345–351. https://doi.org/10.1515/cclm-2015-0277
Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, Bohuon C (1994) Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab 79:1605–1608. https://doi.org/10.1210/jcem.79.6.7989463
Hedegaard SS, Wisborg K, Hvas AM (2015) Diagnostic utility of biomarkers for neonatal sepsis--a systematic review. Infect Dis (Lond) 47:117–124. https://doi.org/10.3109/00365548.2014.971053
Ismail AQ, Gandhi A (2015) Using CRP in neonatal practice. J Matern Fetal Neonatal Med 28:3–6. https://doi.org/10.3109/14767058.2014.885499
Hofer N, Zacharias E, Muller W, Resch B (2012) An update on the use of C-reactive protein in early-onset neonatal sepsis: current insights and new tasks. Neonatology 102:25–36. https://doi.org/10.1159/000336629
Benitz WE (2010) Adjunct laboratory tests in the diagnosis of early-onset neonatal sepsis. Clin Perinatol 37:421–438. https://doi.org/10.1016/j.clp.2009.12.001
Memar MY, Alizadeh N, Varshochi M, Kafil HS (2019) Immunologic biomarkers for diagnostic of early-onset neonatal sepsis. J Matern Fetal Neonatal Med 32:143–153. https://doi.org/10.1080/14767058.2017.1366984
Funding
This study was supported by the National Natural Science Foundation of China (Grant Nos. 81571483 and 81971431) and Shenzhen Science and Technology Innovation Free Exploration Project (JCYJ20170817100735621).
Author information
Authors and Affiliations
Contributions
KY, YH, and JY contributed to the conception of the study. KY contributed significantly to analysis and manuscript preparation; KY performed the data analyses and wrote the manuscript; SX, QA, and JY helped perform the analysis with constructive discussions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University (2015-115).
Consent to participate
The consent to participate had been obtained from all the legal guardian of the patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, KD., He, Y., Xiao, S. et al. Identification of progranulin as a novel diagnostic biomarker for early-onset sepsis in neonates. Eur J Clin Microbiol Infect Dis 39, 2405–2414 (2020). https://doi.org/10.1007/s10096-020-03981-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-020-03981-x